
Optimizing Electrode Positioning in 3-lead ECG Chest
Devices
Ricardo Simoes
1,2
, Joana Sousa
3
, Cristina Nogueira-Silva
4,5
and Hugo Gamboa
3,6
1
Institute for Polymers & Composites - IPC/I3N, University of Minho
Campus de Azurem, 4800-058 Guimarães, Portugal
2
Polytechnic Institute of Cávado and Ave, Campus do IPCA, 4750-810 Barcelos, Portugal
3
PLUX - Wireless Biosignals, S.A., Av. 5 de Outubro, n. 70 – 6, 1050-059 Lisbon, Portugal
4
Life and Health Sciences Research Institute (ICVS), University of Minho, 4710-057 Braga;
ICVS/3B’s - PT Government Associate Laboratory, Braga/Guimarães, Portugal
5
Department of Obstetrics and Gynecology, Hospital de Braga, 4710-243 Braga, Portugal
6
CEFITEC - Faculdade de Ciências e Tecnologia, Universidade Nova de Lisboa
2829-516 Caparica, Portugal
Abstract. Although the 12-lead electrocardiogram has become an essential
medical and research tool, many current and envisaged applications would ben-
efit from simpler devices, using 3-lead ECG configuration. This is particularly
true for Ambient Assisted Living (in a broad perspective). However, the chest
anatomy of female patients, namely during pregnancy, can hamper the adequate
placement of a 3-lead ECG device and, very often, electrodes are placed below
the chest rather than at the precise thoracic landmarks. Thus, the aim of this
study was to compare the effect of electrode positioning on the ECG signal of
pregnant women and provide guidelines for device development. The effect of
breast tissue on the ECG signal was investigated by relating breast size with the
signal-to-noise ratio, root mean square and R-wave amplitude. Results show
that the 3-lead ECG should be placed on the breast rather than under the breast
and indicate positive correlation between breast size and signal-to-noise ratio.
1 Introduction
The electrocardiogram (ECG) was introduced in clinical practice in 1942 and nowa-
days is one of the most used non-invasive techniques in medicine. For extracting the
ECG signal, the placement of multiple electrodes in specific anatomic regions is typi-
cally required. The patient is traditionally connected to the ECG monitoring system
using 10 wires, which allow a 12-lead ECG reading; with this configuration, the de-
polarization and re-polarization of the heart are recorded as five typical waves (P, Q,
R, S and T) [1]. The most analyzed feature of the ECG trace is the QRS complex,
which reflects the ventricles’ depolarization. The R-wave is the most widely used for
extracting important cardiac parameters, such as the Heart Rate (HR = 1/(R
i+1
-R
i
))
and the Heart Rate Variability (HRV = R
i+1
-R
i
). With those parameters, the physician
can identify and possibly predict several cardiac pathologies [2].
However, the quality of the signal depends strongly on the electrode placement
Simoes R., Sousa J., Nogueira-Silva C. and Gamboa H..
Optimizing Electrode Positioning in 3-lead ECG Chest Devices.
DOI: 10.5220/0003885800810088
In Proceedings of the 2nd International Living Usability Lab Workshop on AAL Latest Solutions, Trends and Applications (AAL-2012), pages 81-88
ISBN: 978-989-8425-93-5
Copyright
c
2012 SCITEPRESS (Science and Technology Publications, Lda.)

since noise or presence of artifacts on the ECG can induce important diagnosis errors
[3]. Therefore, a strong knowledge of the correct ECG acquisition procedures is re-
quired to conduct a proper diagnosis. It is usually assumed that a major variation on
ECG signals results from chest lead misplacement, which can cause attenuation of
ECG amplitudes due to abundant breast tissue [4, 5]. This is a problem, namely in
women and obese patients, and has given rise to many studies because there is an
uncertainty about the standardized procedures for the placement of ECG chest elec-
trodes in these patients. In 1998, Pentti [6] studied the effect of breast tissue protuber-
ance on ECG signals using a 12-lead ECG and concluded that the volume of breast
tissue had no effects on ECG amplitudes. In this paper, they also recommended the
placement of the chest electrodes on the breast in detriment of placing them under the
breast. Five years later, Marcfarlane [3] studied the precordial electrode placement in
women, using 12-lead ECG. As well as Penti et al., the authors of this study have not
found variability in the ECG signal related to the anatomical positioning of the elec-
trodes namely on lead V3 and V4.
In recent years, we have witnessed a clear tendency for miniaturization of medical
devices, either for remote monitoring purposes or for ambulatory usage. With the
ECG being an important signal to be monitored and taking into account the needs of
the new medical and social areas such as Ambient Assisted Living (AAL), the 12-
lead configuration has a tendency to be abandoned and replaced by 3-lead solutions at
breast level. In particular, considering the most recent developments in AAL devices,
the 3-lead ECG is clearly a major current application and many such devices are ex-
pected to enter the market in the upcoming years [7]. Therefore the knowledge of the
correct ECG–electrode placement is extremely important in the particular case of 3-
lead configuration devices. The 3-lead ECG is more prone to the effects of misplace-
ment than the 12-lead ECG due to the reduced number of electrodes, which increase
the probability of getting a noisy signal in one of them. It is very important to obtain
clean ECG signals from all ECG-electrodes. On the other hand, the generalization of
these devices makes them prone to be used in a variety of different scenarios and by a
higher number of professionals than the traditional ECG. These small and, currently,
wireless devices can be employed in disaster scenarios, transit of patients, home-care
environments and many other situations. As the general purpose 3-lead sensor must
be placed on the left side of the chest, an improved understanding of the effect of the
breast shape and volume on the ECG signal is vital.
1.1 Motivation and Goals
The main goal of this study was to verify if (and how) breast size affects the ECG
signal and which is the best electrode placement using a 3-lead sensor in order to
acquire a signal with high quality and without compromising the medical diagnostic.
The effects of ECG-electrode placement and breast size on the acquired signal
were investigated by analyzing the differences in signal-to-noise (SNR), root mean
square (RMS) and R-wave amplitude that resulted from positioning the sensor on the
breast and under the breast. The correlation between breast size and SNR, RMS and
R-wave amplitude were also ascertained.
82

2 Methods
2.1 ECG Signal Processing
From the collected ECG signals, the signal-to-noise ratio (SNR), root mean square
(RMS), R-wave amplitude and Heart Rate (HR) were extracted.
To obtain the SNR, some steps were followed:
1) A low-pass filter, with 50 Hz cut-off frequency, was applied to the raw ECG.
The ECG spectrum contains frequencies in the range from 0.05 Hz up to 40 Hz [8].
Frequencies higher than 50 Hz are considered as noise. Thus, a Butterworth digital
filter, with cut-off frequency of 50 Hz, order 2 and sampling frequency of 1000 Hz,
was applied to the ECG raw signals. No band pass filter was used, since frequencies
lower than 0.05 Hz have negligible impact on the signal.
2) Noise was calculated as the difference between raw and filtered signal (eq. 1).
Noise = ECG
raw_signal
- ECG
filtered_signal
(1)
3) Both for raw signal and noise, the energy index (EI) was calculated (eq. 2).
(
)
=
1
()
2
=0
(2)
4) Using EI, the RMS both for raw signal and noise was calculated (eq. 3).
=
√
(3)
5) Finally, with the RMS values, the SNR was calculated (eq. 4).
=20×
(
_
)
(
)
(4)
The R-wave amplitude and HR were obtained through an ECG algorithm that uses an
exponential order to seek the R-peaks. The implemented algorithm was based on Pan
& Tomkins [15] to assure that the R-peaks are correctly extracted.
2.2 Breast Size Estimation
The breast size (Bs) was estimated based on the transversal area of the entire breast,
measured for each subject from a lateral digital image collected at the time of the
ECG data acquisition, as schematically represented in Figure 1 (left). Image
processing software was employed to manually draw a spline over the previously
captured digital image, creating a closed region that encloses the entire breast. The
software measures the area of that region automatically.
83
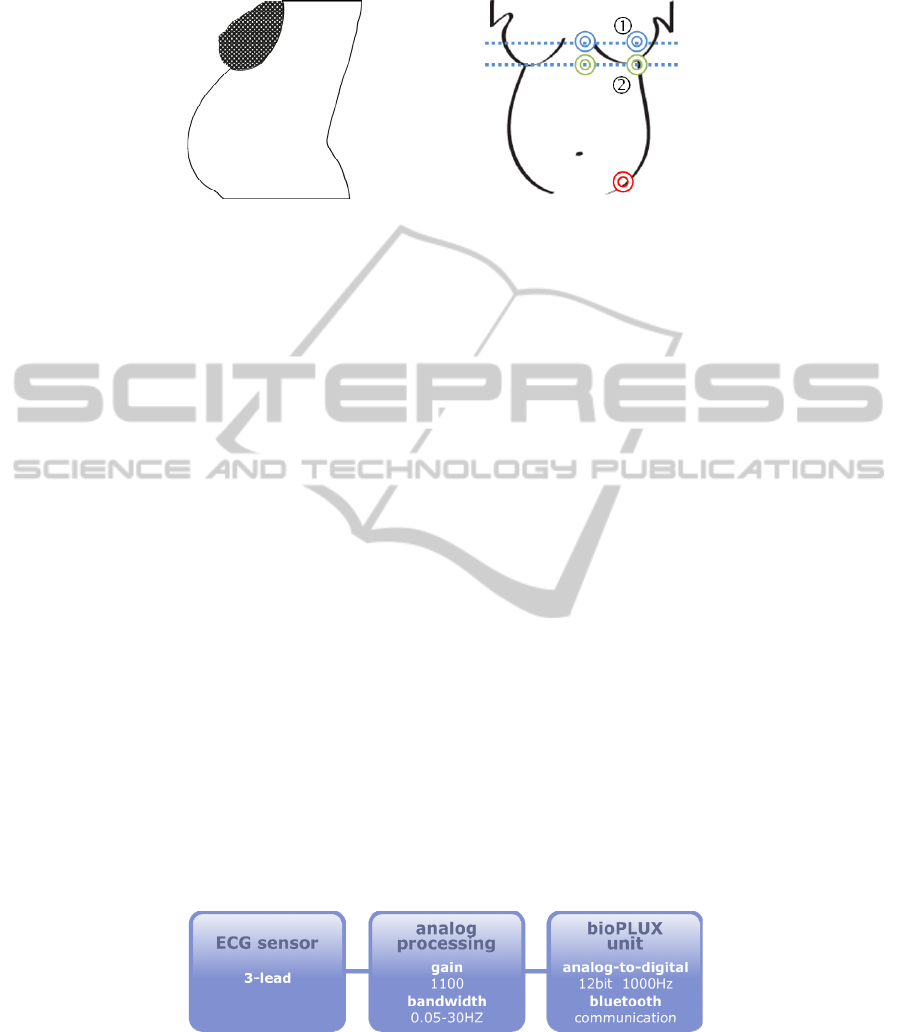
Fig. 1. Estimation of breast size (left), and precordial electrode location for the ECG measure-
ments; the two channels are indicated by double concentric circles, in blue and green, and the
ground is shown at the iliac crest, in red. (right).
2.3 ECG Features Analysis
The extracted parameters (described in Sections 2.1 and 2.2) were statistically ana-
lyzed. In the present work, a t-test was used and all results with p-value less than 0.05
were considered as statistically significant and with R-value larger than 0.5 linearly
related. The statistical study was divided in two analyses:
1) Comparison between ECG-electrode placement and signal parameters.
SNR, RMS and R-wave amplitude were compared concerning the ECG-electrode
placement in two different anatomic regions: on the breast (Figure 1-right, placement
1) and under the breast (Figure 1-right, placement 2), which correspond to the V2 and
V4 standard positions. The mean and standard deviation were calculated for each
signal parameter and then compared regarding the referred anatomic regions.
2) Effect of Breast size on ECG signal
A regression equation and the correlation coefficient were calculated in order to in-
vestigate if the breast size affects the ECG signal.
3 Experimental Setup
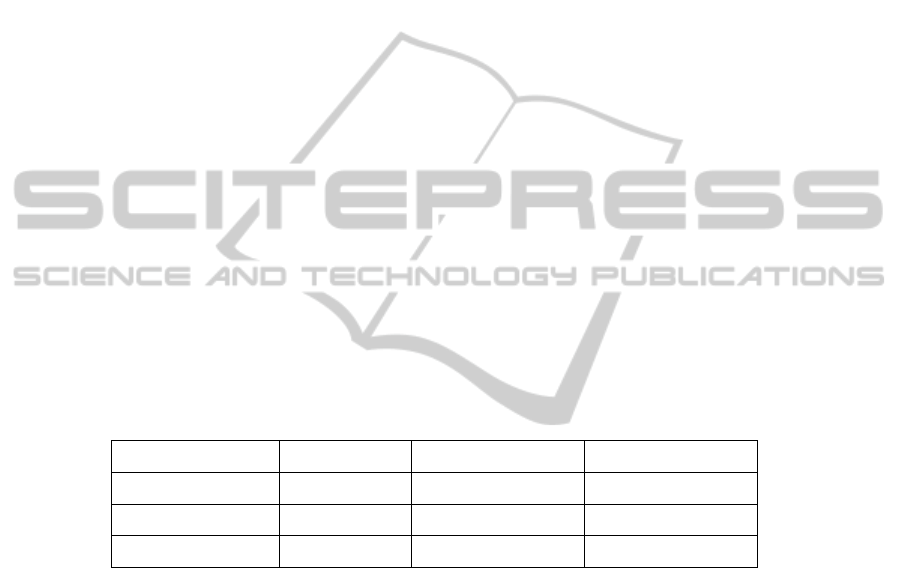
To acquire biosignals in this study, electrocardiography sensors [9] and Kendall/Tyco
ARBO disposable surface electrodes (48x34mm) were used. For the signal’s analog
to digital conversion and Bluetooth transmission to the computer a wireless signal
acquisition system, certified for clinical ECG usage, was used (bioPLUX research)
which has 12 bit ADC and a sampling frequency of 1000 Hz [10]; see Figure 2.
Fig. 2. System architecture.
84
The ECG trace has been collected for each patient in 2 different chest locations. In
order to enable comparison between the two ECG traces, they were recorded simulta-
neously in two different channels of the signal acquisition system. A pair of elec-
trodes (ECG channel 1) was placed at the nipple level and another (ECG channel 2) at
the infra-mammary level. The ground electrode was placed at the left iliac crest. The
setup is shown in Figure 1-right.
The study was conducted in a clinical setting, in a temperature-controlled room.
Measurements were conducted with subjects resting in a sitting position, which was
considered the most representative of continuous (and remote) monitoring scenarios.
In each measurement, the ECG signal was recorded for 2 minutes to enable
processing and analysis. The study subjects were pregnant patients of the Hospital of
Braga (Braga, Portugal), with 30 to 39 weeks of gestation, and who volunteered to
participate in the study and have their vital signals monitored and registered. In-
formed consent forms have been collected from all subjects. The study was approved
by the Hospital ethics committee. The test group included 17 subjects. No subject was
known to have cardiac problems that should be taken into consideration in the study.
4 Results and Discussion
4.1 Effect of Electrode Placement
Table 1 lists the statistical results (t-test) obtained for SNR, RMS and R-wave ampli-
tude with respect to the two anatomic ECG electrode placements.
Table 1. Statistical values for SNR, RMS and R-wave, for the two ECG-electrode placements.
Anatomic Regions SNR (dB± SD) RMS (mV± SD) R-wave (mV± SD)
On the Breast (Wn) 21.2 ± 1.8 0.29 ± 0.1 1.6 ± 0.5
Under the Breast (Wt) 19.9 ± 2.9 0.17 ± 0.1 1.0 ± 0.3
p-value 0.1 < 0.001 < 0.001
From the results of Table 1, it can be observed that RMS and R-wave values de-
crease when comparing the electrode placement on (Wn) with under (Wt) breast. The
same trend is observed for SNR outcomes; however this decrease is not statistically
significant (p-value >.05), demonstrating that it is indifferent to place the ECG-
electrode on or under breast concerning the level of noise. Despite this decrease not
being significant, the ECG-electrode placement does influence the signal, since there
is a statistically significant decrease in RMS and R-wave values under the breast (p-
value < .05). Thus, the results show that the decrease of signal amplitude is not due to
the decrease of the SNR value, but due to the distance between electrode and heart,
which is lower when the electrode is placed on the heart than when it is placed under
the heart In fact, about two-thirds of the heart volume are at the left of the mid-sternal
line, in the direction of the left breast [1]. As a consequence, by placing the ECG-
electrode on the breast the amplitude of ECG signal is higher than under breast be-
85

cause this last placement is more distant from the heart, leading to a decrease of the
ECG RMS value and R-wave amplitude.
These results are not in accordance with the traditional concept. It is believed that
adipose tissue, due to its biologic features, attenuates the ECG amplitudes and de-
creases the SNR value. The obtained results show the opposite behavior, i.e., on the
breast, where the adipose tissue is abundant, the SNR is higher than under the breast.
The same is verified for the RMS value and the R-wave amplitude. Thus, the con-
ducted study does not support the traditional concept, and for a 3-lead ECG configu-
ration, it is recommended to place the ECG-electrode on the breast rather than under.
4.2 Effect of Breast Size
Table 2 lists the regression results for SNR, RMS and R-wave with Breast Size. Re-
sults reveal poor correlation of RMS and R-wave with Breast Size since the correla-
tion's coefficient (R
2
) is less than 0.5 for both parameters.
Furthermore, it can be also verified that despite the R
2
for SNR being less than
0.5, it seems to have a positive linear correlation trending between SNR values and
Breast Size (R>0.5). This can mean that these two variables are somehow correlated,
and SNR can improve with the increase of breast size. However, when these two
variables are categorized, it can be ascertained that there is an increase of the SNR
value with the rise of the Breast Size but only up to a certain breast size value. From
that threshold on, a stabilization of SNR values is observed, i.e., the SNR maintains
its value (≈23dB) with further increase of breast size.
The obtained results reinforce that the SNR is positively influenced by adipose
tissue, with the RMS and R-wave of ECG signal being unchanged with the breast
size. Once more, the results are not supporting the traditional idea that adipose tissue
influences negatively the ECG signal. Other authors have also found this trend, when
they were studying the relationship between breast protuberance and placement of
electrodes on breast. In face of this situation, some authors [11] have suggested that,
physiologically, an increase of chest size is associated with an increase of left ventri-
cular mass (LVM), which is related to the body weight, an important factor on LVM.
Following this line of thought, other studies related to chest size, body weight and
LVM have been published in order to find out a consolidated relationship between
chest size/body weight and LVM. For example, in 1977, Horton [12] studied the
distance for precordial ECG measurement estimating LVM using an echocardiogram.
In this study, the researchers observed a positive relationship between precordial
voltage and echo LVM, concluding also that ECG amplitudes could be strongly influ-
enced by the thoracic size. Also, in 2001, Mahommad [13] tried to determine the
LVM from echocardiogram, and he has verified a positive linear correlation between
LVM and body weight both for males and females. Similar results were obtained by
Jose Peralta-Huerstas in 2008 [14], when investigating LVM differences between
overweight and normal-weight pre-adolescents.
Despite the fact that, in this work, an echocardiogram was not used, the outcomes
suggest that, in fact, the increase of chest size, and breast as well, can positively in-
fluence the ECG signal. However, it is necessary to significantly increase the study
population to establish better statistical significance and obtain more accurate results.
86

Table 2. Linear Regression coefficients relating the parameters SNR, RMS and R-wave with
Breast size (x) (Parameters = a*x +b).
Parameters a b R
2
SNR 0.0056 19.20 0.3
RMS 0.0001 0.24 0.1
R-wave 0.0007 1.38 0.1
5 Concluding Remarks
Over the years, electrode placement has been studied to determine if chest size has an
effect on the ECG signal. This is a critical point in standard ECG procedures, particu-
larly in women or obese patients. In women, the conventional procedure is to place
the ECG-electrode under rather than on the breast, since it is believed that adipose
tissue attenuates the signal and introduces noise. In this work, the ECG signals ac-
quired with a 3-lead ECG sensor positioned on and under the breast were compared,
and the effect of breast size on the signal was determined.
Results indicate that the ECG-electrodes should be placed on the breast rather
than under the breast because there is a statistically significant difference in the RMS
value and R-wave between the signals acquired at these two anatomic regions. These
parameters were found to be higher on the breast than under the breast. In terms of
SNR, no statically significant differences were found. Concerning the effect of breast
size on the ECG signal, there seems to be a positive correlation between SNR and
breast size; however, no relationship was found between ECG amplitudes and breast
size. The intensification of SNR with the increase of breast volume can be explained
by the relationship between LVM and chest size (LVM increases with chest size).
In the future, work will focus on confirming the results and extend the number of
subjects to increase statistical significance. Also, new form factors for 3-lead ECG
devices will be pursued in the context of AAL. An improved understanding the para-
meters under study in this paper will provide valuable information for the future de-
velopment of wearable sensor devices.
Acknowledgements
National Strategic Reference Framework (NSRF-QREN) program, for enabling the
study. Braga Hospital (Portugal) for approving the study and providing facilities for
data collection. We also thank the collaboration from the staff in the Department of
Obstetrics and Gynecology. Partial financial support provided by the Foundation for
Science and Technology, Lisbon, through 3° Quadro Comunitário de Apoio, and
project “Do-IT”, co-financed by the European Community Fund FEDER through
COMPETE – Programa Operacional Factores de Competitividade (POFC).
87

References
1. Tortora, G. J, Grabowski, S. R., (2001). Introduction of Human Body – The essentials of
anatomy and Physiology. John Wiley & Sons, INC, 5th Edition.
2. Paoletti, M., Marchesi, C., (2006). Discovering dangerous patterns in long-term ambulatory
ECG recordings using a fast QRS detection algorithm and explorative data analysis. Com-
puter Methods and Programs in Biomedicine, 82:20-30.
3. Macfarlane, P., Colaco, R., Stevens, K., Reay, P., Beckett, C., and Aitchison, T., (2003).
Precordial electrode placement in women. Netherlands Heart Journal, 11(3):118.
4. Soliman, E. Z., (2008). A simple measure to control for variations in chest electrodes
placement in serial electrocardiogram recording. Journal of Electrocardiology, 41:378-379.
5. García-Niebla, J., Llontop-García, P., Valle-Racero, J. I., Serra-Autonell, G., Batchvarov,
V. N., (2009). Technical mistakes during the acquisition of the Electrocardiogram. Journal
compilation, Willey Periodicals, Inc, 14(4).
7. Muhlsteff, J., Such, O., Schmidt, R., Reiter, H., Lauter, J., Thijs, J., Musch, G., Harris, M.,
(2004). Wearable approach for continuous ECG – and Activity Patient-Monitoring. Pro-
ceedings of the 26th Annual Internat.Conf. of IEEE EMBS, San Francisco, CA, USA:1-5.
8. Mahmoud, S. S., Fang, Q., Davidovic, D. M., Cosic, I., (2006). A Time-Frequency ap-
proach for the analysis of Normal and Arrythmia Cardiac Signals. Proceeding of the 26th
IEEE EMBS Annual International Conference, New Work City, USA.
9. PLUX, ecgPLUX, PLUX Wireless Biosignals. Available from: www.plux.info [Accessed
August 8, 2011].
10. PLUX, bioPLUX Research, PLUX Wireless Biosignals. Available from: www.plux.info
[Accessed Aug 8, 2011].
11. Rautaharju, P., Park, L., Rautaharju, F., and Crow, R., (1998). A standardized procedure
for locating and documenting ecg chest electrode positions: consideration of the effect of
breast tissue on ecg amplitudes in women. Journal of electrocardiology, 31(1):17–29.
12. Horton, J., Sherber, H., and Lakatta, E., (1977). Distance correction for precordial electro-
cardiographic voltage in estimating left ventricular mass. Circulation, 55(3):509.
13. Mohammed, M. (2001). Determination of left ventricular mass by echocardiography in
normal Arab people. morbidity and mortality, 4:6.
14. Peralta-Huertas, J., Livingstone, K., Banach, A., Klentrou, P., and O’Leary, D., (2008).
Differences in left ventricular mass between overweight and normal-weight preadolescent
children. Applied Physiology, Nutrition, and Metabolism, 55.
15. Pan, J, Tompkins, W. J., (1985). A real-time QRS detection algorithm. IEEE Transactions
on Biomedical Engineering, 3:230-236.
88
