
TOWARDS WEARABLE AND CONTINUOUS 12-LEAD
ELECTROCARDIOGRAM MONITORING
Synthesis of the 12-lead Electrocardiogram using 3 Wireless Single-lead Sensors
C. P. Figueiredo and P. M. Mendes
Centro Algoritmi, University of Minho, Dep. Industial Electronics, Campus Azurém, 4800- 058 Guimarães, Portugal
Keywords: Health Monitoring Devices, Biotelemetry, Wireless Systems, Wearable Systems, 12-lead ECG Synthesis,
12-lead ECG Reconstruction, Low-Power Design.
Abstract: Wearable health monitoring systems have emerged in the last decade as innovative means for patient
observation and healthcare delivery. Among the physiological signals which can be measured using such
systems, the 12-lead electrocardiogram is arguably the most important. However, continuous monitoring of
the standard 12 lead electrocardiogram is impractical and unattractive for a wearable system, due to the
obtrusiveness and discomfort that the placement and connection of 10 electrodes would cause. In this
regard, the use of reduced lead sets for the synthesis of the 12-lead electrocardiogram is a preferable
solution. This work analyses the suitability of a wireless sensor network prototype for continuous and
simultaneous monitoring of a set of 3 modified electrocardiogram leads, which can be used for synthesis of
the 12-lead electrocardiogram by application of a patient-specific transformation matrix, estimated by
multiple linear regression.
1 INTRODUCTION
The development of wearable systems for health
monitoring has, since the last decade, been an active
research topic with growing attention (Pantepoulos
and Bourbakis, 2010), benefiting from the recent
advances in sensor and communication technologies,
along with their increasing degree of miniaturization
due to microelectronic integration. These systems
have been shown to have the potential to
revolutionise healthcare systems, which are
currently under increasing pressure, due their rising
global costs, ageing of the population and associated
prevalence of chronic disease (Hao and Foster,
2008). In this sense, the promotion of a shift in
healthcare systems from reactive management of
illness towards proactive management of wellness is
desired (Milenković et al., 2006), supported by
innovative, affordable and efficient solutions for
personal health monitoring. Many other benefits are
envisioned through the widespread availability of
these solutions for both patients and caregivers. The
quality of life and mobility of monitored patients is
increased and the means for detection of early signs
of disease are improved by long-term continuous
monitoring (Nield et al., 2004). These allow for
patients to keep an independent lifestyle in their
environment of choice and for caregivers to provide
better treatment and prevent further complications.
Among the different physiological signals which
can be continuously measured with health
monitoring systems, in order to evaluate the health
condition of a person, the 12-lead electrocardiogram
(ECG) is arguably the most important, since cardiac
disease is the leading cause of death and disability in
the world. The 12-lead ECG is considered as the
gold standard for non-invasive detection of
abnormal cardiac rhythms and cardiac diseases such
as myocardial ischemia. However, continuous
monitoring of the full set of 12 leads of the standard
ECG, and the placement of the respective electrodes
at their standard locations (which include the distal
extremities of the limbs), is unattractive and
incompatible with the design requirements of a
wearable system for health monitoring, namely
unobtrusiveness, comfortable use and user-
friendliness. Therefore, most of the wearable health
monitoring systems proposed to date are only able to
monitor a single lead or a lead subset (e.g. 3-lead
ECG composed only of Einthoven leads) of the
standard 12-lead ECG (Pantepoulos and Bourbakis,
2010), and thus only a limited interpretation of the
329
P. Figueiredo C. and M. Mendes P..
TOWARDS WEARABLE AND CONTINUOUS 12-LEAD ELECTROCARDIOGRAM MONITORING - Synthesis of the 12-lead Electrocardiogram using 3
Wireless Single-lead Sensors.
DOI: 10.5220/0003771203290332
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2012), pages 329-332
ISBN: 978-989-8425-91-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

electrical activity of the heart is obtained. This
limitation can be critical for the sensibility of the
ECG monitoring system on the detection of certain
cardiac abnormalities, e.g., ischemic episodes may
be only visible in part of the 12 standard ECG leads
and may be overlooked (Klootwijk et al., 1998),
even during continuous monitoring. Moreover,
caregivers could perform more efficiently if the
health monitoring system could provide them with
the ECG signal in the same fashion in which they
were trained to analyse, i.e., the standard 12-lead
ECG.
Due to the conflicting design requirements
concerning wearable and continuous monitoring of
the 12-lead ECG, solutions are needed to allow
monitoring the full set of 12 ECG leads, while
simultaneously minimising the obtrusiveness of the
monitoring system. On this subject, several authors
have proposed and studied the synthesis of the 12-
lead ECG using reduced lead sets, based on the
application a generic or patient-specific
transformation matrix, estimated through multiple
linear regression, to the lead signals of the reduced
lead set (Dower et al., 1988; Nelwan et al., 2004).
The synthesis of the 12-lead ECG using wireless
technology was proposed by Trobec and Tomašić
(2011), based on a set of 3 differential leads formed
by pair of proximal electrodes. However, the impact
caused by the use of wireless communications in the
performance of the synthesis algorithm was not
analysed. In this regard, this work aims to analyse
the suitability of a developed wireless network
prototype, consisting of 3 wearable single-lead ECG
sensors, for application in 12-lead ECG synthesis.
The quality of the acquired lead signals is evaluated,
as well as the issues caused by the wireless
transmission of these independent signals, such as
reliability (transmission errors leading to loss of
information) and synchronization between nodes.
2 SYSTEM OVERVIEW
The currently proposed system is illustrated in
Figure 1, and it has the aim of enabling continuous
monitoring of a synthesised 12-lead ECG. It can be
seen that the proposed solution is based on a
wireless network of three wearable single-lead ECG
sensors, placed at different locations and orientations
on the chest of the monitored patient. In addition, a
coordinating node is used to receive the signals
acquired by each of the 3 single-lead ECG sensors,
and to forward them via USB connection to a
personal computer where the 12-lead ECG is
synthesized and displayed. The use of these
Figure 1: Proposed wireless network of wearable sensors
for continuous monitoring of a synthesised 12-lead ECG.
wearable single-lead ECG sensors, combined with
the use of wireless technology and an algorithm for
12-lead ECG synthesis based on independent local
lead signals, has allowed the design of a wearable
12-lead ECG monitoring system featuring total
absence of wired connections, such as electrode lead
wires, and which also does not require the monitored
leads to be referenced to the same ground.
The synthesized 12-lead ECG is calculated on a
personal computer, from the independent single-lead
ECG signals obtained by the 3 sensors in the
network, using the following linear equation:
L
i
= M
i0
+ M
i1
l
node 1
+ M
i2
l
node 2
+ M
i3
l
node 3
(1)
where L
i
indicates the amplitude of synthesized lead
i (i = 1, …, 12 or {I, II, III, aVR, aVL, aVF, V1, …,
V6}), l
node j
indicates the amplitude of the lead signal
at node j (j = 1, 2, 3) and M
ij
is the transformation
matrix filled with patient-specific coefficients,
estimated using multiple linear regression to fit the
model shown in (1) to a dataset of a previously
measured standard 12-lead ECG (dependent
variable) and the three single-lead ECG signals
(independent variables) (i = 1, …, 12 and j = 0, ...,
3).
Concerning the currently presented approach, it
can be noticed from Figure 1 that the wearable
single-lead ECG sensors are centred on V2 and that
their monitored local leads are oriented towards the
proximal extremities of the limbs. This configuration
was selected based on existing evidence that the 12-
lead ECG can be synthesized with a fair degree of
accuracy (cross correlation coefficients greater than
0.9) using a 3-lead subset composed of leads I, II
and V2 (Atoui et al., 2010; Nelwan et al., 2004),
even if the Mason-Likar modification of the standard
12-lead ECG is used for the reduction of motion
artefacts. The position of each single-lead ECG
sensor on the chest of the monitored patient can be
moved along the directions indicated by the dashed
lines shown in Figure 1, to increase the accuracy of
the synthesised ECG or to increase user comfort, as
long as these positions are kept constant between
BIODEVICES 2012 - International Conference on Biomedical Electronics and Devices
330
different monitoring sessions of each particular user.
3 WEARABLE SINGLE-LEAD
ECG SENSOR
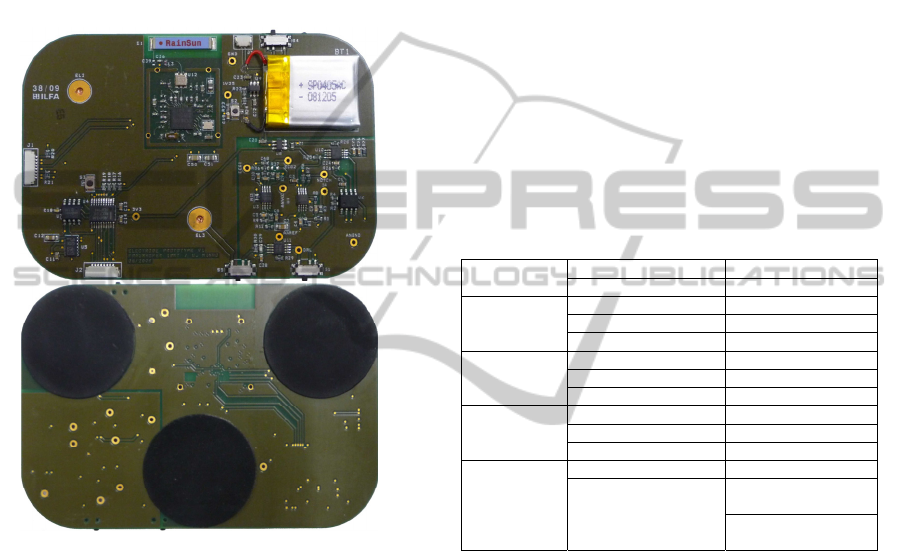
Each single-lead ECG sensor within the wireless
network is similar and the appearance of their first
prototype (Figueiredo et al., 2010) is shown in
Figure 2.
Figure 2: Top and bottom views of the developed wireless
sensor node for monitoring of a single modified ECG lead.
The wearable sensor shown in Figure 2 consists
of a flexible printed circuit board containing built-in
flexible dry electrodes (Steltenkamp et al., 2009) on
its bottom layer, which is intended to contact the
surface of the chest of the monitored patient. These
electrodes do not require skin preparation before use
and are therefore suitable for a wearable system. The
top layer contains low-power electronics for signal
acquisition, processing and wireless communication,
making use of commercial off-the-shelf components.
The design of these sensors meets the requirements
for a wearable system for health monitoring such as:
small dimensions, light weight, wireless
communication and low power consumption.
The wireless communications between the
single-lead ECG sensors and the coordinating node
are based on proprietary wireless transceiver and
MAC Protocol (Omeni et al., 2008), which operates
at the non-crowded 862-870 MHz radio band, and
uses a master-slave architecture with collision
avoidance and a Time Division Multiple Access
(TDMA) scheme. These features not only provide
error resilient and low power wireless
communication, but also help to keep synchronism
between the data transmitted from the different
sensor nodes, since the network coordinating node
periodically requests data from each sensor node in
succession, and only one sensor node is transmitting
at a time.
Besides monitoring of a local ECG lead, the
wireless sensor nodes also include a triaxial
accelerometer and a thermistor for activity and
temperature monitoring. Table 1 summarizes the
specifications and features of the developed
wearable single-lead ECG sensors (Figueiredo et al.,
2010).
Table 1: Summary of the specifications and features of the
developed wearable single-lead ECG sensors.
Wireless link
Operation frequency 862-870 MHz
Data rate 50 kbps
ECG lead
monitoring
Gain 500
Resolution 11 bits
Sampling Frequency 250 samples/s
Triaxial
accelerometer
monitoring
Range ± 2g or ± 8g
Resolution 8 bits
Sampling Frequency 400 samples/s (max.)
Temperature
monitoring
Range 20 ºC to 40 ºC
Resolution 11 bits
Sampling Frequency 250 samples/s
Power
consumption
Supply voltage 3.3 V (minimal)
Average current
consumption
0.98 mA
(ECG mode)
1.43 mA (ECG +
accelerometer mode)
4 RESULTS
4.1 Measurement of Single-lead ECG
Signals
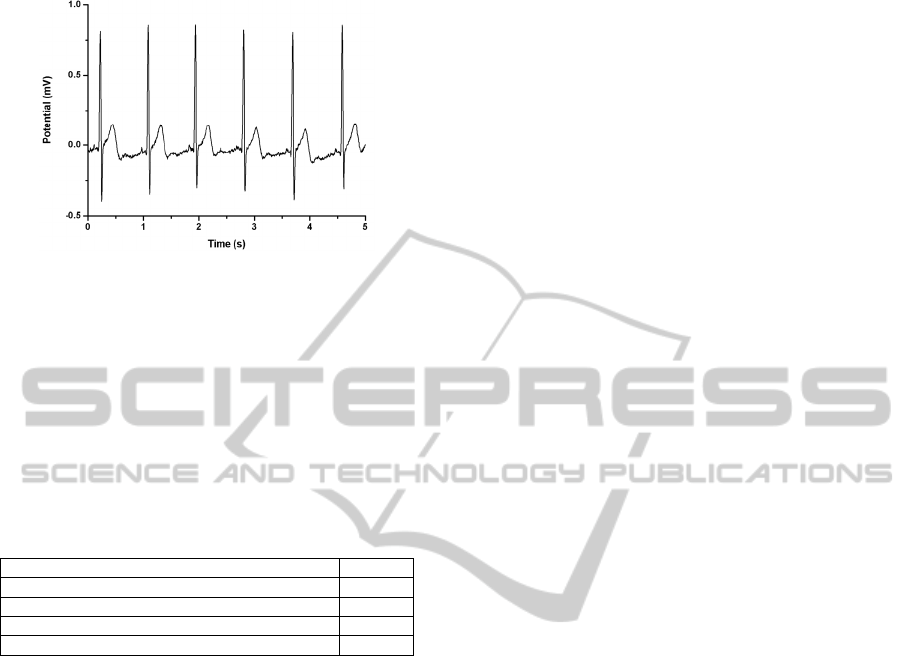
A five second period of a modified ECG lead,
obtained by the developed single-lead ECG sensor is
shown in Figure 3. The obtained signal has suitable
quality and signal to noise ratio for the intended
ECG monitoring application, allowing different
features of the ECG signal to be detected, such as
the QRS complex, T wave and the ST interval.
4.2 Wireless Link Performance
The reliability of the wireless communications
between the sensor nodes and the network
coordinating node was tested by evaluating the
TOWARDS WEARABLE AND CONTINUOUS 12-LEAD ELECTROCARDIOGRAM MONITORING - Synthesis of the
12-lead Electrocardiogram using 3 Wireless Single-lead Sensors
331
number of communication errors occurred over time.
Figure 3: ECG lead signal acquired by the developed
wearable sensor.
Table 2 shows a list of different statistics obtained
during a testing period of one hour, within which the
3 wireless sensor nodes were performing signal
acquisition and transmitted their monitored data
when requested by the network coordinating node,
following a TDMA communication scheme.
Table 2: Statistics of error performance in wireless
communications within the developed network, during a
testing period of one hour.
Connection losses 2
Packets lost due to link errors 60
Duplicate packets received 10
Total number of generated packets/TDMA slots 1383
Packet error rate 5.1%
The obtained packet rate of 5.1% is considerable,
although it could be acceptable for continuous long-
term monitoring applications, where loss of data is
less critical.
5 CONCLUSIONS
From a preliminary analysis of the developed
system, it is expected that the use of a wireless
network of single-lead ECG sensors, using a
protocol based on TDMA and operating in a less
crowed band, could provide reliable support for
continuous monitoring of independent single-lead
signals and for continuous 12-lead ECG synthesis.
Future work will involve testing of the accuracy
of the proposed system for 12-lead ECG synthesis in
volunteers and the development of a new
miniaturised version of the single-lead ECG sensors.
Moreover, tests should be performed to evaluate up
to what degree the data losses caused by errors in
wireless communications affect the accuracy and the
performance of the system for continuous
monitoring of a synthesized 12-lead ECG.
ACKNOWLEDGEMENTS
This work was supported by the Portuguese
Foundation for Science and Technology under grant
SFRH/BD/40341/2007.
REFERENCES
Atoui, H., Fayn, J., Rubel, P., 2010. A Novel Neural-
Network Model for Deriving Standard 12-Lead ECGs
From Serial Three-Lead ECGs: Application to Self-
Care. IEEE Trans. Inf. Technol. Biomed., 14(3),
883-890.
Dower, G. E., Yakush, A., Nazzal, S. B., Jutzy, R. V.,
Ruiz, C. E., 1988. Deriving the 12-lead
electrocardiogram from four (EASI) electrodes. J.
Electrocardiol., 21, 182-187.
Figueiredo, C. P., Becher, K., Hoffmann, K.-P., Mendes,
P. M., 2010. Low Power Wireless Acquisition Module
for Wearable Health Monitoring Systems. Proc. 32nd
Ann. Int. IEEE EMBS Conf., 704-707.
Hao, Y., Foster, R., 2008. Wireless body sensor networks
for health-monitoring applications. Physiol. Meas., 29,
R27-R56.
Klootwijk, P. et al., 1998. Comparison of usefulness of
computer assisted continuous 48-h 3-lead with 12-lead
ECG ischaemia monitoring for detection and
quantitation of ischaemia in patients with unstable
angina. Eur. Heart J., 18(6), 931-940.
Milenković, A., Otto, C., Jovanov, E., 2006. Wireless
sensor networks for personal health monitoring: Issues
and an implementation. Comp. Commun., 29,
2521-2533.
Nelwan, S. P., Kors, J. A., Meij, S. H., Bemmel, J. H. v.,
Simoons, M.L., 2004. Reconstruction of the 12-lead
ECG from Reduced Lead Sets. J.Electrocardiol., 37,
11-18.
Nield, I., Heatley, D. T. J., Kalawsky, R. S., Bowmann, P.
A., 2004. Sensors Networks for Continuous Health
Monitoring. BT Technol. J., 22(3), 130-139.
Omeni, O. C., Eljamaly, O., Burdett, A. J., 2007. Energy
Efficient Medium Access Protocol for Wireless
Medical Body Area Sensor Networks. Proc. 4th IEEE-
EMBS Int. Summer School & Symp. Medical Devices
and Biosensors, 29-32.
Pantepoulos, A., Bourbakis, N. G., 2010. A Survey on
Wearable Sensor-Based Systems for Health
Monitoring and Prognosis. IEEE Trans. Syst., Man,
Cybern. C, Appl. Rev., 40(1), 1-12.
Steltenkamp, S., Becher, K., Doerge, T., Ruff, R.,
Hoffmann, K.-P., 2009. Electrode structures for
acquisition and neural stimulation controlling the
cardiovascular system. Proc. 31st Ann. Int. IEEE
EMBS Conf., 5478-5481.
Trobec, R., Tomašić, I., 2011. Synthesis of the 12-Lead
Electrocardiogram From Differential Leads. IEEE
Trans. Inf. Technol. Biomed., 15(4), 615-621.
BIODEVICES 2012 - International Conference on Biomedical Electronics and Devices
332
