
HYBRID ELECTRONIC HEALTH RECORDS
Tiago Pedrosa, Rui Pedro Lopes
Polytechnic Institute of Braganc¸a, Braganc¸a, Portugal
Jo
˜
ao C. Santos
DEE, Coimbra Institute of Engineering, Coimbra, Portugal
Carlos Costa, Jos
´
e Lu
´
ıs Oliveira
IEETA, University of Aveiro, Aveiro, Portugal
Keywords:
EHR, PHR, Mobility, Hybrid EHR.
Abstract:
The research related with digital health records has been a hot topic since the last two decades, producing
diverse results, particularly in two main types – Electronic Health Records and Personal Health Records. With
the current wider citizen mobility, the liberalization of health care providing, as well as alternative medicine,
elderly care and remote patient monitoring, new challenges had emerged. These brought more actors to the
scene that can belong to different healthcare networks, private or public sector even from different countries.
For creating a true patient-centric electronic health record, those actors need to collaborate in the creation and
maintenance of the record. In this work, the Hybrid Electronic Health Record (HEHR) is presented, describing
how information can be created and used, as well as focusing on how the patient defines the access control.
Some new services are also discussed.
1 INTRODUCTION
Digital health records has been under development on
the last two decades, focusing on two type of records
– Electronic Health Records (EHRs) and Personal
Health Records (PHRs). The EHRs were defined and
deployed mainly to cope with the requirements of the
healthcare providers without considering the patient
needs on the process. PHRs were created to enable
a more active role by the patient in the creation and
maintenance of his health record.
The idea of achieving a longitudinal patient-
centered record that can enable health professionals
to have an integrated view of the patient’s clinical
history is still an open challenge (Smith and Kalra,
2008). The liberalization brought a wide number of
actors into healthcare provisioning, offering new pro-
cedures (Chanda, 2002) (enabling the patient to have
free choice of the healthcare provider, access to new
types of complementary and alternative medicine,
among others). Also the citizen’s mobility has in-
creased, either for professional, personal or medical
reasons (EESC, 2007), leading to a huge number of
different healthcare providers, public, private, feder-
ated, isolated, from different countries. Meanwhile
the patient requires a more active role, controlling the
access to his medical information and contributing to
his record without compromising the choice of his
healthcare provider (Eysenbach, 2008).
In order to achieve a record where all the ac-
tors could collaborate, this paper describes the Hybrid
Electronic Health Record (HEHR), and how it is used
in the creation of information, access control and new
services support.
2 EHR VS. PHR
To clarify the HEHR, we begin by analysing the two
main streams of records, EHRs and PHRs. The EHR
can be described as a longitudinal storage of patient
health information generated by one or more encoun-
ters in any care delivery setting (HIMSS, 2010a). This
information may include several kinds of data such
571
Pedrosa T., Lopes R., C. Santos J., Costa C. and Oliveira J..
HYBRID ELECTRONIC HEALTH RECORDS.
DOI: 10.5220/0003167605710574
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2011), pages 571-574
ISBN: 978-989-8425-34-8
Copyright
c
2011 SCITEPRESS (Science and Technology Publications, Lda.)

as patient demographics, progress notes, problems,
medications, vital signs, past medical history, immu-
nizations, laboratory data, and radiology reports. The
EHR has the ability to generate a complete record of a
clinical patient encounter, as well as supporting other
care-related activities directly or indirectly via exter-
nal interfaces.
The information on EHRs is produced by health-
care professionals and maintained by the health-
care providers, following four types of models: the
fully federated, federated, service orientated and in-
tegrated (NCRR, 2006). Moreover, each deployment
in each country/region or federation uses different ap-
proaches under different regulatory frameworks, This,
plus the lack of a well defined standard makes inter-
operability difficult (The Lancet, 2008).
EHRs are mainly devoted to facilitate the work
and information flow between different departments
of an institution or a federation. They also try to
manage administrative information related to the ad-
mission, discharge and payments (The Lancet, 2008).
This approach excludes any patient intervention, in-
cluding the requirements analysis. In other words,
it is a solution to cope with healthcare profession-
als needs, inside a well-defined group of actors, sup-
ported by agreements between them, to share patient
clinical related information.
PHRs can be described as an lifelong tool for
managing relevant health information of an individ-
ual (HIMSS, 2010b). It promotes personal informa-
tion maintenance and may be used in a broader scope
or in more specific scenarios, such as chronic dis-
ease management. The PHR is owned, managed and
shared by the individual or a legal proxy(s).
Although different types of PHR have been devel-
oped the most relevant are: the standalone, resident in
some external store device (Santos et al., 2010), and
the web-based. The most prominent web-based PHR
are Google Health, Microsoft HealthVault and Dos-
sia. These web-based PHRs are generally based on a
central repository and on a set of core features that, in
some cases, can be extended by third-party services.
Table 1 resumes the main differences between
EHRs and PHRs. According to the definitions and the
method of deployment of those types of records, the
PHR seams to better cope with most of the needs, as it
enables the easily sharing between different actors de-
spite of their location, agreements and depends on pa-
tient approval. It also solves the problem of the infras-
tructure cost, as the patient chooses a PHR provider.
It also empowers the patient to maintain and control
the access to his medical record. One drawback is the
trust by the clinical staff on the integrity of the clinical
information.
Table 1: EHR vs. PHR.
EHR PHR
Guardian Providers Patient or a service on his
behalf
Creation of data Medical Staff Patient or exported by ser-
vices
Sharing Institutional
agreements
Patient choice
Access Control Provider Controlled by the patient
System Provider Providers External Service Provider
The EHR has the trust of the medical staff how-
ever, record sharing is difficult. It also restricts the
patient freedom of choice, since he is dependent on
the agreements that providers have in other to access
his medical information. In this scenario, the patient
is a passive actor, since he cannot contribute to his
record, and cannot control the access to his medical
information. Mobility and EHR harmonization have
been discussed previously (Pedrosa et al., 2010).
3 A NEW PROPOSAL FOR A
HYBRID EHR
The Hybrid Electronic Health Record appears as a so-
lution to overcome the problems identified previously,
enabling the free collaboration of all the actors, con-
trolled by the patient and with medical data integrity
control. The hybrid approach tries to combine the
best characteristics of the EHR and PHR, supporting
contributions from several actors, and allowing access
control by the patient, without dependency on agree-
ments between healthcare providers.
For enabling the HEHR all actors are required to
generate a report, considered as a contribution to the
EHR. Those contributions can be generated from the
already deployed systems, from user input or by spe-
cialized services. The aggregation of all contributions
results in the patient-centric longitudinal electronic
health record.
The HEHR is based in a centralized repository,
trusted by the patient, to deposit all the contributions.
The collaboration of all the actors is illustrated on Fig-
ure 1.
The access control is performed through the pa-
tient station, where he can also create contributions.
Healthcare providers, such as hospital centers, labo-
ratories and other medical centers, can contribute as
well, exporting reports from their systems or using ex-
ternal services. Every contribution must be previously
authorized by the patient. New services can manipu-
late the information as patient centered-services, e.g.
prescription alarms or other treatment alarms; scien-
HEALTHINF 2011 - International Conference on Health Informatics
572
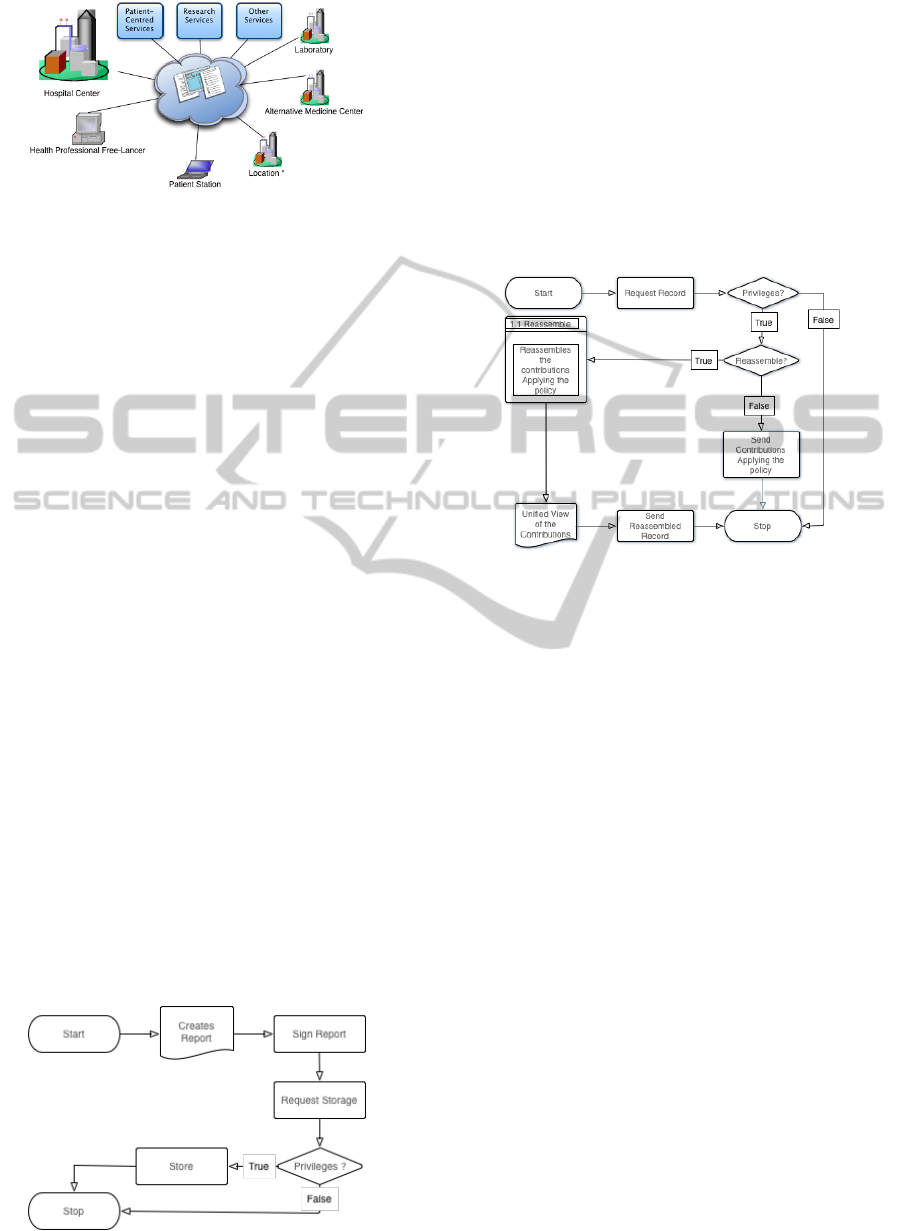
Figure 1: HEHR actors.
tific research, when allowed by the patient; and other
new services that can bring added value to the use of
patient clinic information.
Each new producer or consumer that wants to gain
access to the patient EHR requires patient authoriza-
tion. The clinical integrity of the contributions can be
confirmed, increasing the trust on the system by the
healthcare professionals.
3.1 Use Cases
On this type of record, three types of operation should
be explained: the deposit of a contribution, the request
of the record and how a new service can make use of
the HEHR.
The operation of deposit of information can be
decomposed in three steps (Figure 2). First a re-
port in a standard format, such as CDA (Dolin et al.,
2006), CCR (Ferranti et al., 2006) or OpenEHR
archetypes (OpenEHR, 2007) is generated. Then
those reports have to be signed by the producers to
ensure integrity and traceability. The last step is the
deposit of the information on a repository chosen by
the patient, if the requester has enough privileges.
Scenarios with already deployed EHR systems
should be able to generate the reports, sign and de-
posit in a seamless way. As an alternative, a local
service could perform those steps on the healthcare
provider behalf. If the provider doesn’t have a de-
ployed system, he can choose a service provider to
create the contribution.
Figure 2: HEHR store procedure.
The retrieval process is explained in Figure 3. The
actor requests the full record or parts of it. Then, the
system checks the requesters’ privileges and checks
wether the requester wants the contributions individ-
ually or assembled as a unique view. Then the pre-
viously defined policies, created by the patient, are
applied on the contributions set in order to create a fil-
tered view for the requester. The possibility of asking
for the contributions before unification allows creat-
ing custom views associated with a navigation model.
The process of requesting access to the HEHR is de-
Figure 3: HEHR retrieve procedure.
fined in two main sub processes (Figure 4): the ad-
vertisement of a new actor providing a service and
the procedure of a patient choosing a new service
provider. In the former, the new service should gen-
erate a certificate and ask a Certification Authority to
sign it. Then, the actor (services or healthcare profes-
sionals that want to deposit or access the information)
creates a description of the service, sign and register
it.
When a patient wants to use a new service, he
searches the service, chooses the provider and vali-
dates the CA signature. Then, using the public certifi-
cate of the chosen service, the patient defines the pol-
icy for that actor, controlling what the service/actor
can view or store in his record.
HYBRID ELECTRONIC HEALTH RECORDS
573

Figure 4: HEHR joining new actor.
4 CONCLUSIONS
The HEHR tries to create a true longitudinal patient-
centric electronic health record, based on contribu-
tions from all actors that provide healthcare services
to the patient. This open collaboration, controlled by
the policies specified by the patient, can deal with his
mobility and freedom of choice, since all they can
easily join as patient collaborators. The bureaucratic
sharing problem between actors is solved by the use
of the patient consent. The healthcare professionals
can trust in the clinical integrity, since it’s signature
can check all collaborations integrity.
Considering the features of the EHR and PHR (Ta-
ble 1), the HEHR can be described as a collaborative
record, which guardian is a service acting on the user
behalf. With such kind of record, it is expected the
deposit of more information, combining clinical in-
formation with other health related data, e.g. sport
activity monitoring, athletic training programs, and
other information produced by alternative medicine
procedures. Moreover, new paradigms, such as home
care, remote patient monitoring, and elderly care, can
bring added value to the patient HR.
This paper presented the difficulty that two main
streams of digital health records, EHR and PHR, have
dealing with the challenges of patient mobility, free-
dom of healthcare providers choice, and liberaliza-
tion of market. It also introduces a Hybrid Electronic
Health Record, that empowers the patient with access
control to his medical information, as enabling the ac-
cess to new healthcare services. As a result, it estab-
lishes a longitudinal patient-centered electronic health
record created by the collaboration of all the actors.
We are currently developing a framework to en-
able hybrid records, taking advantage of existing in-
terfaces between EHR and PHR. Further work in-
cludes the implementation of a storage solution and
the evaluation of data formats, such as XML serial-
ization of CDA, CCR and OpenEHR archetypes.
REFERENCES
Chanda, R. (2002). Trade in health services. Bulletin of the
World Health Organization, 80(2):158–63.
Dolin, R., Alschuler, L., Boyer, S., Beebe, C., Behlen, F.,
Biron, P., and Shabo Shvo, A. (2006). Hl7 clinical
document architecture, release 2. Journal of the Amer-
ican Medical Informatics Association, 13(1):30.
EESC (2007). Report on the implementation of the commis-
sion’s action plan for skills and mobility com(2002)
72 final. Technical report, Commission of the Euro-
pean Communities.
Eysenbach, G. (2008). Medicine 2.0: social networking,
collaboration, participation, apomediation, and open-
ness. Journal of medical Internet research, 10(3):e22.
Ferranti, J., Musser, R., Kawamoto, K., and Hammond, W.
(2006). The clinical document architecture and the
continuity of care record. British Medical Journal,
13(3):245.
HIMSS (2010 (accessed July 19, 2010)a). Himss ehr defi-
nition. http://www.himss.org/ASP/topics ehr.asp.
HIMSS (2010 (accessed July 19, 2010)b). Himss phr defi-
nition. http://www.himss.org/ASP/topics phr.asp.
NCRR (2006). Electronic Health Records Overview. Tech-
nical report, MITRE.
OpenEHR (2007). Introducing openehr - revision 1.1. Tech-
nical report, OpenEHR.
Pedrosa, T., Lopes, R., Santos, J., Costa, C., and Oliveira,
J. (2010). Towards an EHR architecture for mobile
citizens. In HealthInf 2010 Proceedings, pages 288–
293, Valencia, Spain.
Santos, J., Pedrosa, T., Costa, C., and Oliveira, J. (2010).
Modelling a portable personal health record. In
HealthInf 2010 Proceedings.
Smith, K. and Kalra, D. (2008). Electronic health records
in complementary and alternative medicine. Interna-
tional journal of medical informatics, 77(9):576–88.
The Lancet (2008). Electronic health records. The Lancet,
371(9630):2058–2058.
HEALTHINF 2011 - International Conference on Health Informatics
574
