
IDENTIFYING THE CARDIAC REGION IN IMAGES
OF ELECTRICAL IMPEDANCE TOMOGRAPHY
THROUGH WAVELET TRANSFORM
José Pedro de Oliveira, Harki Tanaaka and Neli Regina Siqueira Ortega
School of Medicine, University of São Paulo, LIM01/HCFMUSP, Brazil
Keywords: Electrical Impedance Tomography, Medical decision support system, Wavelet transform.
Abstract: Electrical Impedance Tomography (EIT) is an imaging technique, still in development, in which an image
of the conductivity of part of the body is inferred from surface electrical measurements. Despite the
benefits, its resulting image still does not offer a good spatial resolution. In EIT images of the thorax the
largest challenge is the treatment of the lung perfusion, especially in the identification of the cardiac region.
The current EIT equipments, used in the treatment of ICU (Intensive care unit) patients with respiratory
complications, have a need to better define the cardiac region in dynamic EIT images, in order to
offer a better system of support to the medical decision. In an attempt to overcome this problem,
Tanaka and collaborators proposed a methodology using the theory of fuzzy sets. Fuzzy logic
approach allowed a more appropriated treatment of the uncertainty in identifying the pixel as
belonging to a pulmonary or cardiac region. However, this fuzzy model presented some
limitations when submitted to different clinical conditions, such as PEEP variation. In this work
we present a methodology based on wavelet transform for analysis of the EIT signals of the
pulmonary perfusion obtained in an animal experiment.
1 INTRODUCTION
Electrical Impedance Tomography (EIT) is an
imaging technique, still in development, in which an
image of the conductivity of a transversal section of
an object is inferred from electrical measurements
done in a series of electrodes placed on its surface.
Despite the benefits presented by this technique, it
has some limitations, amongst which we detach the
low spatial resolution. Although the EIT method
presents a high time resolution, the low spatial
resolution hinders the characterization of the activity
of regions according to their physiological origin in
a dynamic image. One of the most important EIT
studies concerns to the images of the thorax, aiming
the monitoring the cardio-respiratory functions. In
that sense, Tanaka et al. proposed the use of the
theory of fuzzy sets to deal with the uncertainty of
identification of the pixels, aiming a segmented
image containing the cardiac and pulmonary regions
(Tanaka et al, 2008). Despite the good results, this
model presented some limitations in identifying the
heart in more complex situations. Therefore, it is
realized that a tool that could extract more
information from EIT signal could be capable to
separate with more clearness the pulmonary and
cardiac regions. One of the tools capable to extract
information of signals in the time and frequency
domains, with possibilities to minimize this
limitation, is the Wavelet Transform.
Wavelet transform emerged as a result of
developments in this type of representation of
signals. Basically, there are three classes of wavelet
transforms: the Continuous Wavelet Transform
(CWT), the Semi-Discrete Wavelet Transform
(SWT) and the Discrete Wavelet Transform (DWT)
(Polikar, 1999). The DWT is a multi-resolution
representation of the original signal and is
particularly useful for noise reduction and data
compression, whereas the CWT is better for feature
extraction purposes. The SWT is simply a
discretization of the CWT in order that this can be
processed by computers and digital equipments.
A typical EIT system has the following
components: a set of current injection electrodes; a
system of measure of electric potentials between the
electrodes; and an algorithm of image reconstruction
(Adler et al, 1997). Among the benefits offered by
this technique, we detach: it is a noninvasive
technique; it presents a high temporal resolution; the
380
Oliveira J., Tanaaka H. and Ortega N. (2009).
IDENTIFYING THE CARDIAC REGION IN IMAGES OF ELECTRICAL IMPEDANCE TOMOGRAPHY THROUGH WAVELET TRANSFORM.
In Proceedings of the International Conference on Knowledge Engineering and Ontology Development, pages 380-383
DOI: 10.5220/0002277203800383
Copyright
c
SciTePress
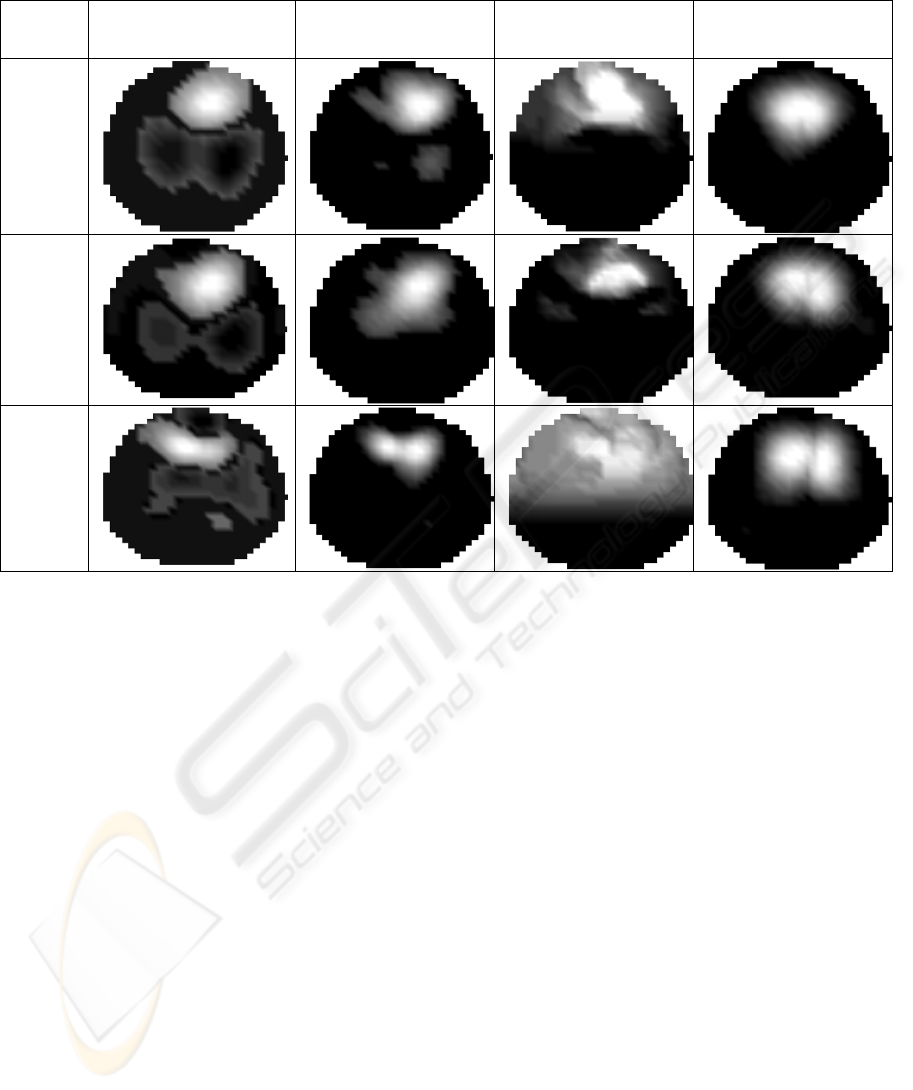
Table 1: Heart maps provided by the systems for each PEEP values: a) the wavelet analysis; b) the fuzzy approach; and c)
the saline injection.
PEEP WaveletAlgorithm 1 WaveletAlgorithm 2 Fuzzy Saline
18
cm
H2O
12
cm
H2O
0
cm
H2O
(ZEEP)
equipments are cheap, relatively small and can be
installed at the bedside of the patient. As for its
limitations, we can point the low spatial resolution
and the relationship between the differences of
electrical potential measures on the surface and the
internal parameters of the object in analysis is not
linear, which difficult the development of the image
reconstruction algorithm (Tanaka et al, 2008;
Brown, 2003; Noor, 2007).
2 MATERIALS AND METHODS
The image generated by the EIT system used is
formed by 1024 pixels, where each pixel
corresponds to a certain area of the body of the
object under analysis. These pixels have variations
in their impedances due to the flow of blood during
the cardiac cycle. In order to develop a methodology
able of identifying the heart region in EIT images of
a thorax, it is necessary a qualitative analysis of the
information contained in these signals. Firstly, this
qualitative analysis was based on the wave patterns
and after each pattern was discussed with a panel of
experts, taking into account the physiological
knowledge about the cardio-respiratory dynamic.
This analysis was the fundamental importance in the
model development, because it provided the
standard behavior for each region of chest (lungs,
ventricle, atrium, aorta, etc.).
EIT raw data were collected in an animal
experiment (pig) by means of an electrical
impedance tomography, based on the Enlight ®
technology (DIXTAL, Brazil), which uses the image
reconstruction algorithm developed by Lima and
collaborators (Lima et al, 2005). EIT signal was
synchronized with the peak of the wave "R" of the
ECG signal. The pig was submitted to different
values of Positive End-Expiratory Pressure (PEEP):
18cmH2O (PEEP18), 12cmH2O (PEEP12) and
0cmH2O (ZEEP). This is important to evaluate the
robustness of the system developed in different
clinical conditions. For each one of these PEEPs was
done an experiment using a hypertonic solution
(20% NaCl), which serves as contrast to EIT images,
during apnea. The EIT images obtained by means of
this contrast allows localizing
the different
structures for where the flow passed. The objective
with the saline data is to establish a reference base,
so it will be possible to compare the results of the
IDENTIFYING THE CARDIAC REGION IN IMAGES OF ELECTRICAL IMPEDANCE TOMOGRAPHY THROUGH
WAVELET TRANSFORM
381

Table 2: ROC curves obtained for the wavelet and fuzzy approaches, compared with the heart region obtained through the
saline injection, for each PEEP values, where AUC means Area under of Curve.
THE ROC CURVES: __Wavelet ---Fuzzy
PEEP18 PEEP12 ZEEP
WAVELET
ALG1
AUC
Wav
=0.83; AUC
Fuz
=0.88
AUC
Wav
=0.94; AUC
Fuz
=0.86
AUC
Wav
=0.82; AUC
Fuz
=0.95
WAVELET
ALG2
AUC
Wav
=0.91; AUC
Fuz
=0.88
AUC
Wav
=0.97; AUC
Fuz
=0.86 AUC
Wav
=0.83; AUC
Fuz
=0.95
present model with this EIT contrast.
In order to identify the regions with similar
pixels, we began our analysis by a qualitative
evaluation from the patterns presented by EIT
signals. Based on experts’ experience of the
respiratory ICU at the Clinics Hospital of São Paulo,
Brazil, in a consensus method, we took off
conclusions about on which organ (heart or lungs)
each pixel belonged with larger possibility. This
analysis requires that the beginning of each EIT
signal must be synchronized with the peak of the
wave "R" of the ECG signal, marking the beginning
of the systolic phase. It allow us to identify the
pixels with the standard behavior of heart or lung.
According to discussed above, we proposed the
following method to analyze extracted signals of
thorax by means of Electrical Impedance
Tomography in order to identify the cardiac region:
a) We suppose that the pigs are healthy.
Therefore, the cardio-respiratory functions are
performed with certain normality and so we can
consider the same standard behavior found by
qualitative physiological analysis;
b) Two algorithms using the Wavelet Transform
were developed based on finding the pixel that had
the largest positive variation in its impedance during
the first half of the cardiac cycle and decomposing
the signal of the pixel above by means of the CWT
using the wavelet gaus4.
3 RESULTS AND DISCUSSIONS
The analysis of EIT signals of the thorax of the pig
with controlled pressure PEEP18 was used to
identify the macro regions according to variations of
blood flow during the cardiac cycle. After
physiological analysis, we determined a typical
variation of impedance of those found in ventricular
region during the cardiac cycle, in which the
different phases of the cardiac cycle are very well
defined. In order to find the adequate wavelet for our
analysis, several tests were performed. The wavelet
that adjusted better to the EIT signals was the gaus4.
Table 1 shows the heart maps provided by
wavelet and fuzzy approaches, and also the maps
found with the saline contrast. We can note in these
figures that the pixels, corresponding to the heart
region, are located in a superior central position,
independently of the PEEP values. It important to
detach that in this region there is a crossover of the
different cardio-breathing functional structures, such
as ventricle,
atrium, lung, aorta, and so on, which
causes important alterations in the expected pattern
for the dynamics of the cardiac cycle. We can also
note in table 1 that the wavelet approach, mainly the
wavelet algorithm 2, provides an almost crisp heart
map. Thus, in this method the pixel identification
uncertainties are practically vanished. The fuzzy
model provides an image containing pixels of
several magnitudes in the interval [0, 1], so varying
a cutoff value, the area corresponding to the heart
KEOD 2009 - International Conference on Knowledge Engineering and Ontology Development
382

region may contracts or expands. On the other hand,
varying the cutoff in the wavelet approach, the area
correspondent to the heart region practically does
not change. In this sense, the fuzzy model is
dependent of the cutoff value, which clearly is not
desirable in an automatic process. Other fact of great
importance in an automatic process is that the fuzzy
model is dependent of the PEEP settings, i.e., for
each PEEP its parameters need to be changed. This
limitation does not have in the wavelet model; its
configuration is not dependent on PEEP value.
Comparing the heart maps generated from wavelet
and fuzzy models with the image of the cardiac
region obtained by the saline method, we elaborated
ROC curves for each PEEP value. Table 2 presents
these results. We can note that both models
presented excellent agreements with the saline
injection. ROC curves of fuzzy and wavelet models
were practically equivalent. In general, the best
results were found with the wavelet algorithm 2.
Due to the movement of the heart in the
longitudinal axis and to the fact that the lungs should
be more closed in the ZEEP condition, it is expected
that the identification of the pixels as belonging or
not to each anatomical structure becomes more
difficult in this situation. In this sense, we expected
that the agreement would be larger for PEEP18,
followed by smaller values of agreement for
PEEP12 and ZEEP, respectively. However, this
monotonic behavior was not observed. The possible
hypothesis for this fact is that the ventricle was
dislocated to a more central region due to the heart
movement.
4 CONCLUSIONS
The wavelet methodology proposed was able to
identify the heart region from EIT data of perfusion
when compared with the saline method and fuzzy
model. Both methodologies present limitations to be
overcome. In the wavelet approach, we should have
extended our analysis to other cardiac chambers
beside the ventricular region. In the fuzzy model, the
limitations consist in the cutoff and PEEP
dependences in the generation of the heart maps.
These limitations should be understood in a more
deep work.
Finally, the results presented here were
encouraging and indicate that the modeling of EIT
images pos data acquisition, besides the
reconstruction algorithm, is a good way that should
be certainly explored
REFERENCES
Tanaka, H., Ortega, N. R. S., Galizia, M. S., Borges, J. B.,
& Amato, M. B. P., (2008). Fuzzy modeling of
electrical impedance tomography images of the lungs,
Clinics, 2008, vol.63, no.3, p.363-370. ISSN 1807-
5932.
Polikar R. (1999). The Engineer's Ultimate Guide to
Wavelet Analysis: The Wavelet Tutorial, 1999.
Retrieved March, 2009 from Web site
http://engineering.rowan.edu/~polikar/WAVELETS/
WTtutorial.html.
Adler, A., Amyot, R., Guardo, R., Bates, J.
H. T. &
Berthiaume, Y., (1997). Monitoring
changes in lung
air and liquid volumes with electrical impedance
tomography. J. Appl. Phys. 83: 1762-1767
Brown, B.H. (2003). Electrical impedance tomography
(EIT): a review, Journal of Medical Engineering &
Technology, 2003, vol. 27, n
o
3, pp. 97-108.
Noor, J.A. E. (2007). September) Electrical Impedance
Tomograph at low frequencies [Thesis of Doctor],
Faculty of Science at University of New South Wales.
Retrieved October 2008 from
http://unsworks.unsw.edu.au/vital/access/services/Do
wnload/unsworks:1359/SOURCE02?view=true.
Lima, R. G. , Aya, J. C. C. , Moura, F. S. , Schweder, R.
K. , Mirandola, L. A. S. & Pai, C. N. , (2005). A
black-box back-projection algorithm for electrical
impedance tomography, in Proceedings of the 18th
International Congress of Mechanical Engineering,
Ouro Preto, Minas Gerais, Brazil.
IDENTIFYING THE CARDIAC REGION IN IMAGES OF ELECTRICAL IMPEDANCE TOMOGRAPHY THROUGH
WAVELET TRANSFORM
383
