
A FLEXIBLE POLICY ARCHITECTURE FOR MEDICAL
INFORMATION MESSAGING
Edward Brown
Department of Computer Science, Memorial University of Newfoundland, St. John's, Canada
Jamie Goodyear
Progress Software Corporation, 570 Newfoundland Drive, St. John's, Canada
Keywords: Policy, Messaging, Architecture, Middleware, Medical context.
Abstract: We describe a design solution for the problem of changing policies regarding information management in
the health care environment. Frequent policy modification regarding security, privacy and workflow
through institutional re-organization and policy revision occur at multiple levels of administration, which
can leave the health care information users with non-compliant systems (such as electronic medical records)
and procedures which are expensive and difficult to update. Our solution is a medical information
messaging infrastructure designed to respond flexibly to changes in information policy. Instead of
embedding fixed policy into static application code, our architecture provides configurable policy rules as
part of the communications framework. This entails two critical components: the dynamic router, which
routes messages according to the policy rules, and the medical context header, which attaches policy-
relevant information to all communication messages. All information applications are automatically
compliant with policy, since it is enforced at the communications level of the system.
1 INTRODUCTION
Large scale communication infrastructure for
medical information applications is essential if
different medical applications, such as electronic
medical records and electronic prescription services,
are to be interoperable. In other words, information
needs to be shared seamlessly across different
applications, vendor systems, jurisdictions, and
health care providers. The Canadian health care
system, being substantially government funded and
therefore having a close relationship between
funding and regulation, is one context in which such
an infrastructure can be designed and built as a
federal initiative. The underpinning of this
infrastructure in Canada is a common
communication layer, called the Health Information
Access Level (HIAL). With a common information
exchange architecture, the HIAL solution provides
for different applications to share and retrieve
information stored in repositories throughout the
system. (CHI, 2003)
However, questions of the legitimacy of
information access are not addressed by any specific
architectural feature. Policies regarding who, when
and why information may be accessed and used are
not explicitly represented in the system architecture.
Instead, security and privacy solutions and services
that can be deployed when policies are developed.
These follow traditional security monikers and
solutions, such as authentication, identity
management and other software mechanisms.
(Brown and Wareham, 2007)
The concern with these solutions is that policies
regarding information exchange and access are re-
created as part of each application. In each case,
procedures for implementation of these policies,
such as accessing an authentication service, are
coded into the application programs. When policy
changes occur, the applications may not be suited to
any changes and the cost of updating the
applications may place an unnecessary burden on
health care budgets. We contend that such policy
changes are in fact frequent, particularly at the level
of individual organizations such as hospitals. (see
Brown and Wareham, 2007, at 46)
70
Brown E. and Goodyear J. (2010).
A FLEXIBLE POLICY ARCHITECTURE FOR MEDICAL INFORMATION MESSAGING.
In Proceedings of the Third International Conference on Health Informatics, pages 70-76
DOI: 10.5220/0002737100700076
Copyright
c
SciTePress

Consider, for example, the case of “reportable”
diseases which require notice to a public health
authority. The obligation to report such diseases
typically falls on the primary care physician. (see
HPPA, 1990 for one Canadian jurisdiction) An
electronic information system could help the
physician's information management burden, by
automatically reporting such diagnoses. However,
there are variations on regulations, process, and
responsible authority between provincial
jurisdictions. These policies may change or be
amended fairly quickly, such as in response to a
particular epidemic threat. If policy changes entail
reprogramming of application code or circumvention
of legacy procedures that are embedded in software
applications, then software hinders, rather than
helps, such reporting.
There are even more frequent information
management policy changes on a more detailed
institutional level. A particular lab or individual
may be censured, health service units may be
restructured, information workflow may be re-
organized, institutional analysis procedures may be
revised: these all have implications for how
information is shared and accessed, which we refer
to as information policy.
The tendency is to implement applications based
on existing policies or regulations, without regard
for the frequent re-interpretation or change of policy,
due to administrative decisions (as per the preceding
paragraph), new regulation, new technologies,
innovation in health care strategies or even court
decisions which alter obligations or liability. The
ability to respond to such changes is compromised
when the system enforces procedures and policies
that were current or thought appropriate at the time
the system was designed. Vendors that design,
create and/or implement systems have little
incentive to design to accommodate such future
changes, particularly if they can look forward to
being engaged and paid to overhaul their application
program each time changes do occur.
Our prototype system deploys information policy
at the communications layer of the system rather
than within each application, making the system
aware of the medical context of each
communications message. This relieves the
application code of the burden of compliance with
(possibly changing) information policies.
Active use of medical context has precedent,
including context-aware computing (Bricon-Scouf
and Newman, 2007), linking of related medical
events (Clerq, Bangels and France, 2004),
annotating EHR records with disambiguating
context (Manzoor, Ceusters and Rudniki, 2007),
mobile access through user and location context
(Hägglund et al, 2007), adaptive information for
telemedicine communications (Doukas,
Maglogiannis and Karpouzis, 2008), and hospital
applications such as context aware pill containers or
hospital beds (Bardram, 2004). This literature
illustrates the importance of context not only in the
operation of health care tools and software systems,
but also in understanding needs of the user and
patient.
Although there are application specific uses for
this medical context information, such as tracking
and logging medical events and data security
forensics, we limit this discussion to messaging
infrastructure advantages.
2 CONTEXT-BASED
MESSAGING
Our problem is to provide for policy changes within
the architecture of the medical information
infrastructure itself. By making information policy
explicit in the system architecture, rather than
implicit (and possibly hidden) in the coding of each
individual software application, we are able to
change information access and information sharing
characteristics as a system configuration exercise.
Policy changes are new system configuration
directives (that is, messaging rules), rather than re-
coding of applications.
This architecture introduces two critical
elements: first is the use of a dynamic router for
messaging within the information infrastructure used
by all applications; the second is attaching medical
context headers to each message to which the
dynamic router can respond.
2.1 Dynamic Router
A dynamic router will route messages according to a
rules base which can be configured manually or
automatically, and changed dynamically without
halting any system operations or services. The
router makes decisions about where specific
messages are to be sent based on the message itself
and the current rules in its rules base. Since the
router is dynamic, the rules can be modified
manually or through software that is appropriately
authenticated for making such alterations. Routing
messages based on current information management
policies is a matter of translating the policies into
routing rules which are added to the current rules
base.
A FLEXIBLE POLICY ARCHITECTURE FOR MEDICAL INFORMATION MESSAGING
71
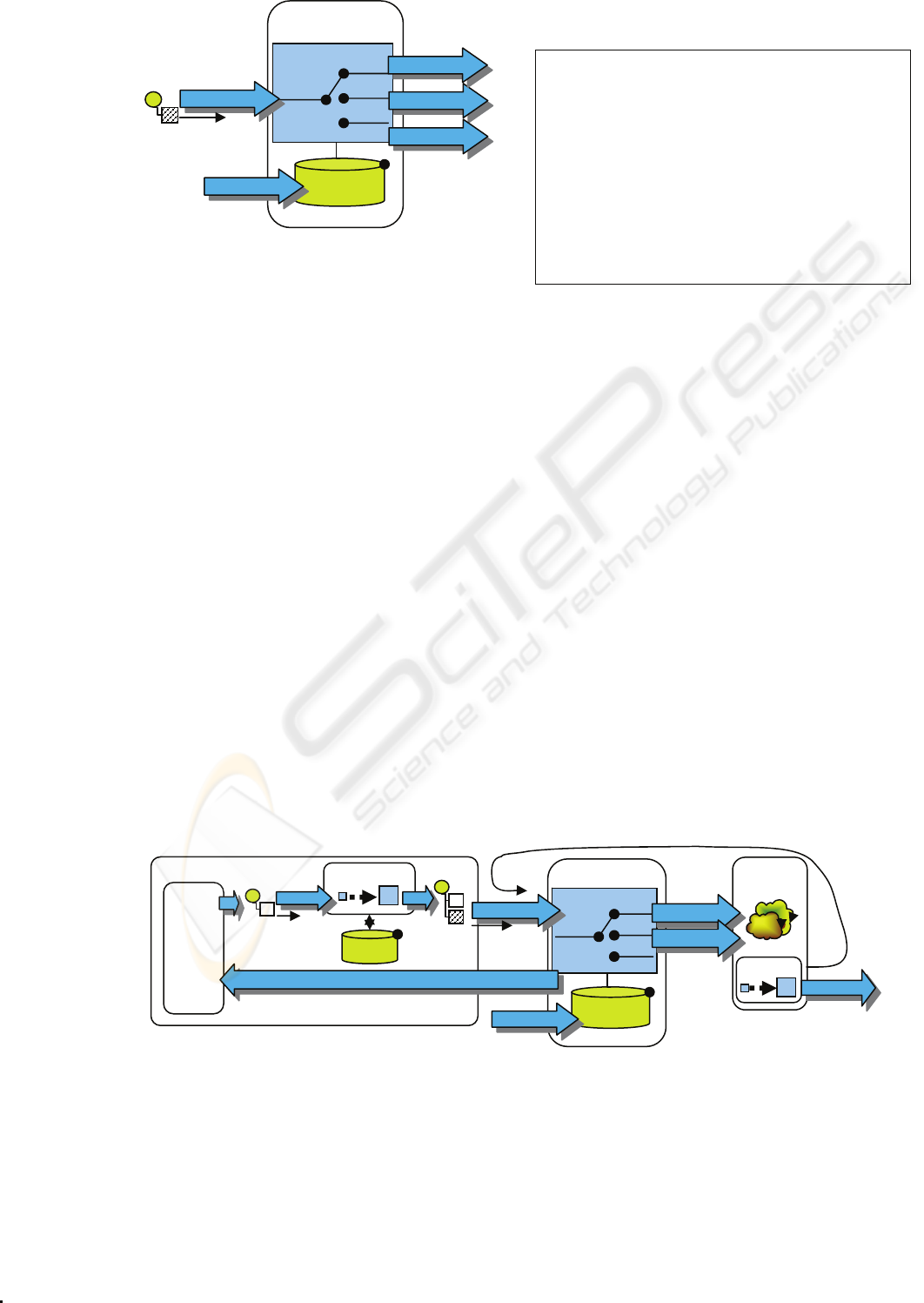
Figure 1: Dynamic Router.
The dynamic router appears in architectural
design texts as an enterprise integration pattern
whose application is well understood. (Hohpe and
Woolf, 2003) Its use allows the explicit expression
of routing policies in a consistent manner, and at a
known and configurable point in the overall system.
All applications will be operating in accordance with
the policies encoded by the routing rules.
In the dynamic router architectural pattern
(shown in Figure 1) the routing rules are retrieved
from a rules data store. (Hohpe and Woolf, 2003)
This frees message distribution from complete
preplanning as routes may be added, modified, or
removed at run time.
The dynamic router includes a rules engine (not
shown). This component is responsible for
accessing, modifying and storing rules for the router.
For example, the rules engine may be directed to
modify the rules base by adding or deleting rules, or
retrieve the currently stored rules for inspection.
Messages for the rules engine relating to
administration of the rules base itself use a special
“control” channel for its own messages.
The concept of a dynamic router is not itself
original; it is in common use in financial services
software and can even be seen in e-Health
information frameworks. (Krasser, 2009) Our
contribution is using the rules base for explicit
information policies, rather than mere application
configuration.
stjohns;Results;dr.farrell.response.que
ue;tcp://localhost:61616
stjohns;radiology;radiology;tcp://local
host:61612
stjohns;microbio;microbio;tcp://localho
st:61620
stjohns;clientreq;Q_RecordRequest;tcp:/
/localhost:61628
stjohns;ReportD;pub.health;tcp://localh
ost:61624
stjohns;Patient_Record;*meddrid;tcp://l
ocalhost:61616
Figure 2: Some routing rules as they appear in one test of
the policy-oriented rules base.
Our implementation adopts the Apache Camel
messaging framework, which provides information
routing as an extension to server functionality. At
present, the routing technique is simple: messages
typically specify their intended destination, and
further routing constraints or destinations are chosen
by the dynamic router as each message arrives, by
matching properties of the message against the rules
base. (Some simple rules are illustrated in figure 2)
More complex routing capabilities are feasible, but
even this simple scheme allows intricate routing
behaviours and basic policy statements to be
represented.
The dynamic router is not sufficient by itself to
allow the system to respond to the type of
information policies we have been discussing.
These policy directives (implemented as routing
rules) are intended to operate across applications,
and may be related to jurisdiction, treatment, nature
of the medical event, type of information requested,
origin of the request, identity of the individuals or
organizations involved, intended use of the
information, and other policy related characteristics
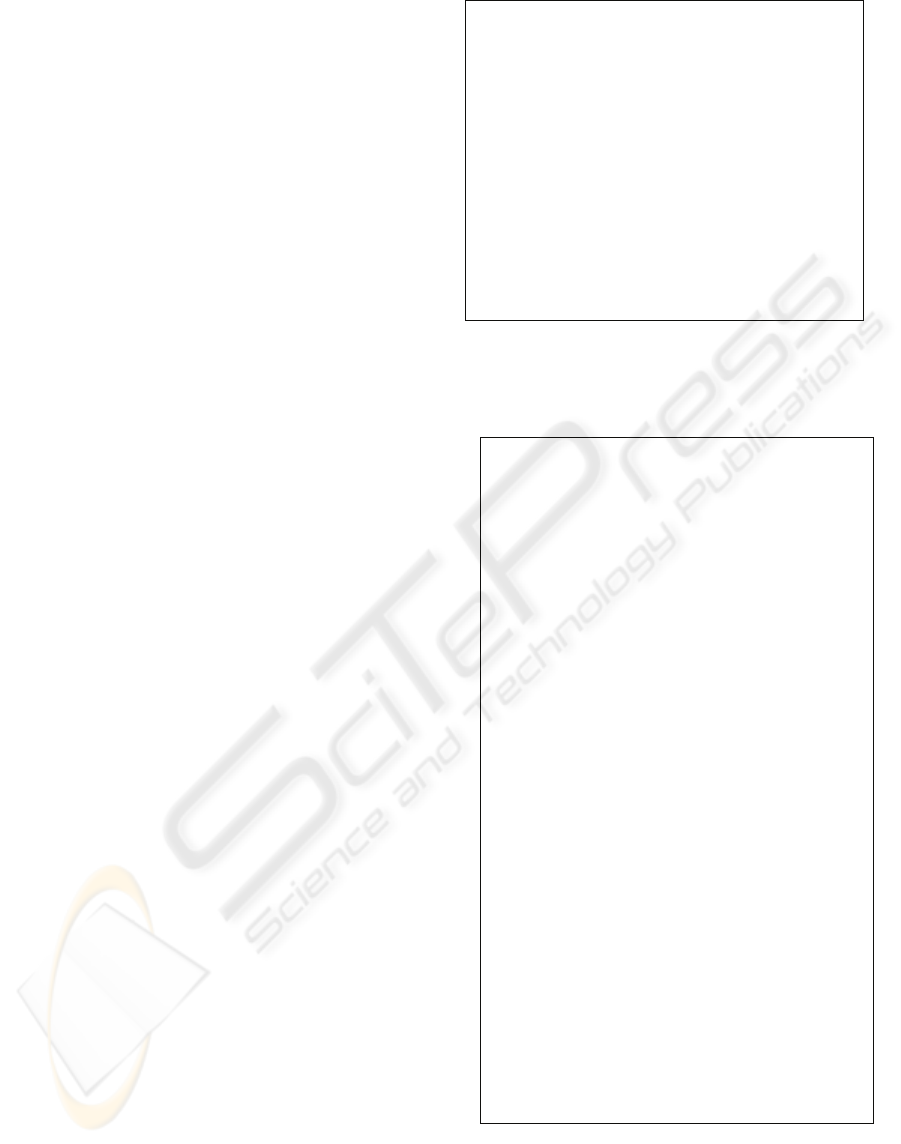
Figure 3: Messaging context affects routing.
Rules Base
Dynamic
R
Message
R
Message
Input Channel
Control
Output
Output
Output
Rules Base
Dynamic Router
Message
Enriched
Message
In
p
ut
Control
Application
Enricher Module
Remote
Services
Message
Output
Output
Output Channel
Contex
t
Client
Enrichers
Res
p
onse
Service responses are
messages
HEALTHINF 2010 - International Conference on Health Informatics
72
of the message. This additional information, which
we refer to as the medical context, must appear in a
message in order for the router to have something to
match its policy based rules. In a conventional
software deployment, some of this information (such
as intended use) would be implicit due to the
particular application being used. Under our system,
however, messages are not routed according to the
particular software application, but according to
multiple policies that apply regardless of the
particular software application in use.
2.2 Medical Context
The second critical element for policy-based
message routing is enrichment of messages to
include the medical context information that might
trigger a policy rule. Information about the source
and destination of the message, and the function of
the message in terms of data access, updates and
requests would already be included in conventional
message definition; only the medical context need be
added. Once a message arrives at the dynamic
router for delivery, the medical context for that
message is matched against the dynamic router's set
of rules, to find applicable policy rules that indicate
how the message should be routed. The router then
proceeds to deliver the message using the
communication components of the architecture.
The content enrichment module (included in
Figure 3) is used to add medical context information
to base messages. This pattern is normally used in
integration scenarios in which the message
originator does not have all the required data
available, so that additional information has to be
injected into the message. (Hohpe and Woolfe,
2003) Some of the headers deployed in our current
prototype are shown in figure 4. When applications
need to communicate, the content enricher is called
to add the medical context headers to their base
messages. As a separate code package or module,
the enrichment feature is available to all application
programmers.
Our current prototype implementation uses Java
Message Service (JMS) as the communication
infrastructure. JMS is a well supported middleware
package that provides messaging infrastructure
among multiple clients. It is a fairly simple matter
to enrich a JMS message with medical context
information, simply by adding an additional header
section to each JMS message. A simple message
header after injection in our prototype system is
shown in figure 5. The medical context header
becomes a part of each JMS message, and is carried
and delivered to routers and application code
medmsgtype: Control or Default type. Control
messages are sent to the router’s control
channel.
medcommand: Commands issued to a router.
medpolicy: A policy in the form of routing
rules.
meddrid: Healthcare provider identification.
Used by router to construct a unique output
queue.
medptid: Patient identification.
medwhere: Location of medical event (scoping
is currently unstructured).
medaction: Situational information about
medical event.
Figure 4: Some headers currently defined to inject medical
context information.
transparently by the JMS infrastructure.
{commandId = 7, responseRequired =
true, messageId = ID:jamie-
goodyearsmacbook, Local-50300-
1240760119906-0:2:1:1:1,
originalDestination = null,
originalTransactionId = null,
producerId = ID:jamie-goodyears-
macbook.local- 50300-1240760119906-
0:2:1:1, destination =
queue://Q_Default, transactionId =
null, expiration = 0, timestamp =
1240760120317, arrival = 0,
brokerInTime = 1240760120318,
brokerOutTime = 1240760120319,
correlationId = null, replyTo = null,
persistent = true, type = null,
priority = 4, groupID = null,
groupSequence = 0, targetConsumerId =
null, compressed = false, userID =
null, content = null,
marshalledProperties =
org.apache.activemq.util.ByteSequence
@f7b44f, dataStructure = null,
redeliveryCounter = 0, size = 0,
properties = {medptid=555-555-5555,
meddrid=dr.farrell.response.queue,
medmsgtype= default,
medaction=microbio-TBTestReq-sputem-
HL7-2.4, medwhere=stjohns},
readOnlyProperties = true, readOnlyBody
= true, droppable = false}
Figure 5: A JMS message header after injection of medical
context information.
These two critical architectural elements, the
dynamic router and the enriched message, are not
A FLEXIBLE POLICY ARCHITECTURE FOR MEDICAL INFORMATION MESSAGING
73

radical new architectural design concepts; in fact,
each of these elements are conventional, “off the
shelf” ideas. The dynamic router is a published and
understood enterprise integration pattern familiar to
software architects, and extended message headers is
a feature common to all electronic messaging
frameworks, including JMS. What makes our
system different is routing based on medical context
information, at a level usually limited to technical
considerations, such application, network load,
client jurisdiction or data protection.
Figure 3 illustrates the combination of the two
critical architectural elements. The medical context
enrichment must be installed at the client site where
the message originates, as this is where the context
is known; it is effectively an add-on to the
application. The dynamic router (which may be
remote or local) becomes the means for that client to
access the communications infrastructure.
3 A USE SCENARIO
Our initial implementation effort is framed as a
response to the Canadian Health Infoway Reference
Implementation Suite (CHIRIS, see CHI, 2005).
CHIRIS is intended to simulate the construction of a
cross-jurisdictional electronic health record, and
includes Admit, Dismiss, Transfer (ADT) and EHR
viewer applications. Unlike CHIRIS, our design is
conceived around medical context and messaging
rather than data access and modification. Rather
than data access or retrieval calls, we conceive of
messages as parts of a medical narrative. Handling
of these stories about patient care is defined by the
directives contained within a dynamic policy rules
base. Polices are understood as rules about how to
treat the messages that constitute the medical
narrative.
The remainder of this section traces the operation
of our prototype implementation for a particular use
case sequence, or more specifically, a particular use
of the system in which the physician consults with a
patient, updates the patient chart, and requisitions a
number of lab tests, one of which results in
diagnosis of a reportable disease. A more formal
description of the use case and its implementation
can be found in Goodyear, 2009. The following
description tracks the system operation in terms of
the medical context and dynamic router: we are not
interested in the particular application software or
screen interfaces that the various users employ, but
only in describing the messaging architecture.
Initially, the physician requests a patient record
and receives the relevant record. The message
transactions are controlled by rules in the router’s
rules base. The medical context is injected by the
software client into a message to the dynamic
router. The router, according to its rules, will pass
the message on to the patient record repository
(available as a remote service). The repository site
injects its medical context and returns the record to
the router as a response message. The response is
routed back to the requesting physician. Several
rules were involved is this exchange – the absence of
any rule to pass the messages would have caused the
data retrieval to fail.
Figure 6: All messages in the scenario are sent through a
dynamic router.
In the second portion of the scenario the
physician requisitions a chest xray. The rules base
contains an entry for xrays, so the request is
forwarded to a radiology lab. After completing the
xray procedure, the results are sent back to the
requesting physician as a response message with the
appropriate medical context injected by the lab
software site. When the response is routed, a policy
rule is matched for updating the patient record so the
lab results are automatically copied by routing a
message to the patient record repository as well as
the requesting physician. The repository responds
by sending a message notifying the primary care
physician that their patient's record has been
updated: in this test scenario, this is the same
physician that ordered the lab in the first place. The
physician receives two notifications in this scenario;
first the lab results, and second notification of the
patient record update. Rules that provide these
notifications begin to show the benefits of our
proposed architecture: in the CHIRIS reference
system notifications occur only if the application
developers program them into the application in
use. The new design allows notifications to be
routed by a simple policy rule change that
automatically affects all applications.
In the final portion of the scenario, the physician
requisitions a sputum test. The rules base contains an
entry for sputum tests, so the request is forwarded to
HEALTHINF 2010 - International Conference on Health Informatics
74

the microbiology lab. The lab results are sent back
to the requesting physician; however in our actual
test we simulated a positive result for a reportable
disease. The reportable disease is injected into the
message as part of the medical context at the lab
before the results message is sent to the dynamic
router for delivery. When this results message is
processed by the dynamic router, several rules are
matched; the physician will get immediate
notification, the patient record will be updated, and
the public health authority is notified of the
reportable disease. The physician will ultimately
receive notification of the patient record update and
an additional notification from public health that
they are aware of the test result. The notification
message from public health is also copied to the
patient repository according to another routing rule.
In this portion of the scenario, the medical context
information is used multiple times to provide
appropriate messaging. Each time a message is
passed, the rules base was consulted to provide
directives to where messages should be sent, without
any programming of the client applications. Instead,
the policy rules base provides a single consistent
source of messaging directives.
4 DISCUSSION
Our proposed design requires all client applications
and services to inject medical context into their
messaging. The test of our prototype dynamic router
involved the simulation of different health system
deployments, including the lab and record repository
services: these were simulated, not actual field
deployed systems. In practice, the messaging
facilities used by real world units would have to be
modified to include the medical context, preferably
by adding the message enrichment module to their
softwares. Our team is currently pursuing support
for a larger scale prototype and field testing of this
architecture.
There are elements of our approach that need
further design work. Most obvious is data security,
which is usually handled on an application-by-
application basis. With flexible routing of messages
with added medical context, a comprehensive
security solution which is responsive to rule changes
is needed. Part of the security solution would have
to consider to what extent a “bad actor” could hijack
the system by inserting invalid rules, similar to
server attacks currently familiar to internet service
providers. Tools to help translate medical
information policy to routing rules would be helpful
as well, including some analysis capability to
identify conflicts in policy or rules, eliminate
circularity in routing, and ensure the rules were not
used to subvert laws, security or privacy concerns.
An interesting question is how intelligent to
make the dynamic router. It could be built to make
fairly sophisticated decisions regarding conflicting
policies from different agencies or levels of
authority, to avoid or produce notification events, to
monitor and track information sharing and medical
decisions, or it could leave all important decisions to
specific human intervention. It could also apply
meta-policies about what policies can be changed or
updated.
A related question is where the dynamic router
and the rules based are physically housed. In
particular, it is interesting to consider whether a
single router with a single rules base offers
advantages in predictability and reliability (but a
single point of failure), is preferable to a distributed
system of multiple routers with multiple rule sets for
different jurisdictions and different levels of
authority.
In the meantime, our prototype system with
simulated health information services demonstrates
the technical feasibility of using a dynamic router to
implement health information policy, and realize the
advantages recited in this paper: flexible change in
information handling without the cost of redeploying
new software; explicit articulation of health
information policies, rather than implicit
enforcement by individual applications; and no risk
of being stuck with legacy software and processes
that cannot be updated to reflect organizational or
regulatory changes. Additional advantages in
traceability of medical events and decisions, largely
due to enriched medical context information, are
discussed in Goodyear, 2009.
ACKNOWLEDGEMENTS
Thanks to Dr. Gerard Farrell and the members of
Memorial University of Newfoundland's e-Health
Research Unit and Medical Informatics Group for
their support of the work herein described.
REFERENCES
Bardram. J.E., 2004. Applications of context-aware
computing in hospital work: examples and design
principles. ACM symposium on Applied computing,
New York
Bricon-Souf, N. and Newman, C.R, 2007. Context
A FLEXIBLE POLICY ARCHITECTURE FOR MEDICAL INFORMATION MESSAGING
75

awareness in health care: A review. International
Journal of Medical Informatics, 76, Elsevier
Brown, E., Wareham, H., et al., 2007. Technology
Choices and Privacy Policy in Health Care. Report to
the Privacy Commissioner of Canada, Medical
Informatics Group, Memorial University, 2007,
online: http://cpig.cs.mun.ca/TechnologyChoices
CHI, 2003. EHRS Blueprint, an inter-operable EHR
framework Canada Health Infoway Inc, version 1.0
edition.
CHI, 2005. Canada Health Infoway. CHIRIS User
Manual. Canada Health Infoway Inc, version 0.2
edition. online: http://sourceforge.net/projects/crrs.
Clercq, E.D., M. Bangels, M. and F. R. France, F.R.,
2004. Integration of electronic patient record context
with message context, Studies in health technology
and informatics, 107(2), IOS Press.
Doukas, C., Maglogiannis, I., and Karpouzis, K., 2008.
Context-aware medical content adaptation through
semantic representation and rules evaluation, IEEE
International Workshop on Semantic Media
Adaptation and Personalization, Washington.
Goodyear, J., 2009. Extending the Health Information
Access Layer with a medical context messaging
framework. Honours Dissertation. Department of
Computer Science, Memorial University of
Newfoundland.
Hägglund, M., Scandurra, I., D. Moström, D., and Koch,
S. Koch, 2007. Bridging the gap: a virtual health
record for integrated home care, International Journal
of Integrated Care 7(26), Igitur Publishing.
Hohpe, G. and Woolf, B., 2003. Enterprise Integration
Patterns : Designing, Building, and Deploying
Messaging Solutions, Addison-Wesley Professional.
Krasser, M., 2009. Introduction to the open eHealth
integration platform, online: http://
architects.dzone.com/articles/introduction-open-
ehealth, accessed July 7, 2009.
Manzoor, S., Ceusters, W.M. and Rudnicki, R., 2007. A
middleware approach to integrate referent tracking in
EHR system, American Medical Informatics
Association Symposium Proceedings..
HEALTHINF 2010 - International Conference on Health Informatics
76
