
Semantic Sensor Networks for Personalized Health
Systems for Risk Prevention
Teresa Meneu
1
, Antonio Martínez
1
, Carlos Fernández
1
, Ainara Gonzalez
2
and Vicente Traver
1
1
Universidad Politécnica de Valencia, Camino de Vera S/N, 46022 Valencia, Spain
2
Innovalia Asociation, Rodriguez Arias 6, Dept. 605, 48008 Bilbao, Spain
Abstract. Current monitoring systems for chronic disease management and as-
sisted living are advancing with giant strides, providing more complete and per-
sonalized solutions. So far, standardization and physiological tracing strategies
have mostly overcome difficulties dealing with integration and interoperability.
However, with the deployment of massive sensing infrastructures, another big
problem appears on the scene: an enormous amount of data, coming from the
different and heterogeneous sources, and trying to describe one single scenario
or situation. This problem becomes more and more evident in we focus in the
needs of risk prevention scenarios, where the level of complexity of the targeted
indicators relays in informal and less reliable sources. This paper proposes a
new architecture for data indexing and correlation that provides a semantic
middleware to search and select relevant information from a complex and flexi-
ble monitoring scenario in a work environment. Risk prevention must look back
for trends and patterns, and furthermore, with a personalized approach. Index-
ing of semantic concepts would optimize algorithms to trigger emergency situa-
tions, provide dynamic and adaptive decision support and improving lifestyle
and care of both employees and patients.
1 Introduction
Monitoring of health related parameters, behaviors, signs and symptoms in patients
with diagnosed conditions is still a challenging issue [1]. This is evident, if not
because the need of more advanced sensing technologies, also due to the intrusiveness
and the excessive technological component of the more trivial solutions proposed.
However, the need for enhanced control and support of said patients and the
corresponding professionals makes, in many cases, the usage of less comfortable
solutions bearable for the sake of a greater good. However, this situation is brought to
the extreme when the desired scenario deals more with primary prevention,
populations at risk or promotion of healthy habits. Is in these cases where we need to
demonstrate that the role of advanced ICT technologies can and will cause a dramatic
impact in the possibilities of supporting and adapting to the evolving needs of
Meneu T., Martínez A., Fernández C., Gonzalez A. and Traver V..
Semantic Sensor Networks for Personalized Health Systems for Risk Prevention.
DOI: 10.5220/0003119200950102
In Proceedings of the International Workshop on Semantic Sensor Web (SSW-2010), pages 95-102
ISBN: 978-989-8425-33-1
Copyright
c
2010 SCITEPRESS (Science and Technology Publications, Lda.)

individuals and groups, overcoming the problems of feeling inside a continuous ‘big
brother’[2] .
Thus, technologists and professionals of health promotion and disease prevention
need to work together to create imaginative solutions that could enable that each
person is able to create his own personalized sensing environment, that provides the
right level of support, with the adequate capability for adaptability and within a
comfortable level of intrusiveness. This situation is not a utopia as it may seem, as
individuals and groups do very often reduce their level of desired privacy if they feel
within a comfortable environment or they receive positive outcomes that match their
expectations more than they feel as being controlled. In this framework, new solutions
that enable truly personalized sensor systems in not formally controlled environments
need to be proposed and validated in order to foster a new generation of personalized
health solutions. In primary prevention, this Personal Health Systems (PHS) will be
used in what in the medical world is called “uncontrolled environments”. This means
that the usual clinical golden standards (that have been set for controlled
environments) cannot be applied as such.
Nevertheless, advances need to be done in different technologies and different
layers of the architecture: in relation to the type and characteristics of the sensors
themselves, in relation to the capacity of the information processing, in the
standardization of the protocols and in the middleware. However, the aim of this paper
is to focus in the challenges and opportunities that arise from the design and
development of a middleware for advanced personalized health sensor networks for
non medicalized environments.
2 Material and Method
In between the Factory of Future (FoF) and the Internet of the Future (IoF) paradigms,
healthcare and risk prevention have arisen as key points for contribution to
development and competitiveness in Europe [2] [3]. Within this scenario, Ambient
Intelligence (AmI) can play an important role when applying multimodal monitoring
by using different types of sensors and sensing procedures for both, human and
machine activity. Thus, the acquisition of information through different sources can
contribute to setting up sub-networks that provide redundancy and enable to create
more solid measurements and conclusions from “uncontrolled environments”.
Future interfaces will be able to detect behavioral patterns and changes that may
occur during the performance of daily activities, and then react as a global platform
according to these changes. Biometrical sensors are the basement of these interfaces.
Apart from a continuous monitoring, where emergency situations can be triggered out
just analyzing whether the parameters are or not into a normal range, they allow to
complement other information coming from other sensor sub-networks, trimming
down the number of freedom degrees to apply algorithms and workflows, and
improving results sturdiness.
As a matter of fact, integrated platforms or systems are not realistic in these
environments, as the level of agreement, standardization and homogenization
96

required, both at the business/political level as well as in the technical, are extremely
difficult to obtain, if not impossible. Furthermore, the more closer we get to primary
prevention the less willingly the person will renounce to his freedom to have the
‘opportunity’ to be completely spied by the system. FoF model must engage the
concept of an open solution where the different modules that build it up can be added,
discarded, replaced or updated without modifying the core, interoperating and
contributing to depict the picture of the person and his behavior. This approach can be
only affordable with a semantic based system.
Personal Health Systems (PHS) normally share a common architecture based in a
closed-loop approach, combining monitoring and feedback to different levels of care.
This model can be easily exported as the base for more open scenarios such as the
ones targeted by this paper. The main characteristics that the architecture needs to
cover are:
• The object of the monitoring are not sick patients but citizens at risk, so they
need a greater degree of freedom in relation to the number, type and
characteristic of the monitoring sensors in their personalized system.
• Not only pure health parameters need to be assessed but also behavior and
emotional characteristics of the person need to be taken into account.
• People do not normally live alone; they normally interact with other persons and
groups and many times share with them a same physical scenario for long
periods of time (at home, at work, at school).
• To be successful, business and usage models associated to these types of systems
need to be extremely efficient and low in cost, taking profit of existing
infrastructure and aligning with the personal preferences of the actors involved.
With these requirements in mind, the proposed architecture will aim at providing a
flexible setting where different types of sensors could be dynamically combined to
create an environment of knowledge where specialized algorithms could generate a
personalized response for the user. Furthermore, this same architecture, with
personalized instances and potentially different configuration of sensors, should be
useful for different members of the social unit, and for different purposes. That it’s to
say, it does not make sense that every member of the family has his own sensor for
their own risk, but that they share a common basic infrastructure and the system adapts
to the needs and preferences of each individual at the moment of interaction. Besides,
different users in the same scenario could also prefer to use a different interface or a
different sensor for a similar purpose, such as using a wireless pedometer or an iPhone
with an integrated accelerometer.
Taking into account that the sensors sub-networks are the basement of these kinds
of systems and also pretending to have as much information as possible from many
different sources, the conception and definition of an interoperable layer is essential.
When a wide range of devices and sensors, each one working with their own
communication protocols, provide heterogeneous amount of data, two problems must
be faced: data meaning and link layer.
Healthcare industry is progressively focusing on putting standards for a new era of
m-health and e-health systems. But till nowadays it is still missing the real
implementation of a full-standardized system. Nonetheless there are many companies
97

working together, in Continua Health Alliance (CHA) [4] to overcome this hurdle for
the development; but so far only a few companies offer certified devices compliant
with 11073 standard [5].
3 Architecture
The architecture model will require a semantic based middleware, which allows easy
configuration of different sensors in a dynamic way, identifies similarities and
differences and learns from the interaction with the users how to more efficiently
configure the semantic sensor network in order to match the concrete requirements of
each situation. Furthermore, each time more, these sensors will incorporate a certain
level of processing, allowing not only extracting raw data but also high level
parameters that could be directly combined in the middleware for the first automatic
level of response [7], [8]. These components, that allow to know more about small
parts of the individual’s status are identified in the proposed model as ‘software
sensors’, extending the capabilities of data acquisition to more than just physics.
These components need to be identified and connected through the middleware,
creating bigger pieces of more complex information and providing feedback ones to
the others in order to enhance their individual performance and better adapt to the
evolution of the person. The final objective will be to have a dynamic evolving and
adapting picture of the person’s status and behavior that is as close as possible to the
reality and that can be used for configuring and providing authomatized personalized
care and creating the foundations of decision support systems for the person itself and
his related health professionals.
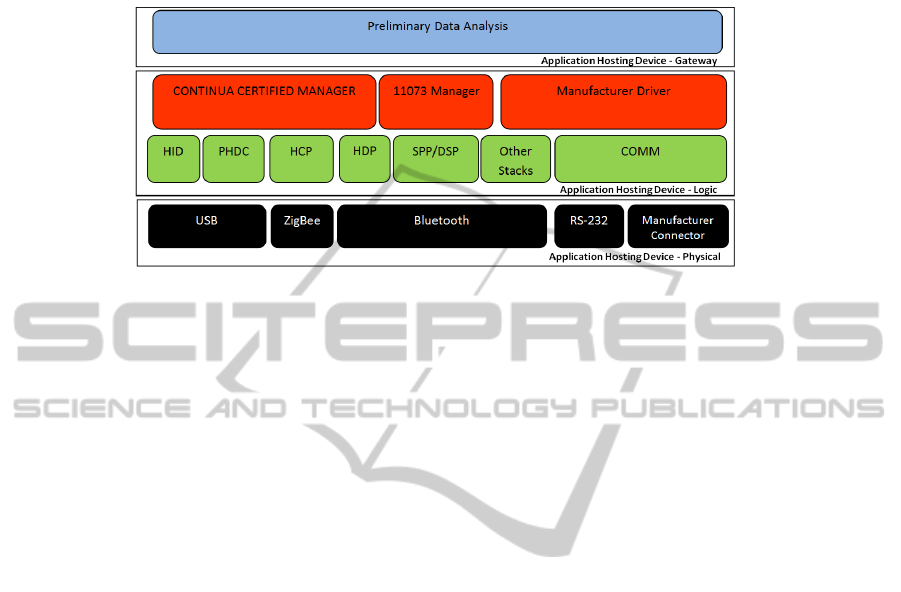
Sensor sub-networks are braked out into six different types of sub-networks, facing
the current state of art in monitoring technologies and the purpose of a holistic system.
Each sub-network is made up by an Application Hosting Device (AHD), which acts as
a manager of the sub-network, and the sensor network itself, that may be constituted
by a complex inter-dependant sensor mesh or just by an isolated sensor.
Fig. 1. Proposed Architecture for a Personal health System. Sensors are grouped into sub-
networks, where an Application Hosting Device (AHD) acts as a data concentrator and intelli-
gent gateway towards the Semantic Middleware.
98

The core of the Personal Health System (PHS) is the Semantic Middleware (SM). It
will work as an Ontology does [6] but with a human reasoning approach. The engine
within will be capable to correlate measurements arriving from different sub-networks
and perform data differential analysis to refine rules and algorithms. Data analysis will
not be more based in just working with values or conditions. New data analysis is
focused to compare a value in a context, and then analyze these contexts in order to
obtain behavior patterns and trends. In this way a fundamental topic when talking
about health prevention is covered. As a dynamic engine, new data and context
correlations can be identified, and just by an easy inquiry to the system is able to draw
a comprehensive state of the person in its concrete context.
Standards from HL7 [7] as v2.6, v3 Reference Information Model and ISO IEEE
11073 are helpful when describing health related contents and so on, for semantic
management. So far, these standards and their correspondent information models are
defined for an application special domain (i.e.: v2.6 for sending messages between
clinical entities), so there is a need to sort huge collections of data in an easy-
understandable way based in:
• Keyword (not comparable to key or ID)
• Context meaning (who, what, why, when, where)
• The value itself
Logic and rules into the semantic repository will be able to relate measurements with
contexts and also identify correlated measurements, contexts and patterns.
Therefore an environment is provided for searching and picking up information by
just describing low level aspects (for instance: employees with systolic BP greater
than 130 when they arrive at work) and above of this large libraries of indexed
metadata can be automatically fulfilled
The suitable way to stimulate interoperability and self-custom systems regarding
meta-data is the use of XML codification. CDA specifications for HL7 and CHA
Guidelines v1.5 can be taken as a reference to this kind of data storage. A useful tool
is one developed by National Institute of Standards and Technology “NIST”, the
ICSGenerator [7].
Rules and indicators which are present in the SM can be extrapolated and
optimized for specific sub-networks, and so, speeding up the process of triggering an
emergency situation.
The headmaster of the sub-network is the AHD. It defines an integrated unit split
up by three main layers: Physical layer, Logic Layer and Gateway Layer.
3.1 Physical Layer
The Physical Layer gathers all the physical interfaces the sensors offer. Following the
approach of interoperability and standards implementation, three main interfaces
defined in continua and 11073 guidelines are present: USB, Bluetooth and ZigBee.
The system may be opened also for other kind of physical interfaces such serial RS-
232 or IrDA, or even for special interfaces that manufacturers have such serial-jack.
99
As a hardware layer, the restrictions for connecting sensors may depend on the
localization of the Application Hosting Device.
Fig. 2. Application Hosting Device Stack.
3.2 Logic Layer
This Layer is conceived as a pipe. The sensor is connected to one side of the pipe and
in the other side of the pipe is expected to receive the value measured.
The main purpose of this layer is to put together the necessary classes which deal
with each physical interface and obtain the measurements. As it has been said, market
standardization is continuously facing obstacles because hardware and health sensors
companies still work with their own protocols and connection procedures. Thus, in
order to provide a transparent solution for the transport layer, independently of the
device connected, the Logic Layer will be build up by four modules:
• USB module: It will contain a Human Interface Device (HID) and Personal
Health Device Class (PHDC) libraries that will provide the basic functionalities
to initialize, maintain and close the communication with USB wired sensors.
• ZigBee module: It will contain the Health Care Profile (HCP) libraries to connect
to ZigBee [8] nodes.
• Bluetooth module: Using Bluetooth hardware access libraries, such Microsoft,
Toshiba and Bluesoleil stack, and other open source solutions as 32feet, a channel
to communicate with Bluetooth sensors will be provided. Also the basic Serial
Port Profile (SSP) and Service Discovery Protocol (SDP) functionalities of the
Bluetooth 2.0 specification and the Health Device Protocol (HDP) as defined by
Continua Health Alliance are implemented within this layer.
• COMM module: For peer-to-peer communications against RS232 and IrDA
interfaces.
Above these communications functional modules, the managers will be placed,
being able to talk the same language of the sensors. Continua, 11073 and the owner
protocol for each device will be capable to send commands through each of the four
modules mentioned before.
100

3.3 Gateway Layer
The Gateway Layer is used to connect sensors sub-networks with the Semantic
Middleware above. It will be able to interconnect different networks each one
deploying its own architecture and protocols. The purpose of this layer is to turn the
measurements from the sensors (data) into values that a semantic engine can
understand (metadata)[11].
This component will be the intelligent module in the AHD, it will be capable to
detect errors in the incoming data burst, perform high level data processing to discard
irrelevant information and endow a context for the metadata routed to the Middleware.
4 Conclusions
More extensively developed semantic sensor networks need to be developed to face
the challenges and requirements of more open scenarios for health related monitoring
in personalized systems. These semantics will enable different combinations of
sensors, which could vary in time and in instantiation, incorporating more sources of
information and allowing a more efficient traceability of the person in a more
comfortable way. This scalability and flexibility needs to be supported both in the
technical level but also at the level of data fusion and data processing. The semantics
are basic to represent the complexity of the acquired parameters, reflex the relation
between concepts and measurements and provide the mechanisms for time coupling
the information in a broad sense.
In addition to this, questionnaires and the same user interaction could also be
considered as one type of sensor, allowing assessing qualitative data that is also
required to provide the most appropriate response. The incorporation and mixing of
this qualitative data with more quantitative parameters and its usage through automatic
or semi-automatic decision support systems need a strong semantic support and an
adequately defined knowledge base. This will prevent the emergency of erroneous
conclusions but it will also allow to maximize the usage of all kinds of small pieces of
information that, all together and interpreted with the correct approach, could become
the difference between a successful and efficient personalized primary prevention
strategy and a superficial one. Furthermore, this approach seems to be much more cost
effective and provides the person with a much higher degree of freedom to choose,
increasing the possibilities of sucess.
Prevention in healthcare and in the FoF model must look to the future with the
focus in evidence based medicine and co-creation of health between multiple
stakeholders outside medicalized environments. To accomplish that, a powerful and
adaptive semantic middleware on top of a scalable and flexible monitoring
infrastructure is necessary and can make a dramatic change towards a new way of
building health and preventing risks.
101

References
1. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st
Century. Washington : National Academy Press, 2001.
2. European Project PREVE – Co-funded under the 7
th
Framework Programme of Research of
the European Commission, Information and Communication Technologies Priority, ehealth
unit (www.preve-eu.org)
3. K.L. Belkic, P.A. Landsbergis, P.L. Schnall, D. Baker. Is job strain a major source of
cardiovascular disease risk? Scandinavian Journal of Work, Environment and Health
2004; 30 (2) 85-128.
4. F Kauffmann, D Drouet, J Lellouch, D Brille. Occupational exposure and 12-year spiro-
metric changes among Paris area workers. British journal of Industrial Medicine 1982; 39:
221-232.
5. Continua Health Alliance. http://www.continuaalliance.org/about-the-alliance.html
6. ISO/IEEE 11073, Personal Health Data. http://en.wikipedia.org/wiki/ISO/IEEE_11073_
Personal_Health_Data_(PHD)_Standards
7. Paolo Baronti Prashant Pillai Vince Chook Stefano Chessa Alberto Gotta Y. Fun Hu, Wire-
less Sensor Networks: a Survey on the State of the Art and the 802.15.4 and ZigBee Stan-
dards, Computer Communications, 2006, pp. 1-30.
8. Akyildiz, I. F.; Weilian Su; Sankarasubramaniam, Y.; Cayirci, E.;, A survey on Sensor
Network, IEEE Communication Magazine, August 2002, Volume 40, Issue 8, Aug. 2002
Page(s):102 - 114.
9. O. Bodenreider, J. A. Mitchell, and A. T. McCray. Biomedical Ontologies: Session Intro-
duction. Pacific Symposium on Biocomputing 10:76-78(2005).
10. HL7. Health Level Seven Standards. http://www.hl7.org (Last Access July 2010)
11. National Institute of Standards and Technology Web Page. http://xw2k.nist.gov/ medical-
devices/index.html (Last Access July 2010)
12. ZigBee Alliance. ZigBee Health Care web page. http://www.zigbee.org/Markets/ ZigBee-
HealthCare/Overview.aspx (Last Access July 2010)
13. Magedanz T. Evolution of SOA Concepts in Telecommunications. IEEE Computer, vol.
40, no. 11, 2007, pp. 46-50.
102
