
TOWARDS AN EHR ARCHITECTURE FOR MOBILE CITIZENS
Tiago Pedrosa, Rui Pedro Lopes
Polytechnic Institute of Braganc¸a, Portugal
Jo˜ao C. Santos
Coimbra Institute of Engineering, DEE, Portugal
Carlos Costa, Jos´e Lu´ıs Oliveira
University of Aveiro - IEETA, Portugal
Keywords:
EHR, PHR, Integrated access, Security.
Abstract:
Electronic Health Records are typically created and stored in different places, by different healthcare providers,
using different formats and technology. This poses an obstacle to patient mobility and contributes to scatter
personal health related information. Patients constantly move between healthcare providers, searching for a
better service, lower prices or specialists. It is important that healthcare professionals, regardless of technology
and location, have access to the complete patient health record. The access to this personal health record can
be granted through a network (web-based, for example) or can be carried by the patient, in a usb drive, for
example. Either approach has to enforce the patient consent to access his information, cope with different
types of EHR systems and formats. This paper is an ongoing research, part of a PhD on Electronic Health
Records for Mobile Citizens.
1 INTRODUCTION
The typical medical procedure aims at recognizing a
disease or a health problem based on a set of symp-
toms and signs. To facilitate the process, the physi-
cian will try to build the diagnostic based on physical
signs and medical tests. The result of the tests, such as
blood pressure, medical imaging, electrocardiogram,
and others is information that will contribute to the
patient’s medical history, or health record, a valuable
insight for future diagnostics. In the past, this infor-
mation was paper-based, which suffered from prob-
lems such as of illegibility, unavailability, volume
of the health record during patient life, difficulty of
sharing information between the different healthcare
providers (which frequently implies duplication of in-
formation) (Rom´an et al., 2006; Coiera, 2003; Pories,
1990). Moreover, the paper-based record demands a
huge number of resources to do the routing, archiving
and maintenance of the records, for all the presented
reasons and others it can be said that the paper-based
patient record is reaching it’s limits (Uslu and Staus-
berg, 2008).
In the natural evolution of the paper-based health
record appeared the Electronic Health Record (EHR),
as an alternative to paper-based records. Different
types of EHRs exist but the most promising is the In-
tegrated Care EHR (ICEHR), that acts as a repository
of all the health information of a patient, responsi-
ble for storing, manage access to the information in
a secure away. The repository should maintain infor-
mation about the clinic history of the patient, as well
current produced information and prospective infor-
mation (Technical Committee ISO/TC 215, 2005).
The paper-based record also affects the mobility
of the citizens, increasing the problems of medical in-
formation sharing and access. The health record is
typically stored in a specific health provider, which
may cause difficulties if the patient is mobile. Mo-
bility is inevitable and proportional to the mobility of
persons, either for professional, personal or medical
reasons. Mobility exists at local, regional, national
and international scope, between public and private
healthcare providers. For creating a useful ICEHR it
is necessary to create an unique view of the scattered
health information across different providers. Hence,
288
Pedrosa T., Pedro Lopes R., C. Santos J., Costa C. and Luís Oliveira J. (2010).
TOWARDS AN EHR ARCHITECTURE FOR MOBILE CITIZENS.
In Proceedings of the Third International Conference on Health Informatics, pages 288-293
DOI: 10.5220/0002742202880293
Copyright
c
SciTePress

it is unavoidable that the different systems need to
address such challenges as a standardized logical in-
formation model, persistence of information, and as-
pects such as security and privacy of the records. At
a lower level, functional interoperability is needed for
sharing information, but a semantic interoperability
would increase the value of the solution. For achiev-
ing the semantic interoperability, the option is the
standardization of clinical concepts using terminolo-
gies, archetypes and templates. A logical informa-
tion model is being developed by organizations such
as ISO (International Organization for Standardiza-
tion), CEN ( European Committee for Standardiza-
tion), HL7(Health Level Seven) and the OpenEHR
project.
Despite these efforts, many systems are already in
use with different or without communication mecha-
nisms, they have different identification codes for the
same patient, using divergent terminology and coding
schemas.
This paper presents an access control solution that
creates an unified view of disperse patient health-care
information, allowing the achievement of the goals of
an IEHR. The developed model is supported by a cen-
tralized access control mechanism that implements
the intent consent policy when the patient can con-
trol the access to his/her personal information. More-
over, to attain the IEHR, several services gather dis-
perse health information, create an unified view of the
health record and enforce the access policy to health
professionals.
2 RELATED WORK
Different approaches on the creation of the EHRs
exists and are already being used. First, it should
be differentiated the two main streams: the Elec-
tronic Health Records (EHR) and the Personal Health
Record (PHR). They can have the same record archi-
tecture but they differ in the data custody ownership,
which has also the responsibility of manage it. The
PHR can be a self-contained registry, maintained and
controlled by the subject of care. It can be based on
a specific portable data storage, some entry in a web
service provider or even a component of an IEHR. In
the EHR case healthcare providers are responsible for
its maintenance (Technical Committee ISO/TC 215,
2005).
In this interoperability context, standardization is
the solution to enable the communication between
different systems. Several European and American
committees, country initiatives and also the World
Health Organization, are putting efforts into this goal.
These attempts pushed forward the research, but they
also brought results that evidence standards interop-
erability barriers. These efforts can be divided in two
main areas: the communication standard and the doc-
ument standard (Sunyaev et al., 2008). The former
refers how systems can communicate with each other
and the later describes how information is stored to
ensure a correct interpretation by other systems.
Several standardization results were already ob-
tained concerning health care information, some deal-
ing with data integration approach, others with data
transfer. HL7/CDA proposal copes with the commu-
nication and document needs by the different func-
tions in healthcare, from hospital information sys-
tems (HIS), radiology informationsystems (RIS), pic-
ture archiving and communication systems (PACS),
to EHR. It supports prescriptions, emergency and
administrative data. Others such as DICOM, xDT
and EDIFACT support fewer healthcare functions
but have also played important roles in specific do-
mains (Sunyaev et al., 2008). The standardization ap-
proaches are necessary for enabling communication
capability between the different institutions’ systems,
but the problem remains, i.e. the unique view of the
disperse EHR will persist. The mobility factor poses
challenges as information dispersion between differ-
ent healthcare providers’ systems increases. Even a
solution where the health records are centralized in
one place, cannot cope with mobility constraints. It
can be accepted that a national centralization of med-
ical data, at most, could exist , but a world-wide cen-
tralization is not feasible (Hasselbring, 1997). So the
information will continue to be stored in different sys-
tems bringing the need to create interoperability solu-
tions between those systems and data.
In the last decade, the use of smart-cards in health-
care information systems has been consensual, as
they provide a secure way for storing information
and authentication credentials for remote authentica-
tion (Chien et al., 2002). The Electronic Health Card
(EHC) is basically a smart-card that is used to support
information related with administrative tasks, emer-
gency medical data, security certificates and, in some
cases, e-prescriptions. This type of tokens is used in
some countries like, for instance, Germany and Aus-
tria to achieve a national IEHR solution.
As discussed, the IEHR implementations need to
provide an integrated access mechanism to disperse
information. So, the integrator system must know
the data location and, more precisely, the query en-
gine service to extract information of a specific pa-
tient. This linkage information can be stored in the
integrator database, however some projects decided
to extend electronic health card to support that ser-
TOWARDS AN EHR ARCHITECTURE FOR MOBILE CITIZENS
289

vice. Hence, the Virtual Unique Electronic Patient
Card (VU-EPR) appears as a possible solution. Costa
et al (Costa et al., 2003; Ferreira Pol´onia et al., 2005;
Carlos Costa, 2003; Carlos Costa, ) developed a VU-
EPR solution named Multi-Service Patient Data Card
(MS-PDC).
The MS-PDC is based on a token that contains
card-owner resident clinic-admin information, as well
as structured references to its distributed electronic
records. The smart card securely contains this refer-
ence, a structured data set. The association of Public
Keys Cryptographyand Crypto Smart Cards, provides
a way to securely store, transport and access the card-
owner information. Moreover,it also grants the owner
full control over the access to its data, through a PIN
and/or biometric registration.
This MS-PDC model empowers patients, enabling
the discretionary access to remote data, when crossed
VU-EPR card with health professional card, and also
allows an open access to the medical emergency data
stored in the card. It also allows the card-owner to
entitle information access levels to other users such
as the clinical professionals. The main benefits asso-
ciated to this solution can be characterized by highly
scattered geographical storage requirements.
The MS-PDC uses URLs to fetch the information
on the disperse systems and present them to the user
as a unique view. This model copes well with mobil-
ity issues, such as the gathering of disperse data and
controlling the access to it. Nevertheless, in a wider
concept of mobility it’s not feasible that all patients
will hold the same type of card world-wide. Another
discussable aspect is the physical dependency of the
card whenever exists the need to access the patient
IEHR. Many other questions can be associated with
this model like, for instance: How to retrieve data
from systems with different communication and data
standards? How can the references be dynamically
updated when new information is created, if the card
is not present? In this approach the new information
is created in EHR systems, what to do when such sys-
tem is not available?
The model, on Section 3,appears as a solution to
the problems of previous approaches in patient mobil-
ity environment.
3 RESULTS
As a result of the drop-backs identified in previous
approach, this paper proposes a model, based on the
MS-PDC concept, for coping with the special needs
of citizens’ mobility.
Since many health providersalready use EHR sys-
tems, it is proposed that those systems would continue
to be used for producingnew patient information. Our
noveltyis in the information search and display mech-
anism that uses a different solution to promote the in-
tegrated access to disperse health information. The
approach is compliant with the freedom of choice of
an EHR system by each healthcare provider. With
institutions where an information system is not avail-
able in mind, this model enables the use of a web-
based PHR (Figure 1). Hence, the proposed inte-
grated access mechanism will enable the users to have
a unique unified health record that dynamically con-
catenates all available information in the network, i.e.
EHR and web-based PHR data elements.
The display of disperse patient information in a
unique view is issued by a proxy component that will
be used for querying the remote EHR systems and the
web-based PHR (Figure 1). The proxy will imple-
ment mechanisms for understanding the remote cod-
ing, terminology and communication protocol. It will
also translate the results to a common terminology
and coding for creating the read-only unique EHR.
This proxy mechanism will be modular and will be
developed as an interface module to talk with each
type of remote EHR system. Moreover, for systems
that don’t have the ability to be queried remotely, a
broker should be deployed to enable the proxy com-
munication with that remote system. To query all the
desired information, the proxy must establish a trust
relation with every remote EHR and web-based PHR.
The authorization control responsibility will be dele-
gate to a trusted agent component (Figure 1), respect-
ing the privileges of the requesting user.
Resuming, the proxy and the trusted agent com-
ponent need to know where is the information of a
specific patient, how to retrieve it and which informa-
tion should be available for the requesting user. All
those important issues are the responsibility of a Vir-
tual Health Card System (VHCS). The VHCS is a key
component that will be explained later on this doc-
ument. The remote access to the distributed patient
information must be authorized by the patient and the
local EHR system access will continue to be managed
by the local policies of each healthcare provider.
The proposed model (Figure 1) for achieving an
Integrated Electronic Health Record (IEHR) copes
with the needs of mobile citizens. Basically the
model was developed with the goal of providing an
integrated access to the disperse health information
systems that are already stored in Electronic Health
Records, providing a read-only, unique view of pa-
tients’ IEHR.
The model will just create a new way for viewing
the information and will not create more workload for
HEALTHINF 2010 - International Conference on Health Informatics
290
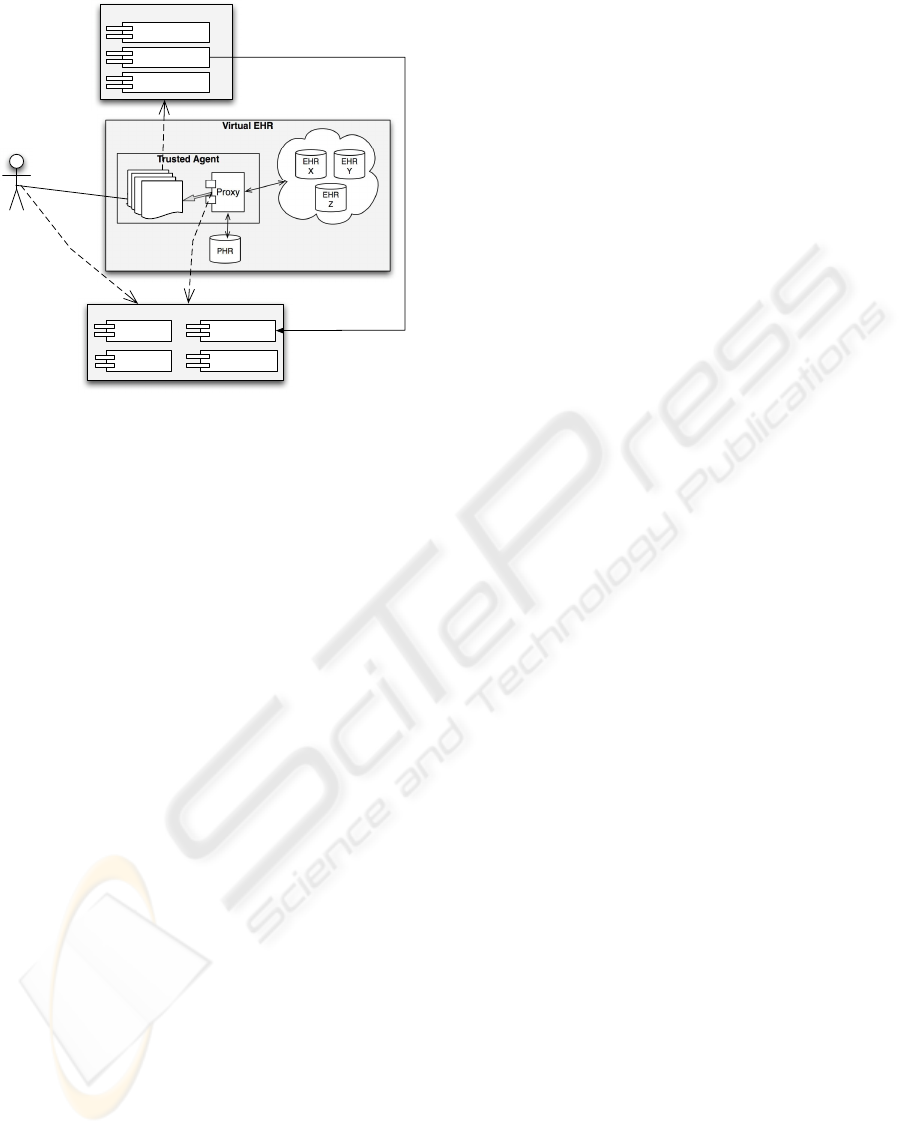
Virtual EHR
Trusted Agent
Proxy
EHR
X
EHR
Y
EHR
Z
PHR
Actor
Security Service
Authentication
Authorization
Accounting
u-EHR
Read-
Only
Virtual Health Card
Credentials
Access
Policy
UUIDs Private
UUIDs
Protected
Figure 1: EHR Architecture for Mobile Citizens.
the practitioner since he will continue to work with
his usual tools. He will only need to use a different
solution for navigation on the IEHR.
In the model, the component VHCS - Virtual
Health Card System (Tiago Pedrosa, 2009) is respon-
sible for associating the scattered EHR information
of a patient and also for providing the access control
mechanisms to the patient information. As informa-
tion resides in different organizations systems, pri-
vate and public, even in different countries, the Vir-
tual Health Card System implements the intent con-
sent of the patient to enable the access to his informa-
tion. The VHCS allows the disassociation between
the credentials used by users in system authentication
and the credentials used inside the system. For ac-
cessing his Electronic Health Card, the user will au-
thenticate himself using a token. The system is suf-
ficiently flexible to support different tokens including
the new Portuguese Citizen Card, an electronic iden-
tification card (eID card) that contains a certificate for
authentication. Moreover, if the user token or eID is
lost or stolen, the system can temporary block the ac-
cess to the Virtual Health Card until the new token
is available and associated to a patient Virtual Health
Card.
The “intent consent” consists of the patient ex-
press permission to grant the health professional ac-
cess to some part or all of his EHR. This consent en-
ables the patient to manage aspects like who can ac-
cess and what kind of information a specific health
professional can access. Basically, the patient in the
first contact with the practitioner creates an access
policy rule, including the access privileges. After this
consent the practitioner can access the patient EHR
while the access rule exists, enabling time limit to the
access period that is granted.
The model has also a ”break-the-glass” mecha-
nism that enables the bypass of the access policy,
whenever the patient is not able to provide his in-
tent consent. This mechanism will only give access
to information that is not protected in a private area.
The use of ”break-the-glass” mechanism will gener-
ate auditing records for future analysis and detection
of misconduct access.
Each patient will have his virtual health card,
this component has the patient digital credentials, the
EHR access policy and an universal unique identifiers
(UUIDs), that will act as links to the disperse informa-
tion. Each link has also complementary information
about access mechanisms (or services).
There are two types of UUIDs (Figure 1). The
UUID Private is used to handle references of verysen-
sible and discriminatory information. On this compo-
nent, the patient can manage the information that he
does not want accessible to any health professionals,
in any occasion. To enforce this behavior, the sys-
tem will cypher the references with the users corre-
spondent public-key forcing that only with the user’
private-key this information can be read. The access
to this private information demands always the ex-
plicit patient consent.
The Protected UUID is the place where other sys-
tem components (or external services) can update the
UUIDs, as new information is being produced in sev-
eral health systems. Components that, on behalf of an
authenticated and authorized user, want to access the
patient’s information, query this component to get in-
formation about remote patient data location and how
access to it.
The credential component is responsible for se-
curely storing the private and public key of the user
(Figure 1). The access to the private-key container is
only available to the authenticated user (the actor), by
the way of a secret (a password or other method (Bas-
ney et al., 2005)). The private-keyinside the container
is the credential that will be used internally for au-
thentication, signing, cypher and de-cypher the infor-
mation. This modus operandi separates the creden-
tials for authentication in the system from the cre-
dentials that the user uses to logon in other system
or components in the model.
The Security Service component (Figure 1) is re-
sponsible by the practitioner’s authentication, the au-
thorization and the accounting of requests. Hence,
each request made to the trusted agent is accounted
on this service, this will enable to audit the requests
and the creation of a report each time the ”break-the-
glass” mechanism is used. This component has also
TOWARDS AN EHR ARCHITECTURE FOR MOBILE CITIZENS
291
the critical mission to interact with the access policy
on the patient’s virtual health card in order to grant
access to the EHR to the requesting user.
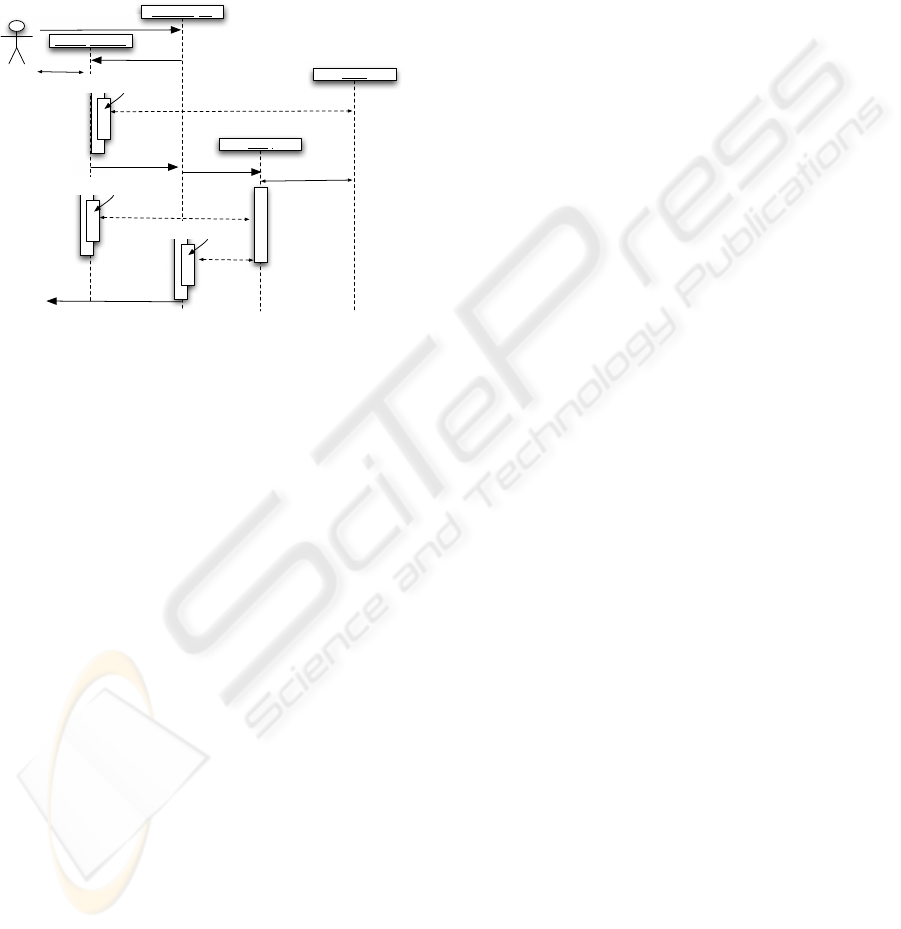
After this description of model components and
functions, we will explain in detail the procedure
steps to create a patient unique EHRs, in Figure 2 (for
simplicity, the accounting is not represented in the
figure). A practitioner, after obtaining patient intent
Security Service
Trusted Agent
Practitioner
Proxy
VHCS
GetEHR
Authenticate
Authentication
Challenge
GetEHR
Authorize ()
Get Access Policy
Authorized
Get Protected UUIDs
Authorize ()
G
a
t
h
e
r
For each UUID
Retrieve
Translate
Check Authorization
Send to Truted Agent
generate u-
EHR ()
Display EHR
Figure 2: Practitioner getting an EHR.
consent, requests the u-EHR to the trusted agent. The
Security Service will do the accounting of this request
and will also do the practitioner’s authentication in the
system. Another important feature is the authoriza-
tion, so the service will consult the access policy on
the patient virtual health card to create the EHR view
according to the practitioner privileges. However, in
emergency scenarios, the authorization process can
be bypassed using the ”break-the-glass” mechanism.
This will enable the practitioner access to all the in-
formation available in the protected UUIDS.
The next step is to gather the information stored
in dispersed EHR systems and eventually on the
web-based PHR. As previously stated in the Virtual
Health Card System exists a component-the protected
UUIDs -that works as links to the disperse infor-
mation and also informs how information should by
queried and translated to the u-EHR. This linkage in-
formation is passed to the Proxy component. Hence,
for each link the proxy will use the correspondent
module to communicate with the remote system, re-
trieve and translate the information to the u-EHR. The
retrieved information is filtered according to practi-
tioner privileges. The proxy will do this procedure
for all protected UUIDs available on the patient Vir-
tual Health Card. At the end, the trusted agent would
have available the u-EHR view corresponding to the
practitioner’s privileges. With this behaviour, only
the information in the protected UUID component is
gathered, the information that the patient considered
private is not contemplated. To enable the access to
private UUID data, the patient must explicitly request
the access to the trusted agent, i.e. given his express
consent.
Concluding, the intent consent is done by the pa-
tient directly to the VHCS. He defines, for each health
professional, the access level to his information. The
model is generic enough to allow the patient’s def-
inition of access policy or it can use a service that
defines the privileges that each category of profes-
sionals should have to the EHR. In the former, the
patient would have to create the complete access pol-
icy, defining which type of information of his EHR
the health professional could access. In the later ap-
proach, a system that maps each category of health
professionals to the type of information it should ac-
cess can be used, the patient only needs to choose the
health professional that he wants to grant access and
the category of the professional. The model can even
cope with an external service that could create the ac-
cess rules in the policy of each patient.
4 CONCLUSIONS
The proposed VHCS is an integrated access model to
disperse healthcare information. The main achieve-
ment is the implementation of a unique EHR that
copes well with requirements of mobile citizens. This
model implements the patient intent consent to enable
the sharing of sensible information between differ-
ent healthcare actors. It promotes the transparent use
of existent EHR systems in the healthcare providers.
Moreover, where a local system is not available, it
provides a web-based PHR solution to save the new
information.
The model separates the credentials used in au-
thentication from the credentials used in the indexing
system. It enables the creation of a dynamic mecha-
nism to update references of remote patient informa-
tion. It also copes with the existence of different iden-
tifiers for the same patient, along different healthcare
systems. Moreover, it empowers patients with the ca-
pability to decide what information is absolutely pri-
vate. Finally, the use of the informed consent mech-
anism respects the regulatory framework for sharing
healthcare records between distinct professionals (or
institutions) in different regions or countries.
Supplementary work should be done in research-
ing how each component should specified and devel-
oped, considering the need of high-availability and of
security. It will be also necessary to define the struc-
ture, coding and terminology used in the u-EHR.
HEALTHINF 2010 - International Conference on Health Informatics
292

REFERENCES
Basney, J., Humphrey, M., and Welch, V. (2005). The
MyProxy online credential repository. Software:
Practice and Experience, 35(9):801–816.
Carlos Costa, Jos´e Lu´ıs Oliveira, A. S. “um sistema de
integrac¸˜ao e acesso seguro a informac¸˜ao cl´ınica dis-
tribu´ıda suportada num cart˜ao de utente de sa´ude.”
(a secure and integrated access system for distributed
clinical data based on a patient card). Patent Reference
PT20040103114 20040429.
Carlos Costa, Jos´e Lu´ıs Oliveira, A. S. V. G. R. (2003).
A new concept for an integrated Healthcare Access
Model. Studies in health technology and informatics,
95:101.
Chien, H., Jan, J., and Tseng, Y. (2002). An Efficient and
Practical Solution to Remote Authentication: Smart
Card. Computers & Security, 21(4):372–375.
Coiera, E. (2003). Guide to health informatics. Arnold
London.
Costa, C., Oliveira, J., Silva, A., et al. (2003). A new con-
cept for an integrated healthcare access model. The
new navigators: from professionals to patients: pro-
ceedings of MIE2003, page 101.
Ferreira Pol´onia, D., Costa, C., and Oliveira, J. (2005).
Architecture evaluation for the implementation of a
regional integrated electronic health record. Con-
necting Medical Informatics and Bio-Informatics—
Proceedings of MIE2005—The XIXth International
Congress of the European Federation for Medical In-
formatics. Geneva: IOS Press.
Hasselbring, W. (1997). Federated integration of replicated
information within hospitals. International Journal on
Digital Libraries, 1(3):192–208.
Pories, W. (1990). Is the medical record dangerous to our
health? NC Med J, 51(1):47–55.
Rom´an, I., Roa, L., Reina-Tosina, J., and Madinabeitia,
G. (2006). Demographic management in a feder-
ated healthcare environment. International Journal of
Medical Informatics.
Sunyaev, A., Leimeister, J., Schweiger, A., and Krcmar, H.
(2008). It-standards and standardization approaches
in healthcare. Encyclopedia of Healthcare Informa-
tion Systems. Editors: Wickramasinghe, N.; Geisler,
Publisher: Idea Group.
Technical Committee ISO/TC 215 (2005). Health informat-
ics — electronic health record — definition, scope,
and context - iso/tr 20514:2005(e). Technical report,
International Organization for Standardization.
Tiago Pedrosa, Carlos Costa, J. L. O. R. P. L. (2009). Virtual
health card system. Inforum 2009.
Uslu, A. M. and Stausberg, J. (2008). Value of the electronic
patient record: An analysis of the literature. Journal
of Biomedical Informatics, 41(4):675 – 682.
TOWARDS AN EHR ARCHITECTURE FOR MOBILE CITIZENS
293
