
AUTOMATING THE IMPORTATION OF MEDICATION DATA
INTO PERSONAL HEALTH RECORDS
Juha Puustjärvi
Helsinki University of Technology, Innopoli 2, Tekniikantie 14, Espoo, Finland
Leena Puustjärvi
The Pharmacy of Kaivopuisto, Neitsytpolku 10, Helsinki, Finland
Keywords: Medication data, e-Prescription, Personal health record, Business process management, XML, RDF.
Abstract: A personal health record (PHR) provides a summary of the health and medical history of a consumer. It
includes data gathered from different sources such as from health care providers, pharmacies, insures, the
consumer, and third parties such as gyms. Importing data into PHRs is problematic as different data sources
use different representation formats. In addition, automating the importation is problematic as many of the
sources are built based on proprietary solutions, and thereby are not able to interoperate with PHR systems.
In this paper, we described how the importation of e-prescriptions into PHRs can be automated. In our
solution e-prescriptions are produced by an electronic prescription writer (EPW) which functionality is
specified by BPMN notation and then translated into executable WS-BPEL code. The EPW sends CCR-
formatted data of e-prescriptions into PHR system, which first transforms (if needed) the data into the
format of the used PHR system, and then stores them into PHRs. In particular, we consider how a PHR
system can transform a CCR-formatted data into RDF/XML format. The gain of such transformation is that
we can implement the PHR system as an application of a knowledge base system, and thereby we can
capture the wide expression power of knowledge base system’s query interface into the PHR system.
1 INTRODUCTION
E-prescription is the electronic transmission of
prescriptions of pharmaceutical products from
legally professionally qualified healthcare
practitioners to registered pharmacies (Batenburg
and Van den Broek, 2008). The information in an e-
prescription includes for example, prescribed
products, dosage, amount, frequency and the details
of the prescriber.
The problems related to prescribing medication
are discussed in many practitioner reports and public
national plans, e.g., in (Hyppönen et al., 2005;
Puustjärvi and Puustjärvi, 2006; Dwivedi et al, 2007;
Batenburg and Broek, 2008; Ghani et al., 2008).
These plans share several similar motivations and
reasons for the implementation of electronic
prescription systems (EPSs). These include:
reduction of medication errors, speeding up the
prescription ordering process, better statistical data
for research purposes, and financial savings.
Physicians usually produce e-prescriptions by
exploiting specific electronic prescription writers
(EPWs), which also assist in storing e-prescriptions
into prescription holding stores. As a result of recent
interest in personal health records (PHRs) a relevant
challenge is to extend EPWs in a way that they are
also able to store e-prescriptions into PHRs.
A PHR is a record of a consumer that includes
data gathered from different sources such as from
health care providers, pharmacies, insures, the
consumer, and third parties such as gyms (Agarwal
et al., 2006; Kaelber et al, 2008). It typically
includes information about medications, allergies,
vaccinations, illnesses, laboratory and other test
results, and surgeries and other procedures (Lewis et
al., 2005; Tuil et al, 2006).
An ideal PHR provides a complete and accurate
summary of the health and medical history of a
consumer (Angst et al., 2008). It is accessible to the
consumer and to those authorized by the consumer.
It is not the same as electronic health record (EHR)
135
Puustjärvi J. and Puustjärvi L. (2010).
AUTOMATING THE IMPORTATION OF MEDICATION DATA INTO PERSONAL HEALTH RECORDS.
In Proceedings of the Third International Conference on Health Informatics, pages 135-141
DOI: 10.5220/0002335801350141
Copyright
c
SciTePress

(EHR, 2009), which is designed for use by health
care providers (Raisingha and Young, 2008).
PHRs can be classified according to the platform
by which they are delivered. In internet-based PHRs
health information is stored at a remote server, and
so the information can be shared with health care
providers. They also have the capacity to import data
from other information sources such as a hospital
laboratory and physician office. However, importing
data to PHRs from other sources requires the
standardization of PHR-formats.
Various standardization efforts on PHRs have
been done. In particular, the use of the Continuity of
Care Record (CCR standard) of ASTM and HL7’s
(Dolin et al., 2001) Continuity of Care Document
(CCD standard) has been proposed. From
technology point of view CCR (CCR, 2009) and
CCD-standards (CCD, 2009) represent two different
XML schemas designed to store patient clinical
summaries. However, both schemas are identical in
their scope in the sense that they contain the same
data elements.
It is widely anticipated that in the near future
PHRs have the potential to dramatically change
healthcare. However, our argument is that a critical
aspect of current PHRs’ use is their consistency. In
particular the recall (the fraction of the relevant
documents, which have been stored in PHRs) is
crucial: making healthcare decision on inadequate
data may be a strong risk.
It is evident that the recall of PHRs is highly
dependent on the way the data is imported to PHRs.
Our argument is that in order to ensure that a PHR
includes an accurate medical history of the patient
the importation of source data into PHRs should be
done automatically. Re-entering data into PHRs
would cause additional manual operations, and the
importation of all the relevant data cannot be
ensured.
In this paper, we describe our work on automatic
importation of e-prescriptions’ data into PHRs. We
will illustrate the extension of WS-BPEL based
EPW in a way that it can automatically send
prescriptions’ data into relevant PHRs. The format
of the data follows the CCR standard. However, we
do not assume that all PHR-systems are based on
CCR standard since the format can be transformed
by a stylesheet engine into PHR system’s used
format. As an example, we present how a CCR-file
can be transformed into RDF/XML-format (RDF,
2004). The gain of using RDF/XML-format is that
we can store the data in a knowledge base which
provides powerful querying facilities on PHRs. This
in turn increases the efficient and reliable use of the
PHRs.
The rest of the paper is organized as follows.
First, in Section 2, we give an overview of an
electronic prescription process in which prescription
writer application interacts with other health care
applications. Then we illustrate how BPMN can be
used in modelling the coordination of electronic
prescription processes. In Section 3 we present the
service oriented architecture where EPW takes
place. In Section 4 we consider the representation
formats of the delivered medicinal and give an
example of transforming a CCR-file into RDF. The
gains of using RDF-formatted PHRs are analyzed in
Section 5. Finally Section 6 concludes the paper by
discussing the weaknesses and advantages of our
developed solutions.
2 e-PRESCRIPTION PROCESS
2.1 Constructing e-Prescriptions
In our used model, in prescribing medication the
physician uses an EPW. The prescribing process
goes as follows: First the physician request from the
patient whether the patient have a PHR, and whether
the data of the new prescription should be stored in
patient’s PHR. In the case positive attitude the
physician delivers that information to EPW. If the
EPW do not have information about patient’s PHR
then such information is requested from the patient
and then delivered to the EPW.
In prescribing the actual medication the EPW
used by the physician may interact with many other
health care systems in constructing the prescription.
For example, the EPW may query previous
prescriptions of the patient from the prescription
holding store and from patients PHR (in the case of
authorized by the patient). The EPW may also query
patient’s records from other health care systems.
Once the physician has constructed the
prescription the EPW sends the prescription to the
medical expert system which checks (in the case of
multi drug treatment) whether the prescribed drugs
have mutual negative effects, and whether they have
negative effects with other ongoing medical
treatment of the patient. Then the EPW sends the
prescription to a medical database system, which
checks whether the dose is appropriate. The medical
database may also provide drug-specific patient
education in multiple languages. It may include
information about proper usage of the drug,
warnings and precautions, and it can be printed to
HEALTHINF 2010 - International Conference on Health Informatics
136
the patient. Then the EPW sends the prescription to
a pricing system, which checks whether some of the
drugs can be changed to a cheaper drug.
Once the checks and possible changes have been
done the physician signs the prescription
electronically. Then the prescription is encrypted
and sent to an electronic prescription holding store.
The patient is usually allowed to take the
prescription from any pharmacy in the country. At
the pharmacy the patient gives the prescription to the
pharmacist. The pharmacist will then request the
electronic prescription from the electronic
prescription holding store. After this the pharmacist
will dispense the drugs to the patient and generates
an electronic dispensation note. Finally they
electronically sign the dispensation note and send it
back to the electronic prescription holding store.
Hence the dispensation of the e-prescription is also
stored in the prescription holding store.
2.2 Modelling e-Prescription Processes
Now we illustrate how the coordination of the
interoperability required by electronic prescription
systems can be automated by utilizing XML-based
languages. In particular we show how the Business
Process Modeling Notation (BPMN) (BPMN, 2005)
and Web Services Business Process Execution
Language (WS-BPEL) (WS-BPEL, 2007) can be
used for automating the coordination of electronic
prescription processes.
The reason for using BPMN is that the BPMN
notation is readily understandable for the employees
of the health care sector. It is also readily
understandable for the business analyst that create
the drafts of health care processes as well as for the
technical developers responsible for implementing
the technology that will perform those processes. In
addition, a notable gain of BPMN specification is
that it can be used for generating executable WS-
BPEL code.
BPMN provides a graphical notation for
specifying business processes in a Business Process
Diagram (BPD), based on a flowcharting technique
very similar to activity diagrams from Unified
Modeling Language (UML).
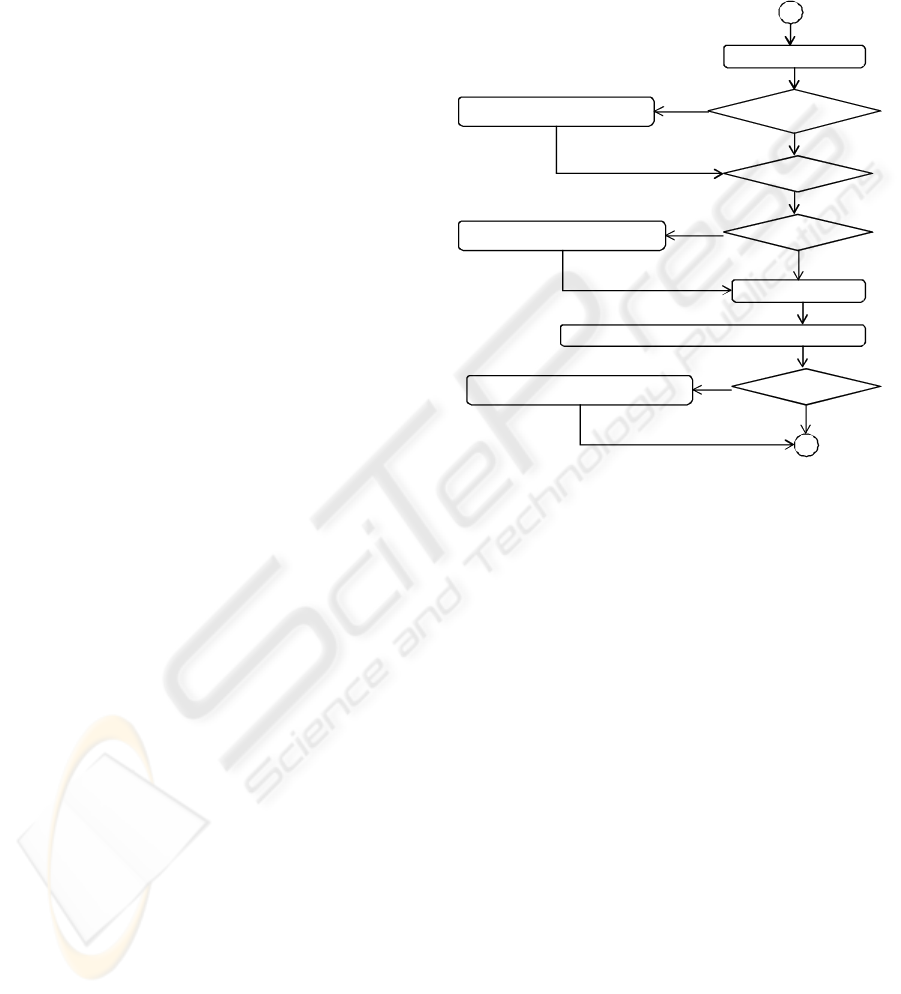
In BPD there are tree Flow Objects: Event,
Activity and Gateway: An Event is represented by a
circle and it represents something that happens
during the business process, and usually has a cause
or impact. An Activity is represented by a rounded
corner rectangle and it is a generic term for a work
that is performed in companies. A Gateway is
represented by a diamond shape, and it is used for
controlling the divergence and convergence of
sequence flow. In BPD a Sequence Flow is
represented by a solid line with a solid arrowhead.
In Figure 1 we have presented how the process
of producing electronic prescription (described in
Section 2.1) can be represented by a BPD.
Construct apre scription
Check negative effectsSe nd toe xpert database system
Yes
Che c k thedose
No
Che c k thepr ice s
No
Se nd tomedical datab as e sys tem
Yes
Sign th e pr escription
No
Se nd the prescription to p re s cription ho ldin gstore
Chec k thePHRSe nd thepre scr iption to PHRsyste m
Yes
No
Figure 1: A prescription process presented by a BPD.
3 EXECUTING
e-PRESCRIPTION PROCESS
Web Services Business Process Execution Language
(WS-BPEL) is an XML based programming
language to describe high level business processes
(WS-BPEL, 2007). A 'business process' is a term
used to describe the interaction between two
businesses or two elements in some business. An
example of this might be an EPW system requesting
from the expert database system whether two drugs
have negative mutual effects. WS-BPEL allows this
interaction to be described easily and thoroughly
such that the expert database system can provide a
Web Service and the EPW can use it.
In terms of WS-BPEL, the term 'Web Service'
means something with which one can interact (Singh
and Huhns, 2005). For example, in our prescribed e-
prescription process there are web services that are
interacted to get information whether there are
substitutable drugs having lower prices.
The interactions of web services are described
from architectural point of view in Figure 2.
AUTOMATING THE IMPORTATION OF MEDICATION DATA INTO PERSONAL HEALTH RECORDS
137
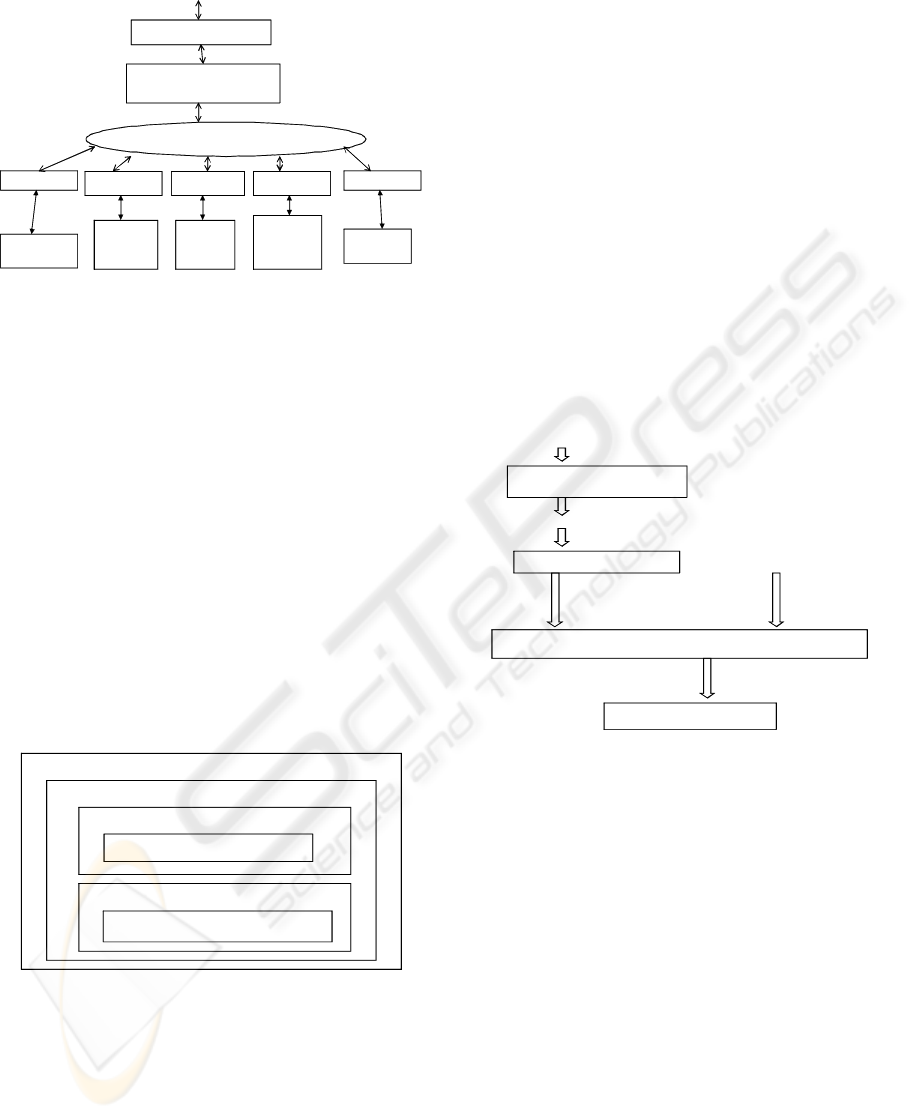
Electronic Prescription Writer
(WS-BPEL engine)
Expert
database
system
Medical
database
system
Prescription
holding store
Prescription
pricing
authority
PHR
system
WS-interface WS-interfaceWS-interface WS-interface WS-interface
WS-interface
Physician
Internet / SOAP-messages
Figure 2: The interoperation of the EPW.
The EPW (WS-BPEL engine) loads WS-BPEL
specifications and then runs the prescription process.
A nice feature of WS-BPEL engines is that they
itself are also web services. Hence the physician
interacts with the web service interface of the EPW.
The EPW communicates with other systems by
using the SOAP protocol (SOAP, 2009), which was
originally intended to provide networked computers
with remote-procedure call services written in XML.
It has since become a simple protocol for
exchanging XML-messages over the Web.
A SOAP-message is comprised of a SOAP
header, SOAP envelope and SOAP body (Singh and
Huhns, 2005). In particular, the SOAP body contains
the application-specific message that the backend
application will understand. As illustrated in Figure
3, we incorporate our used CCR-formatted
medicinal documents in the SOAP body.
HTTP Header
SOAP Envelope
SO AP Header
Headers
SOAP Body
CCR-formatted PHR-element
Figure 3: A CCR-formatted PHR-element in a SOAP-
message.
4 REPRESENTATION FORMATS
4.1 Transforming PHR-formats
In order that the medicinal information systems are
able to handle the XML-elements of the SOAP-
messages they have to use the DOM-parser and the
Stylesheet engine. The DOM parser (Daconta et al.,
2003) transforms input text (i.e., CCR-elements) into
a tree, which is suitable for the Stylesheet engine to
process.
The term DOM (Document Object Model)
(Daconta et al., 2003) refers to a language-neutral
data model and application programming interface
(API) for programmatic access and manipulation of
XML-coded data. Generally, parsing (also called
syntactic analysis) is the process of analyzing a
sequence of tokens to determine its grammatical
structure with respect to a given formal grammar.
As illustrated in Figure 4, the Stylesheet engine
takes the CCR-formatted XML-document from the
DOM-parser, loads it into a DOM source tree, and
picks out the needed information in transforming the
XML-document with the instructions given in the
local (PHR-specific) stylesheet.
Stylesheet engine
P H R in a lo c a l fo rm a t
Local Stylesheet
CCR-form atted
PHR in a tree
fo rm
PHR in CCR-format
DOM -parser
PHR system
W eb service
SOAP-m essage in XM L
Figure 4: Transforming the representation format of a
CCR file.
4.2 Transforming a CCR-file into RDF
The CCR standard is an ANSI-accredited health
information technology standard, which is published
in 2006. Though it is proposed for PHRs its original
purpose is to enable the creation, storing and
exchange (between computer systems) of digital
summaries of individuals’ administrative and
clinical health information.
A CCR-file is comprised of seventeen sections. It
is not intended to capture individuals’ all past
medical history but instead to summarize
information that will be most useful in individual’s
medical encounter with a new or unfamiliar
provider.
The sections of the CCR standard include for
example patient demographics, insurance
information, immunizations, allergies, diagnoses,
HEALTHINF 2010 - International Conference on Health Informatics
138

procedures and medication list. Each section
contains elements that can represent free text or
structured XML-coded text. The content of each
CCR file is captured from various sources such as
from hospital information system, a clinical
laboratory, from a pharmacy or from the patient him
or herself. In order to know who or what
organization is the source of each element in a CCR
file each data element is time and source stamped.
A simplified example of a CCR file is presented
in Figure 5. It represents a CCR file that has a
medication list (element Medications) which is
comprised of one medication (element Medication)
that is source stamped by the Pharmacy of
Kaivopuisto.
<ContinityOfCareRecord>
<Patient><ActorID>Person.12345></ActorID></Patient>
<Medications>
<Medication>
<CCRDataObjectID>
Medication567
</CCRDataObjectID>
<DateTime>
<ExactDateTine>
2009-03-01TO12:00
</ExactDateTime>
</DateTime>
<Source>
<Actor>
<ActorID>Pharmacy of Kaivopuisto</ActorID>
<ActorRole>Pharmacy</ActorRole>
</Actor>
</Source>
<Description>
<Text>One tablet three times a day</Text>
</Description>
<Product>
<ProductName>Voltaren</ProductName>
<BrandName>Diclofenac</BrandName>
</Product>
<Strenght>
<Value>50</Value>
<Unit>milligram</Unit>
</Strenght>
<Quantity>
<Value>30</Value>
<Unit>Tabs</Unit>
</Quantity>
</Medication>
</Medications>
</ContinityOfCareRecord>
Figure 5: An element of a CCR file.
In order to illustrate the transformation of CCR
files into RDF, the CCR file of Figure 5 is presented
in RDF/XML format in Figure 6.
<rdf:RDF
xmlns : rdf=
”http://www.w3.org/1999/02/22-rdf-syntax-ns#”
xmlns : xsd=”http://www.w3.org/2001/XMLSchema#”
xmlns : po=http://www.lut.fi/ontologies/p-ontology#>
<rdf:Description rdf:about=”120962-K3”>
<rdf:type rdf:resource=“&po;Patient”/>
<po : PatientName>Lisa Smith</po : PatientName>
<po : Uses>MO-5481</po:Uses>
<po : Performed>H-257L</po : Performed>
</rdf : Description>
<rdf:Description rdf:about=” MO-5481”>
<rdf:type rdf:resource=“&po;Medication”/>
<po : Contains>Voltaren</po : Contains>
<po : StrenghtValue rdf:datatype=
”&xsd;integer”>30</po : StrenghtValue>
<po : StrenghtUnit>Tabs</po : StrenghtUnit>
</rdf : Description>
<rdf:Description rdf:about=” 211708-8”>
<rdf:type rdf:resource=“&po;Source/>
<po : ActorRole>Pharmacy</po : ActorRole>
</rdf : Description>
<rdf:Description rdf:about=” Voltaren”>
<rdf:type rdf:resource=“&po;ProductName”/>
<po : BrandName>Diclofenac</po : Contains>
</rdf : Description>
</rdf:RDF>
Figure 6: A PHR in RDF/XML format.
5 THE GAINS OF USING RDF IN
PERSONAL HEALTH RECORD
We have investigated the use cases of PHRs. It is
turned out that patients are not only interested about
single documents such as the content of the previous
prescription but most of the searches or queries
require computing over many documents. For
example, a patient may be interested to know the
average blood pressure and/or blood sugar
concentration (glucose level) during the time periods
he or she was using Diovan (a drug for blood
pressure), or the patient may be interested to know
the cholesterol values when he or she was on a diet.
Unfortunately the computation required by such
data centric queries is not supported by the query
languages (e.g., XPath (XPath, 2008) and XQuery
(Xquery, 2008) that are designed to address XML-
documents. The problem here is that the CCR- (as
well as the CCD-based) PHRs are XML-documents
that can only be accessed by the query languages
developed for XML-documents.
This is the reason why we have developed PHRs,
which content is structured according to an
ontology, and which thereby allow a wide variety of
data centric searches and queries. In particular, we
have used OWL (Web Ontology Language) (OWL,
2006) in designing the PHR-ontology. The instances
AUTOMATING THE IMPORTATION OF MEDICATION DATA INTO PERSONAL HEALTH RECORDS
139
of the ontology are presented in RDF. Hence, for
example the RDF-formatted PHR element of Figure
6 can be stored in an ontology based PHR system.
Fundamentally, the purpose of the PHR-ontology
is to describe the concepts of the domain in which
PHRs take place. Hence, a PHR-ontology describes
the concepts (as well as their relationships) such as
demographics, insurance information,
immunizations, allergies, diagnoses, procedures and
medication.
In developing the PHR-ontology we have
exploited the XML-schema of the CCR file. In
transforming the XML schema to OWL-ontology we
have used on the whole the following rules:
• Complex elements are transformed to
OWL classes.
• Simple elements are transformed to
OWL data properties.
• Element-attribute relationships are
transformed to OWL data properties.
• The relationships between complex
elements are transformed to class-to-
class relationships (object properties).
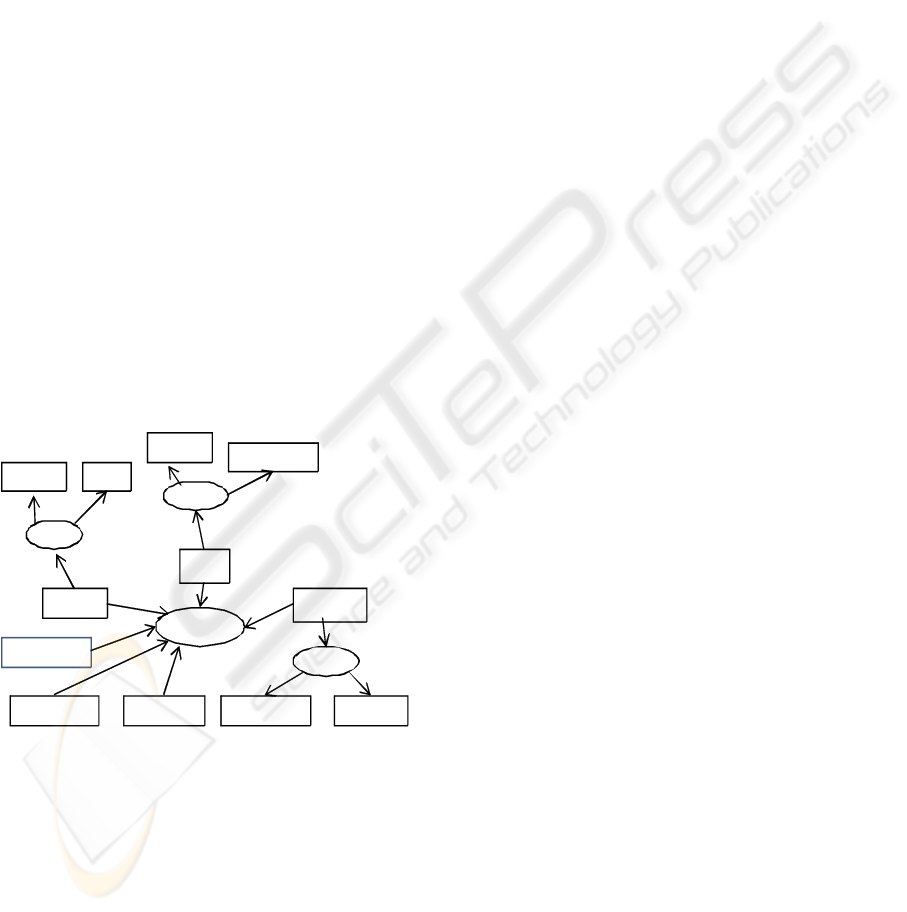
To illustrate this kind of transformation, a simple
PHR-ontology is presented in Figure 7. In this
graphical representation ellipses represent classes,
and rectangles represent data and object properties.
Patient
Me di c ati on
Product
ProductN am e BrandN am eStrenghtU nit
Source
ActorIDActorRole
PatientId
PatientN am e
Uses
Contains
StrenghtValue
O rig in at es
Medi c ati onId
Figure 7: A simple PHR-ontology in a graphical form.
6 CONCLUSIONS
It is obvious that in the near future PHRs have the
potential to dramatically change healthcare. They
will enable consumer to become more involved and
engaged in their care, and allow other authorized
stakeholders to access information about consumer
that has not been previously been available or
difficult to access electronically. The change that
can be caused by the deployment of PHR systems
could have a significant impact on the efficiency of
administrative and clinical process within healthcare
sector, and thus will give rise for considerable cost
savings.
However, the extensive exploitation of PHRs
requires that (i) PHRs are exhaustive in the sense
that they contain all the relevant documents, and that
(ii) PHR systems support appropriate use cases such
as data centric queries.
Our argument is that the exhaustive medicinal
history can be captured in PHRs only if we can
automate the importation of relevant documents into
PHRs. As we have presented, one way of doing that
with respect to e-prescriptions is to extend the EPWs
by exporting the prescriptions into PHRs. Further, in
order to support appropriate use cases, we can
implement the PHR system as an application of a
knowledge base or a database system.
The importation of e-prescriptions into PHRs is
rather straightforward if the EPW exploits service
oriented architecture. In particular, if the EPW is
based WS-BPEL then the required modifications can
be done by just inserting appropriate operations in
the WS-BPEL code.
In order to support a wide variety of queries on
PHRs we have analyzed PHRs, which data is
structured according to an PHR ontology. Importing
data from XML-based data sources (e.g., HL7 CDA
compliant systems) to such PHR system requires
that the XML documents are first transformed by a
style sheet engine to RDF/XML format and then
inserted to the PHR.
We will emphasize that using a PHR should not
be an end in itself: if the PHR captures information
that is imported at random, then the use of the PHR
in healthcare may be a risk. Developing and
maintaining a reliable and exhaustive PHR requires
considerable efforts in developing health care
systems interoperability.
The deployment of a reliable PHR system is also
an investment. The investment includes a variety of
costs including software, hardware and training
costs. Introducing and training the staff on new
technology is a notable investment, and hence many
organizations like to cut on this cost as much as
possible. However, the incorrect usage and
implementation of a new technology, due to lack of
proper training, might turn out to be a risk of
healthcare.
HEALTHINF 2010 - International Conference on Health Informatics
140

REFERENCES
Agarwal R, Angst C.M., 2006. Technology-enabled
transformations in U.S. health care: early findings on
personal health records and individual use, In Galletta
G, Zhang P, (Eds.), Human-Computer Interaction and
Management Information Systems: Applications (Vol.
5). Armonk, NY: M.E. Sharpe, Inc., pp. 357-378.
Angst, C.M., Agarwal, R, Downing, J., 2008. An
empirical examination of the importance of defining
the PHR for research and for practice, Proceedings of
the 41st Annual Hawaii International Conference on
System Sciences.
Batenburg, R., Van den Broek, E., 2008. Pharmacy
information systems: the experience and user
satisfaction within a chain of Dutch pharmacies,
International Journal of Electronic Healthcare. Vol. 4,
No.2 pp.119-131.
BPMN, 2005. Business Process Modeling Notation
(BPMN), Available at: http://www.bpmn.org/
CCD, 2009. What Is the HL7 Continuity of Care
Document? Available at:
http://www.neotool.com/blog/2007/02/15/what-is-hl7-
continuity-of-care-document/
CCR, 2009. Continuity of Care Record (CCR) Standard.
Available at: http://www.ccrstandard.com/.
Daconta, M., Obrst, L., Smith, K. (2003) The semantic
web. Indianapolis: John Wiley & Sons.
Dolin, R. H., Alschuler; L., Beerb, C., Biron, P. V.,
Boyer, S- L, Essin, D., Kimber, E., Lincoln, T., and
Mattison, J-E., 2001. The HL7 Clinical Document
Architecture. J. Am Med Inform Assoc (6). pp 552-
569.
Dwivedi, A., Bali, R.K., Wickramasinghe, N., Naguib,
R., 2007. How workflow management systems enable
the achievement of value driven healthcare delivery.
International Journal of Electronic Healthcare, Vol. 3,
No.3 pp.382-393.
EHR, 2009, Electronic Health Record, Available at:
http://en.wikipedia.org/wiki/Electronic_health_record.
Ghani, M., Bali, R.K., Naguib, R., Marshall, I.M.,
Wickramasinghe, N.S., 2008. Electronic health
records approaches and challenges: a comparison
between Malaysia and four East Asian countries,
International Journal of Electronic Healthcare,Vol. 4,
No.1 pp.78-104-77.
Kaelber, D. Jha, A. Johnston, D. Middleton, B.and Bates,
D., 2008. A Research Agenda for Personal Health
Records (PHRs), J. Am. Med. Inform. Assoc.,
November 1,15(6). pp. 729 - 736.
Lewis, D, Eysenbach. G., Kukafka, R., Stavri P.Z., and
Jimison, H., 2005. Consumer health informatics:
informing consumers and improving health care. New
York: Springer.
Hyppönen, H., Salmivalli, L., Suomi, R.,2005. Organizing
for a National Infrastructure: The Case of the Finnish
Electronic Prescription. In Proc. of the 38th Hawaii
International Conference on System Sciences.
OWL, 2006. Web OntologyLanguage.
http://www.w3.org/TR/owl-ref/
Puustjärvi, J., Puustjärvi, L. ,2006. The challenges of
electronic prescription systems based on semantic web
technologies. In Proc. of the 1st European Conference
on eHealth, pp. 251-261.
Raisinghani. M.S. and Young, E., 2008. Personal health
records: key adoption issues and implications for
management, International Journal of Electronic
Healthcare. Vol. 4, No.1 pp.67-77.
RDF, 2004, Resource Description Framework (RDF).
Available at: http://www.w3.org/RDF/
Singh, M. and Huhns, M. (2005) Service Oriented
Computing: Semantics Proceses Agents. John Wiley &
Sons.
SOAP, 2009. SOAP. Available at:
http://en.wikipedia.org/wiki/SOAP.
Tuil, W. S., Hoopen, A. J., Braat, D. D. M., Vries Robbe,
P.F., and Kremer J. A. M., 2006. Patient-centred care:
using online personal medical records in IVF practice,
Hum. Reprod., November 1, 21(11). pp. 2955 - 2959.
WS-BPEL, 2007. Web Services Business Process
Execution Language (WS-BPEL) Available at:
http://docs.oasis-open.org/wsbpel/2.0/varprop.
XPath, 2008. XML Path Language (XPath). Available at:
http://www.w3.org/TR/xpath.
Xquery, 2008. XQuery 1.0: An XML Query Language.
Available at: http://www.w3.org/TR/xquery/.
AUTOMATING THE IMPORTATION OF MEDICATION DATA INTO PERSONAL HEALTH RECORDS
141
