
EVALUATION OF A MATERNAL AND CHILD ELECTRONIC
HEALTH RECORD IN A DEVELOPING COUNTRY
Preliminary Results from a Field Pilot
Martins Mupueleque
1,3
, Juliano Gaspar
1,2
, Ricardo Cruz-Correia
1,2
and Altamiro Costa-Pereira
1,2
1
CIDES – Department of Health Information and Decision Sciences, Porto, Portugal
2
CINTESIS – Center for Research in Health Technologies and Information Systems, Faculty of Medicine
University of Porto, Porto, Portugal
3
Faculty of Health Sciences, University of Lúrio, Nampula, Mozambique
Keywords: Maternal and child health, Childbirth, Information systems, Electronic health record (EHR), Data quality,
Mozambique, Africa.
Abstract: Introduction: The poor quality of health indicators data such as maternal and perinatal mortality prevents an
adequate planning and evaluation of public health interventions.
Objective: To evaluate the viability and usability of a prototype of a maternal and child electronic health
record, in Northern Mozambique.
Methods: The prototype was based on existing paper forms and the system was assessed at a maternity ard
in a healthcare center of Nampula. The usability was evaluated using in loco observations, interviews and
self-administered questionnaires to health professionals, after a 6 hours training period.
Results: During the evaluation period, 205 clinical forms were registered, corresponding to 58% of all
childbirths. From a total of 19 health professionals, 9 nurses answered the questionnaire. The prototype was
well accepted among these respondents but the recording time was higher than in its paper version (12 vs. 5
minutes per record). Data quality problems were identified. The absence of a unique citizen identifier was a
major obstacle regarding the mother-child data linkage.
Conclusion: Although this system may contribute to the improvement of the quality of the healthcare
provided to women and children in Mozambique, there are still many technical and organizational
challenges to be overcome.
1 INTRODUCTION
Approximately 11 women die every day in
Mozambique, adding up to 3.900 deaths in 2009,
from complications related with pregnancy and
childbirth. For every 1.000 live births, about 48
children die in the first 28 days of life every year,
mainly from complications occurring during
pregnancy and childbirth, including inadequate
home practices (2009a).
Nampula is a province in the Northern part of
Mozambique, covering an area of 78.197 km
2
, with
almost 4 million inhabitants, mainly farmers with
little education and strong ties to a traditional
medical system.
The inadequate infrastructure of Mozambique,
such as communication and transportation networks,
access roads, electricity, data processing equipment
and Internet, complicates the accessibility to
information, both paper-based and electronic (2007;
2008; 2009b).
During the research and the analysis of reports
regarding the Mozambican context, the authors
faced two main problems: the first one is connected
with the tremendous lack of data concerning
different health indicators, and the second one
concerns the quality of available information (OMS,
2010). The number of premature deaths (mortality)
is a strong indicator of this situation, as well as the
high levels of suffering (morbidity) and incapacity
(NEPAD, 2008); (Elizabeth et al., 2007).
1.1 Electronic Health Records
Over time, paper-based systems have become
increasingly systematized and gone through several
256
Mupueleque M., Gaspar J., Cruz-Correia R. and Costa-Pereira A..
EVALUATION OF A MATERNAL AND CHILD ELECTRONIC HEALTH RECORD IN A DEVELOPING COUNTRY - Preliminary Results from a Field Pilot.
DOI: 10.5220/0003788902560262
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2012), pages 256-262
ISBN: 978-989-8425-88-1
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

transformations. Paper-based medical records render
the communication between healthcare providers
extremely difficult, especially in developing
countries (Kalogriopoulos et al., 2009); additionally,
some physicians resist new technologies and prefer
the paper-based recording method (Hayrinen et al.,
2008).
Indisputably, individual patient data, collected
and accessed at the point of care, using an Electronic
Health Record (EHR), can assist clinical
management (Gladwin et al., 2002); (Zandieh et al.,
2008). Physicians can easily access previous records
and receive alerts to potential problems, such as drug
interactions (Fraser et al., 2005); (Dumont et al.,
2009); (Slagle, 1999).
Several African countries still face
organizational difficulties such as lack of data
quality; defective data analysis; timely data delivery
problems and data re-use problems by health
professionals. Moreover, the data collection
mechanism in Mozambican National Health Service
healthcare units is based in manual survey forms,
like annual questionnaires (2007; 2005; Allotey and
Reidpath, 2000).
Opinions regarding the security and
confidentiality of medical data differ across
developing countries. In some locations, the uses of
electronic databases are viewed with a good deal of
suspicion (Fraser et al., 2005); (Zandieh et al.,
2008). Patients can face serious risks in their
communities if, for instance, their HIV/AIDS status,
or other sensitive medical information, is uncovered.
These obstacles emanate from a poor medical
culture, where much of the information is rarely
searched for, usually unavailable and frequently
uncollected (Berkowicz et al., 1997).
1.2 Motivation
Approximately 536.000 deaths worldwide relate to
pregnancy and childbirth every year, and 99% of
these deaths take place in developing countries, 86%
of them in Sub-Saharan Africa (NEPAD, 2008;
2005). However, these estimates are collected from
different systems and many of them are unreliable
(Allotey and Reidpath, 2000). In order to enhance
the accuracy of these estimates we need to improve
the collection of data from pregnant women and
health care professionals, using effective and
functional health systems, capable of quickly and
properly answering the health issues of the
population.
1.3 Study Site
The “25 de Setembro” Healthcare Center (HC) is a
public healthcare unit attended by women and men
from the suburban areas of the Nampula Province.
Aside from the maternity and the mother and child
health wards, this HC provides internal and external
general medicine services.
The HC has only one physician, twenty five
nurses, nine midwives, eight healthcare assistants
and has 42 beds.
The maternity ward has 27 female workers.
These workers have very little technical experience,
all of the midwives have a mere elementary level
and only one of them had used a computer in the
past. None of the workers has any knowledge
regarding the use of electronic health record
systems. Despite having an Internet connection, the
signal is erratic and too weak to operate Web-based
electronic record systems.
2 OBJECTIVES
The objective of this work is to develop, implement
and evaluate a Web-based maternal and child
electronic record system in a HC located in the city
center of Nampula, Northern Mozambique, in order
to build a data repository or to improve the method
of collecting, storing, processing, accessing,
communicating and sharing information.
3 MATERIAL AND METHODS
Our approach included the following development
stages: requirements analysis; prototype
implementation; pilot testing and evaluation of the
result.
3.1 Requirements Analysis
The requirements for the prototype were defined
according to the paper-based records analysis, such
as the “antenatal forms” and the “child health card”
used in Mozambique. Accordingly, we can highlight
the following initial requirements:
Allow access from users with low or limited
Internet speeds;
Create forms intended for users with poor
computer skills (avoiding long steps);
Use forms and tables in data visualization;
EVALUATION OF A MATERNAL AND CHILD ELECTRONIC HEALTH RECORD IN A DEVELOPING COUNTRY
- Preliminary Results from a Field Pilot
257

Include in each result interface a set of queries
connected with the data;
Build an access control, with differentiated user
permissions.
During record analysis we discovered that in
Mozambique there is no unique citizen identifier.
For that reason, we had to cross-analyze
information, using 5 fields of personal data. After
the health center record analysis, we defined the
following fields: first name of the patient; last name;
first name of the mother; first name of the father and
neighborhood of residence.
3.2 SISMI Implementation
In the Maternal and Child Health Information
System (SISMI) prototype design we used UML
language to build use case, activity, sequence and
installation diagrams, as well as the conceptual data
model.
We intentionally used Open Source technologies
in both the database and the prototype development.
The primary languages we used were PHP,
JavaScript, HTML, CSS and AJAX; we used the
MySQL database in data management.
3.3 Pilot Testing
Before the actual pilot testing, we arranged a SISMI
6 hour training program with 19 workers from the
obstetric department, in the meetings room.
In order to overcome the inevitable electricity,
Internet and management problems, we used an
offline version installed in a single computer,
equipped with a 2,10 GHZ processor, 4 Gb RAM
and a 500 Gb hard drive, and with an autonomy of 2
hours in case of power failure.
The purpose of this prototype pilot test was to
perform the initial test, to identify necessary
improvements, to adjust the system, to identify
possible problems in the EHR usage and to collect
data.
3.4 SISMI Evaluation
We evaluated the SISMI usability through
interviews and questionnaires, and the authors also
observed. The interviews were carried out in the
antenatal care room with the head of the Maternal
and Child Health program (MCH), in the maternity
ward with the maternity ward responsible and in the
registry with the director of the HC. The general
purpose of these interviews was:
To be acquainted with the services offered and
the structure of the obstetric service in the“25 de
Setembro” HC;
To know the opinion of the midwives, nurses and
physicians, regarding the system;
Understand the HC culture, and socio-economic
and cultural problems.
One other activity involved the analysis of the
medical files, documentation and the observation of
the “25 de Setembro” HC, to:
Verify existent records in antenatal records of
the pregnant woman, childbirth medical records and
existent records in the health card of the child;
Verify the appointments log book of the pregnant
woman;
Consult the books containing the Obstetrics
structure, the nominal list of workers, their roles,
their educational level and their allocation.
We based our questionnaire in the Likert scale, and
the workers specified their level of agreement
towards the SISMI on a 5 point scale, “1 completely
disagree”, “2 disagree”, “3 neither agree neither
disagree” 4 agree” e “5 completely agree”.
4 RESULTS
4.1 SISMI Prototype
The SISMI is a modular system composed by a
registration module, a data query module, a report
module and a statistics module.
The main menu (figure 1) grants access to
personal data of pregnant women, pregnant woman
search, pregnancy details, antenatal appointments,
childbirths, birth and appointments of the child,
displays information regarding routine check-ups of
the child and, finally, the “statistics” option displays
indicators data.
Figure 1: SISMI graphic interface.
HEALTHINF 2012 - International Conference on Health Informatics
258
4.2 Interview Results
The nurses declared that the paper-based record
maintenance in the HC was exceedingly time
consuming.
They also reported that when a pregnant woman
attends a different HC without carrying her antenatal
record, all previous information is lost or neglected
by the new physicians.
Antenatal records, and maternity records in
general, are kept in the log books of the HC, and
some of them reveal a bad conservation state. Many
of the fields of paper-based records are kept empty
or filled with assumptions made by the nurses, since
pregnant women frequently do not know the answer
or cannot remember the details, even for basic
information such as age. In some cases, nurses will
manufacture the information without even asking the
pregnant woman, erroneously assuming that she will
not know the answer. Records are rarely scrutinized
in detail afterwards, contributing to the sense of
irrelevance given to an adequate data collection.
4.3 SISMI Training
The training included a presentation of the system
and a demonstration of use. Subsequently, structured
and semi-structured exercises were performed,
simulating the reception of patients.
The initial reaction of the workers to the system
was quite positive, and they were all willing to
witness its implementation and to learn how to use
the SISMI.
The process of learning how to use the SISMI
was very difficult, and the workers seemed more
comfortable learning from their colleagues.
Although all of the workers did receive training
inside the maternity ward, only three of them were
able to effectively introduce data and use the system.
The main problems we found during training
were the misspellings, the typing speed and the
general speed when using the computer.
4.4 Pilot Testing Results
In the first day the SISMI was used several
necessary improvements were identified in the
interface, in order to enhance and simplify data
entry. The adjustment of the system to the reality of
the HC was immediately carried out by the author.
We observed that the maternity deals with a great
number of pregnant women every day, and the data
entry speed and agility of the worker were not
enough to register all women. Consequently, in
order to solve this issue, we introduced daily visits
to guide its use; additionally, we recommended that
the HC should use the off-peak hours to introduce
records from previous days, that hadn’t been
introduced yet.
It was registered 205 medical files from pregnant
women childbirths, corresponding to the month of
March, 2011. These records were entered in 11 days
of software usage, and after that stage we produced
electronic forms with some maternity indicators.
In any case, the 205 files registered in this period
represent 58% of the total 354 births that took place.
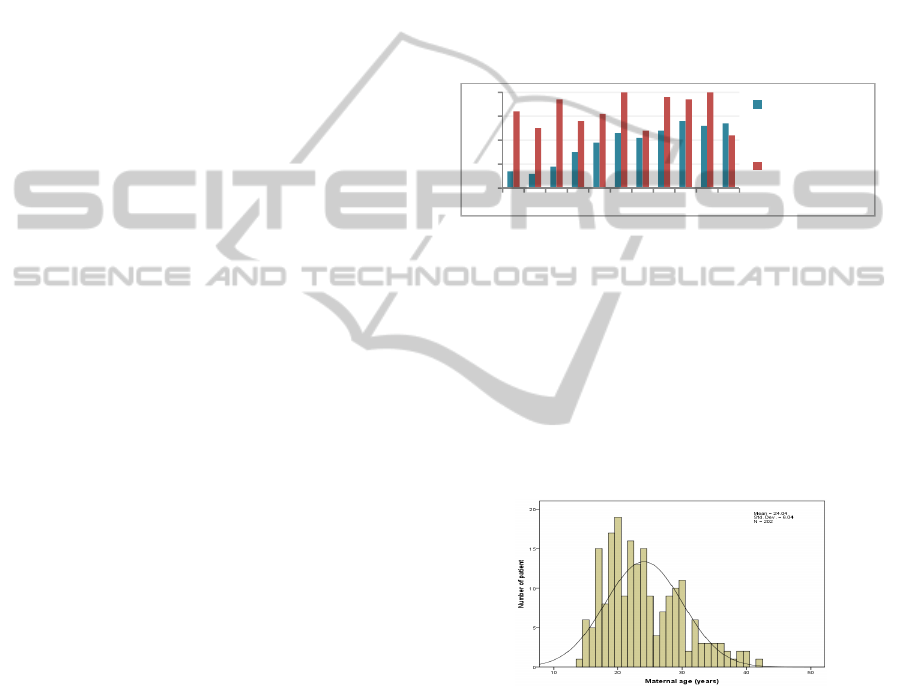
Figure 2 shows the number of appointment files
introduced in the SISMI and births per day.
Figure 2: Number of files introduced per day.
We can clearly observe a gradual increase of the
registered files, illustrating the agility improvement
in the system usage.
4.5 Record Analysis
After a record analysis we identified the introduction
of data inconsistencies in the system, such as: age,
gestational age, weight of the newly-born child, etc.
Figure 3: Age of the women at the time of delivery.
According to the data collected we concluded
that the ages registered for pregnant women ranged
from 14 to 42 years old. However, as we have
already mentioned, the ages were frequently
guessed. The age graphic for pregnant women
(figure 3), shows a small number of registered
patients with 18, 21, 26 and 31 years of age,
suggesting that these were the least ascribed ages.
Therefore, pregnant women with unknown ages
were probably aggregated in the peak categories.
Fetal maturity at the time of birth was another
insufficiently registered or blank field, and in this
0
10
20
30
40
1º 2º 3º 4º 5º 6º 7º 8º 9º 10º 11º
Numberof
birthsregistered
perday
Numberof
birthsperday
EVALUATION OF A MATERNAL AND CHILD ELECTRONIC HEALTH RECORD IN A DEVELOPING COUNTRY
- Preliminary Results from a Field Pilot
259

case only 190 of the 205 files displayed this
information. Table 1 shows a tendency to be born in
the 36
th
week (4% to 12%) and a high tendency to be
born in the 38
th
week (25% to 38%); accordingly,
the likelihood of being born in the 37
th
week could
never be 0%, as indicated. This phenomenon
suggests estimates and guesses from the staff.
Table 1: Expected delivery according to gestational age.
Gestational age (weeks) Births (N=205) [95% CI]
31 0.5% [0;2]
32 0 [0;2]
33 0 [0;2]
34 0.5% [0;2]
35 0 [0;2]
36 7% [4;12]
37 0 [0;2]
38 32% [25;38]
39 58% [51;65]
40 0 [0;2]
41 1% [0;3]
42 1% [0;3]
None of the workers remembered the last time
the scales used in birth weightings were calibrated.
Most of the midwives did not trust the values
obtained with the scales and some of them declared
they were prepared to “guess” the weight of the
infant based on their experience; this is noticeable in
the rounding of all birthweights to the hundreds and
thousands.
Figure 4 shows that more than one quarter of the
newly-born children (28%) were registered as
having exactly 3000 grams (15%) and 2500 grams
(13%); again, this suggests estimates and gross
rounding.
Figure 4: Birthweight distribution.
4.6 Usability Evaluation Results
During observation we concluded that nurses spent
less time (5 minutes) filling paper-based records,
while taking approximately 12 minutes to register
data in the SISMI.
Table 2: Usability evaluation questionnaire and median
classifications (N=9).
Questions concerning usage difficulties
N Mdn
I prefer to work with paper records 5 4
My paper record is more complete
4 2
The paper record is more convenient 4 2
I have trouble using the EHR 4 4
Questions concerning the perceived utility
EHR can be more effective in child care
5 4
EHR can improve my medical practice 8 4
EHR graphics are easy to understand
5 4
EHR is safer than the one in paper-based 5 4
EHR displayed are organized in a clear
manner
6 4
(Mdn: Median of answers)
The questionnaires, containing information
concerning the acceptability and usability of the
system, were handed to 19 workers, as well as a
detailed explanation on how to answer the
questionnaire. Only 9 of them answered the
questionnaire, and out of these only 4 answered all
questions. After the questionnaires were returned we
carried out interviews in order to understand why
some of the questions were left unanswered; several
answers followed these lines: “I was afraid that the
questionnaire would jeopardize my place in the
institution”, “I did not understand how to answer the
questionnaire” and “I did not perceive the utility of
the questionnaire”.
The analysis of the questionnaire and the
interaction with the system proved positive, and this
reveals that the majority of the staff agrees that using
this system can be beneficial to health. However,
considering the low frequency of answers and the
difficulties experienced in their filling, no real
conclusion can be derived from these answers. The
questions we presented proved to be unsuitable
given the educational level of the workers; the
evaluation method was thus inconclusive.
5 DISCUSSION
This system can guarantee the access to the first
maternal and child health indicators based in
pregnant women and serve as an example in
overcoming difficult computer conditions, like the
ones experienced in Nampula, Mozambique.
This system gave way to a simple and effective
method of creating several database query
visualizations while the access to patient data
became quicker once located in a set of database
tables. Unfortunately, the records from the HC of
Nampula are not cross-referenced, and establishing
HEALTHINF 2012 - International Conference on Health Informatics
260

associations between them is practically impossible,
leading to data redundancy and an extremely
difficult data recovery process.
The single tests we ran to check the degree of
correspondence between personal health records and
antenatal care records revealed sufficient
discrepancies to raise validity questions to any
analysis based in these records. This entails serious
implications for maternal and pediatric policy and
planning in this Province.
Despite our method, developed in order to create
a unique identifier, establishing associations across
records is still difficult, and this happens because
many women use different names according to the
purpose of their visit.
The result analysis revealed that the participants
are interested in the implementation of the SISMI.
The interaction with the SISMI proved to be positive
but inconclusive, considering the general lack of
experience with computers.
The workers identified the following benefits
connected with the SISMI and their work in the
health unit: it saves time in the monthly collection of
data; it gives way to a more detailed data analysis; it
ensures an accurate and error-free reporting process,
based in accurate; it stimulates the staff to collect
complete forms.
6 CONCLUSIONS
This system underlines the potential of health
information management in Northern Mozambique,
which can benefit millions of women and children in
the upcoming years by absorbing minimum
resources, saving both time and money.
Furthermore, this system holds unprecedented and
brand new possibilities in the healthcare quality
improvement, especially regarding maternal and
child survival.
However in Mozambique, several socio-
economic and cultural issues need to be answered
before action plans for the implementation of EHR
systems can be enacted, such as: (a) the scarcity of
human resources, both in quantity and quality; (b)
the educational level of the health sector workers,
mostly basic and intermediate; (c) inadequate
facilities; (d) high level of illiteracy; (e) insufficient
communication and transportation networks; (f) lack
of a single patient identifier.
6.1 Future Works
At present, The Nampula Provincial Health
Direction (PHD) is evaluating the proposed SISMI
with the intention of working together with us,
designing and implementing a new test in the “25 de
Setembro” HC or carrying out new pilot tests in
other HC of the Province, in order to develop a
manageable and financially sustainable program. We
also underline the development of additional
functionalities, namely: a partograph, information
regarding the prevention of vertical transmission,
implementing a unique patient identifier technology,
and so forth.
ACKNOWLEDGEMENTS
The authors would like to thank the Nampula PHD,
as well as the entire team of the “25 de Setembro”
HC. So would like to thank to the Department of
Health Information and Decision Sciences (CIDES)
in the Faculty of Medicine, University of Porto,
especially grateful to Professor Cristina Santos.
REFERENCES
(2005). Maternal Mortality in 2005: Estimates developed
by WHO, UNICEF, UNFPA, and The World Bank. In.
(2007). Moçambique - Ministério da Saúde: Relatório
sobre as Boas Práticas do Sistema de Informação em
Saúde de Moçambique. In.
(2008). Sistemas de Informação Sanitária em África:
Recursos, Indicadores, Tratamento de Dados,
Divulgação e uso. In: Conferência Ministerial de
Argel sobre Investigação em Saúde na Região
Africana.
(2009a). Moçambique - Ministério da Saúde, OMS,
UNFPA, UNICEF, USAID: Parceria Nacional para a
Promoção da Saúde Materna, Neonatal e Infantil. In.
(2009b). Moçambique - Ministério da Saúde: Plano
Estratégico do Sistema de Informação para a Saúde
(SIS) - 2009-2014. In, Direcção de Planificação e
Cooperação Maputo - Moçambique.
Allotey, P. A., and Reidpath, D., (2000). Information
quality in a remote rural maternity unit in Ghana. In:
Health Policy Plan 15, 170-176.
Berkowicz, D. A., Chueh, H. C., and Barnett, G. O.,
(1997). Design considerations in migrating an
obstetrics clinical record to the Web. In: Proc AMIA
Annu Fall Symp, 754-758.
Dumont, A., Tourigny, C., and Fournier, P., (2009).
Improving obstetric care in low-resource settings:
implementation of facility-based maternal death
reviews in five pilot hospitals in Senegal. In: Hum
Resour Health 7, 61.
Elizabeth, M., Cristiano, M., Ana M., L., Harriet, B., and
Ezekiel, K., (2007). Mulher, sida e o acesso à saúde na
EVALUATION OF A MATERNAL AND CHILD ELECTRONIC HEALTH RECORD IN A DEVELOPING COUNTRY
- Preliminary Results from a Field Pilot
261

áfrica subsahariana, sob a perspectiva das ciências
sociais. In: vita.
Fraser, H. S., Biondich, P., Moodley, D., Choi, S.,
Mamlin, B. W., and Szolovits, P., (2005).
Implementing electronic medical record systems in
developing countries. In: Inform Prim Care 13, 83-95.
Gladwin, J., Dixon, R. A., and Wilson, T. D., (2002).
Rejection of an innovation: health information
management training materials in east Africa. In:
Health Policy Plan 17, 354-361.
Hayrinen, K., Saranto, K., and Nykanen, P., (2008).
Definition, structure, content, use and impacts of
electronic health records: a review of the research
literature. In: Int J Med Inform 77, 291-304.
Kalogriopoulos, N. A., Baran, J., Nimunkar, A. J., and
Webster, J. G., (2009). Electronic medical record
systems for developing countries: review. In: Conf
Proc IEEE Eng Med Biol Soc 2009, 1730-1733.
NEPAD, (2008). Estratégia para a Saúde. In: A Nova
Parceria para o Desenvolvimento de África.
OMS, (2010). Análise dos Recursos Humanos da Saúde
nos Paises Africanos de Lingua Oficial Portuguesa
[PALOP]. In.
Slagle, T. A., (1999). Perinatal information systems for
quality improvement: visions for today. In: Pediatrics
103, 266-277.
Zandieh, S. O., Yoon-Flannery, K., Kuperman, G.J.,
Langsam, D. J., Hyman, D., and Kaushal, R., (2008).
Challenges to EHR implementation in electronic-
versus paper-based office practices. In: J Gen Intern
Med 23, 755-761.
HEALTHINF 2012 - International Conference on Health Informatics
262
