
STUDY OF LIGHT TRANSMISSION THROUGH THE
UNDERWEAR FOR DEVELOPMENT OF A URINARY
INCONTINENCE SENSOR
Kai Ishida
1
, Toshiya Habata
2
, Akihiro Takeuchi
3
, Harukazu Tsuruta
3
,
Minoru Hirose
4
and Noriaki Ikeda
3
1
Graduate School of Medical Sciences, Kitasato University, Kitasato, Sagamihara, Japan
2
Department of Occupational Therapy, School of Allied Health Science, Kitasato University, Kitasato, Sagamihara, Japan
3
Department of Medical Informatics, School of Allied Health Sciences, Kitasato University, Kitasato, Sagamihara, Japan
4
Department of Medical Safety Engineering, School of Allied Health Science,
Kitasato University, Kitasato, Sagamihara, Japan
Keywords: Urinary incontinence, Photosensor, Dementia, Light transmission.
Abstract: Urinary incontinence is a troubling disease that makes it difficult for patients to live a normal life. Rapid
detection of urinary incontinence could allow many patients with this condition to feel more confident about
going out. Therefore, our goal is to develop a urinary incontinence detector based on a light-emitting diode
and a photodiode. Here, we describe the development and testing of a prototype model. The photosensor is
driven by a 9 V battery and consists of an ordinary electrical circuit, a light-emitting diode (lambda max =
950 nm), a photodiode (spectrum 750-1200 nm), a comparator and, a compact motor. Light transmission
through the underwear was changed by soaking with liquids. This phenomenon was measured using a
digital voltmeter. The urinary incontinence sensor was placed on a dummy. Liquids were drained into the
shorts. These increased in voltage from 3.73 V to 8.78 V, which caused the motor to vibrate. These results
show that the prototype sensor can be used to detect urinary incontinence.
1 INTRODUCTION
In recent years, Japan is rapidly becoming an aging
society. According to the report by the Japanese
Ministry of Internal Affairs and Communications, as
of August 2011, the number of elderly people in
Japan aged 65 or more was 2971 million (23.2%).
Of these, aged 65 or older women were 1702
million. It is reported that about 11 percent of
women need to have surgery related to urinary
incontinence or genital prolapse one or more times,
which means about 187 million women are applied
(Olsen et al., 1997).
In studies of epidemiology or health screening,
lower urinary tract symptoms are highly prevalent
(Homma Y, Yamaguchi O, Hayashi K, 2006; Terai
A et al., 2004). Currently, about 4 to 5 million
people suffer from urinary incontinence in Japan. It
is estimated that the number of urinary incontinence
patient will increase 10 million people after 15
years.
Cause for urinary incontinence includes, the
person who is elderly, patients with dementia,
patients who have undergone radical prostatectomy
due to cancer, patients who injured spinal cord,
patients who have schistorrhachis, females after
delivery of a baby or at the menopausal stage, and
one in four otherwise healthy women who develop
urinary incontinence. Such incontinence decreases
quality of life in various situations in society.
Patients with chronic incontinence have no urge to
urinate, and so it is difficult to use public facilities
and continue to work. For example, Spinal cord
injury (SCI) patients with normal upper body
function have a desire to return to society, but their
concern that urinary incontinence may occur at any
time often causes patients to avoid going out.
Therefore, urinary incontinence disrupts human
relationships and increases isolation, and in extreme
cases patients may commit suicide because of this
condition.
At a hospital, care facility and home, a diaper is
commonly used to prevent urinary incontinence.
311
Ishida K., Habata T., Takeuchi A., Tsuruta H., Hirose M. and Ikeda N..
STUDY OF LIGHT TRANSMISSION THROUGH THE UNDERWEAR FOR DEVELOPMENT OF A URINARY INCONTINENCE SENSOR.
DOI: 10.5220/0003741103110314
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2012), pages 311-314
ISBN: 978-989-8425-91-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)
Patients with SCI may also use intermittent self-
catheterization using a balloon catheter, and male
patients can use a condom remodeled as a urine bag.
However, these methods have several problems:
condoms remodeled as urine bags require a long
time to fit, and patients dislike wearing diapers.
Furthermore, the artificial urinary sphincter, which
is the only definitive therapy for urinary
incontinence, is not covered by the Japanese
National Insurance system and thus is uncommon in
Japan, despite its approval by the Japanese Ministry
of Health, Labour and Welfare (Arai et al., 2009).
Several sensors have been described for
prevention or detection of incontinence, including
monitoring of temperature changes in diapers
(Matsushita et al., 1993), detection of conductance
changes in diapers after incontinence (Nakajima et
al., 1994), and use of the characteristics of
radiofrequency that prevent its transmission if water
is present on clothes (Tamura et al., 2007). A device
that measures urinary volume in the bladder using
ultrasound is also on the market (Yuririn, USH-052,
Takashiba Electric Ltd., Japan, Retrieved Aug 26,
2011). However, these devices are not commonly
used in Japan. In addition, some of the reported
sensors are intended for use at the bedside for
elderly patients or patients with dementia. In
contrast, we have been unable to find a report of
practical use of a portable urinary incontinence
sensor in normal life situations. Therefore, we have
started development of a urinary incontinence sensor
that is portable, works on a battery, senses urinary
incontinence quickly, is diaper-independent, and has
a low cost.
2 METHODS
2.1 Basis and Structure of the
Incontinence Sensor
Our sensor is based on the venous needle
dislodgement sensor that we have described for use
during hemodialysis (Takeuchi et al., 2010). This
sensor utilizes light transmission through a cloth and
changes voltage after liquid osmosis. We modified
the sensor by changing the diode to emit infrared
light, adding a monitoring circuit, and using a dry-
cell battery to drive the sensor. The sensory module
consists of a light emitting diode (LED, lambda max
= 950 nm, SFH4110), a photodiode (PD, spectrum
750-1200 nm, BP104FS), and a comparator
(LM2903) with a compact motor on a simple circuit
(Figure 1). The PD changes its resistance depending
on the intensity of the transmitted light. The LED
and PD are attached at the edges of a plastic clip and
sealed with bonding to avoid a short-circuit that
could be caused by urinary incontinence (Figure 2).
The voltage across the R2 resistor (12 kohm)
increases when the light is bright and decreases
when it is dark. The voltage is not changed by
background illumination such as that from a
fluorescent lamp because the strong LED light is
directly targeted to the PD through the cloth. The
comparator receives a certain voltage from variable
resistors (Rv, 1 kohm) and R2 (variable due to light
transmission). When urinary incontinence occurs,
the R2 voltage increases to slightly higher than the
Rv voltage, and the resulting current drives the
transistor (BC373G) and causes the motor to vibrate.
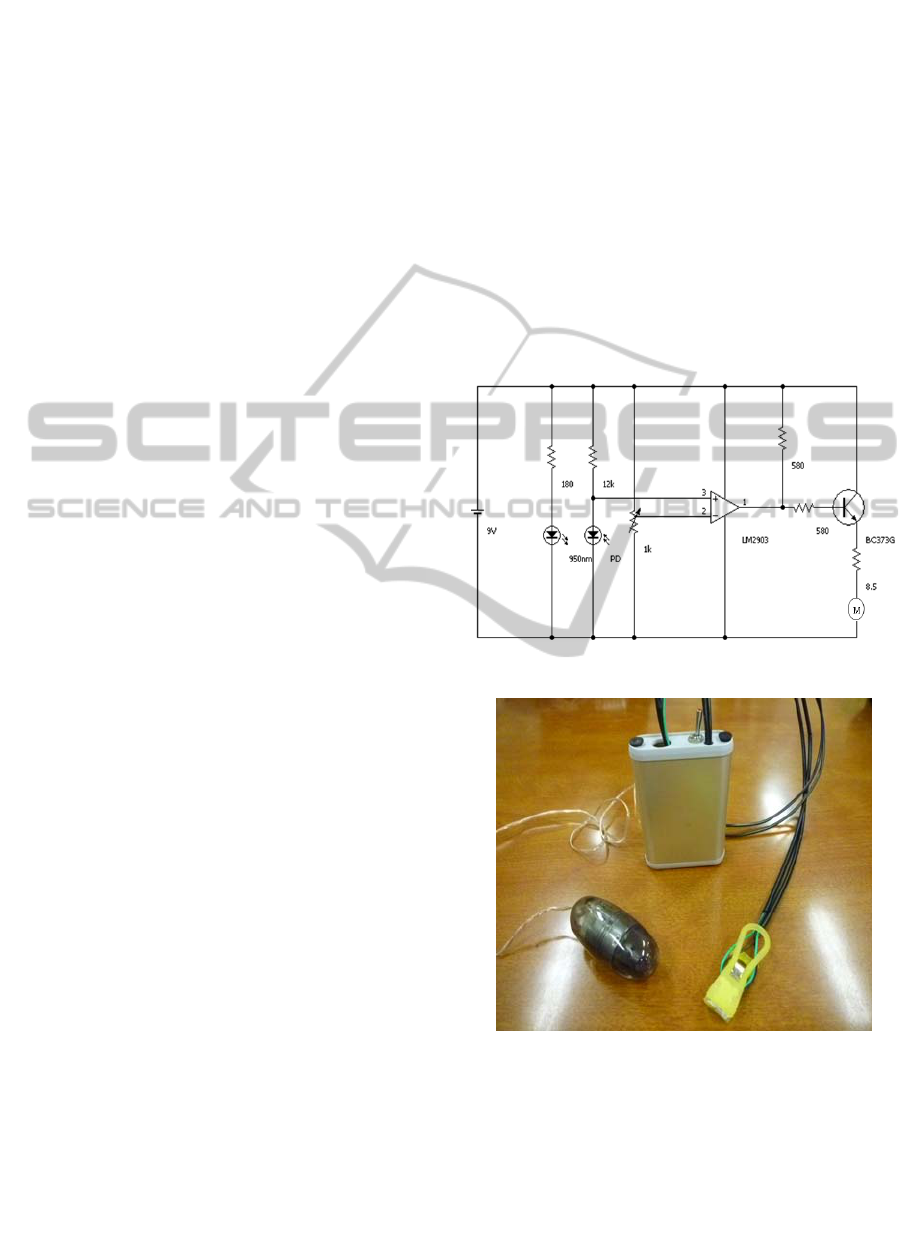
Figure 1: The circuit of the sensor module.
Figure 2: Components of the incontinence sensor.
2.2 Experimental Methods and
Statistics
First, to measure the characteristics of the sensor,
several liquids were infused and light transmission
was measured. The sensor is attached by clipping
underwear made of cotton at the bottom of the front
BIODEVICES 2012 - International Conference on Biomedical Electronics and Devices
312

surface. Infusion tube is inserted into the inner side
of the underwear (Figure 3). The liquids are infused
by the infusion pump (SYRINGE PUMP 1235N
Atom Medical., Ltd., Japan) at a rate of 200ml per
hour. Normal human urine, tap water, or
physiological saline were manually infused into the
underwear, and the R2 voltage change between dry
and wet conditions of the shorts was measured with
a digital voltmeter. We measured the interval of time
between the infusion of liquid and the beginning of
motor vibration. For each liquid, seven independent
measurements were performed. The results are
presented as a mean ± SD. A probability level of P <
0.05 was considered to be statistically significant. To
confirm the effect of thickness of the cloth on light
transmission we used three kinds of cloth with the
thickness of 0.2mm, 0.4mm and 0.6mm. We then
tested the sensor using a dummy patient that was set
to external underwear assumes incontinence may
occur (Figure 4).
3 RESULTS
With a dry underwear, the mean voltage across R2
was 3.58 ± 0.12 V under control conditions. The
threshold of the comparator was set at about 8 V by
adjusting Rv. Infusion of liquid to wet the underwear
caused the R2 voltage to increase from 3.73±0.41V
to 8.78±0.31V with unimpaired urine, from 8.78 ±
0.11 to 5.9 ± 0.06 V with tap water, and from 3.46±
0.13 to 9.08 ± 0.05 V with physiological saline. In
all cases, the values after liquid infusion were
significantly higher (P<0.01) than the Rv voltage
which caused the motor to vibrate about 4.5 to 6
seconds after the liquid was infused (Figure.5).
Figure 3: Positioning of the sensor and infusion tube.
By the experiment that changed thickness of
cloth, the R2 voltage increased from 5.7± 0.2 to
8.38±0.07V with 0.2mm cloth, from 3.41±0.2V to
7.96±0.3V with 0.4mm cloth, and from 1.92±
0.12V to 6.47±0.31V with 0.6mm cloth (Figure 6).
In all cases, the changes were statically significant
(P<0.01).
Similarly, in testing on the dummy patient, the
motor vibrated a few seconds after infusion of tap
water.
Figure 4: Experimental dummy showing the positioning of
the sensor.
Figure 5: Effect of liquid type on the R2 voltage.
Figure 6: Effect of thickness of cloth on the R2 voltage.
4 DISCUSSION
The prototype sensor described in this work is
compact, works on a battery, is suitable for use at
the bedside and outside the house, and has a low cost
because the sensor is washable and sterilizable. Our
STUDY OF LIGHT TRANSMISSION THROUGH THE UNDERWEAR FOR DEVELOPMENT OF A URINARY
INCONTINENCE SENSOR
313

results show that the sensor can respond to a small
amount of urine, which allows detection of
incontinence before a flood of urine occurs. We
think this sensor is suitable for patients with
dementia, patients use a wheelchair such as SCI
patients, and training for young patients with
enuresis. With use of the sensor, younger patients
will be able to avoid wearing diapers and can choose
to wear any type of shorts. Soaking of the shorts due
to incontinence will drive vibration of the motor, and
positioning of the motor on the normal upper body
will allow the patient to detect incontinence at an
early stage.
From the results, we confirmed that the light
transmission through the cloth increased
significantly by human urine, tap water and physical
saline. When the thickness of the cloth was 0.4-
0.6mm, the R2 voltage increased by more than 4V.
This indicates that adjusting Rv resistance and
setting the threshold properly, this sensor is
applicable to detecting urinary incontinence.
In this study we used the underwear made of
cotton. The motor vibrated even when the sensor is
attached at the thickest position. If we adjust the
variable resistors and control threshold voltage,
different type of underwear can be used. In the
experiment, we used dummy patient, but for
practical use it will be necessary to examine the
effects of walk and roll-over, etc. Therefore, as the
next step in development of the sensor, we will work
toward its practical use through testing and
evaluation in a patient with urinary incontinence.
5 CONCLUSIONS
In this article, we described development of a
urinary incontinence sensor, which utilized light
transmission through cloth. This sensor is compact,
works on a battery, can be used at the bedside and in
ordinary life, and frees the patient from wearing a
diaper.
REFERENCES
Olsen A L., Smith V J., Bergstrom J O., Colling J C.,
Clark A L., 1997. Epidemiology of urgical managed
pelvic organ prolapsed and urinary incontinence.
Obstet Gynecol, 89, 501-506.
Homma Y., Yamaguchi O., Hayashi K., 2006.
Epidemiologic survey of lower urinary tract symptoms
in Japan. Urology, 68, 560-564.
Terai A., Matsui Y., Ichioka K., Ohara H., Terada N.,
Yoshimura K, 2004. Comparative analysis of lower
urinary tract symptoms and bother in both sexes.
Urology, 63, 487-491.
Arai Y., Takei M., Nomura K., Baba S., Habuchi T.,
Matsuda T., Takahashi S., Igawa M., Kaiho Y.,
Nakagawa H., 2009. Current use of the artificial
urinary sphincter and its long-term durability: A
nationwide survey in Japan. Int J. Urology, 16, 101-
104.
Matsushita T., Tamura T., Fujimoto T., Nakano T., 1993.
Diaper Sensor for Monitoring Urinary Incontinence.
Jpn. J. Medical Electronics and Biological
Engineering, 31, 29-35.
Nakajima K., Tamura T., Miike H., Shimooki S., Fujimoto
T., Nakano T., 1994. Disposable Diaper with Urinary
Incontinence Monitor. Jpn. J. of Medical Electronics
and Biological Engineering, 32, 15-23.
Tamura S., Shibata M., Nagata H., Nogawa H., Tanaka H.,
2007 RFID as Water Sensor. Jpn. J. Medical
Informatics, 27, 127-131.
Yuririn USH-052 urinary volume data recorder. Retrieved
Aug 26, 2011, http://www.yuririn.jp/,
Takeuchi A., Ishida K., Morohoshi Y., Shinbo T., Hirose
M., Ikeda N., 2010. Study of light transmission
through gauze pad effected by blood or liquids to
detect needle dislodgement. J Clin Monitoring and
Computing, 24, 35-39.
BIODEVICES 2012 - International Conference on Biomedical Electronics and Devices
314
