
Development and Evaluation of a Sensor-based System for Remote
Monitoring and Treatment of Chronic Diseases
The Continuous Care & Coaching Platform
Harm op den Akker
1,2
, Monique Tabak
1,2
, Mihai Marin-Perianu
3
, Rianne Huis in’t Veld
2
,
Valerie M. Jones
2
, Dennis Hofs
1
, Thijs M. T
¨
onis
1,2
, Boris W. van Schooten
1
,
Miriam M. R. Vollenbroek-Hutten
1,2
and Hermie J. Hermens
1,2
1
Roessingh Research and Development, Cluster Telemedicine, Enschede, The Netherlands
2
University of Twente, Telemedicine Group, Enschede, The Netherlands
3
Inertia Technology, Enschede, The Netherlands
Keywords:
Telemedicine, User-centred Design, Physical Activity, Lifestyle Monitoring.
Abstract:
The steep increase in the number of people with chronic diseases in the Western world is a long recognised
problem which forces us to look for less labour intensive and more cost effective methods to deliver health-
care. Wider use of telemedicine services seems to be a solution that can contribute substantially to reduction
of costs and maintenance of health service quality at a high level, but its implementation in regular healthcare
practice often fails. This is no surprise since designing, building and implementing a successful telemedicine
application is no trivial task. The reasons for failure are many, and include technical problems and low us-
ability, however there are also organisational factors such as the often disruptive effect the introduction of new
technologies can have on existing healthcare processes. This paper presents the experience gathered when
building our system: the Continuous Care & Coaching Platform (C3PO). This platform was designed to mon-
itor patients with chronic diseases during daily life and provide them with the support they need to develop
and maintain an active lifestyle in order to improve quality of life and offset deterioration of health condition.
In this paper we share the lessons learned and present results of evaluation studies using earlier versions of the
platform. Innovations in the field of wireless sensor technology as well as changing demands from the users
led us to redesign and develop a new version of the platform. This process is described, starting with the gath-
ering of requirements using a user-centred design approach and derivation of specifications. The components
of the platform are described as well as results of recent evaluation studies. Our evaluations and experience
with working with patients and healthcare professionals indicate that there is currently a great need to add in-
telligence to the platform. The augmentation of the platform with of a smart autonomous health- and lifestyle
coach is the current focus of our research which, we believe, will be a crucial next step towards the future of
intelligent telemedicine applications.
1 INTRODUCTION
The world’s population is rapidly ageing, as a result
of both longer life expectancy and declining fertil-
ity rates. Worldwide, the proportion of people aged
over 60 is growing faster than any other age group,
and by 2050 there will be some 2 billion elderly per-
sons. A person’s health typically deteriorates with
increasing age and chronic diseases emerge, induc-
ing greater demand for long-term care. According
to the United Nations report “World Population Age-
ing 150-2050” (United Nations, Department of Eco-
nomic and Social Affairs, Population Division, 2002),
the mortality, morbidity and disability attributed to
the major chronic diseases — heart disease, stroke,
cancer, chronic respiratory diseases and diabetes —
is expected to rise to 73% of all deaths and 60% of
the global burden of disease by 2020 . Finding in-
novative approaches to making our healthcare system
affordable and sustainable is needed.
Regular physical activity is beneficial for healthy
aging as it substantially delays the deterioration of
health status and helps prevent the development of
secondary chronic diseases. A focus on (self-) man-
19
Tabak M., Tönis T., van Schooten B., Marin-Perianu M., Jones V., Huis in ’t Veld R., Vollenbroek M., Hofs D., den Akker H. and Hermens H. (2012).
Development and Evaluation of a Sensor-based System for Remote Monitoring and Treatment of Chronic DiseasesThe Continuous Care & Coaching
Platform.
In Proceedings of the Sixth International Symposium on e-Health Services and Technologies and the Third International Conference on Green IT
Solutions, pages 19-27
DOI: 10.5220/0004474700190027
Copyright
c
SciTePress

agement of physical condition will become increas-
ingly important in future chronic care and in the
support of the healthy elderly population. Informa-
tion and Communication Technologies play a cru-
cial role in supporting greater independence and self-
management of lifestyle and disorders. We need to
identify patient management approaches that will en-
sure appropriate monitoring and treatment remotely.
To deal with this problem, Hermens and Vollenbroek-
Hutten (Hermens and Vollenbroek-Hutten, 2008) pro-
pose to develop remote monitoring and treatment sys-
tems. These should integrate ambulant sensing to
measure relevant bio signals and context information
with secure data handling and appropriate clinical de-
cision support functionality to assist in both technical
and clinical decision making. In addition, the sys-
tem should also provide feedback to both patients and
care providers. In other words, such systems should
provide continuous monitoring of health status, with
the promise of coaching, or continuous motivational
aid aimed at achieving behavioural change, whenever
required, and efficient and effective individually tai-
lored treatment anywhere anytime.
These systems do promise to make healthcare
more quantitative, more efficient and effective and
less costly, which is desirable for patients, healthcare
professionals and health insurance companies alike.
Although the number of available systems is rapidly
increasing, still around 75% of the telemedicine ini-
tiatives fail during the operational phase after a pilot
(Berg, 1999) and, despite numerous trials, very few
are transferred successfully into routine health care.
Inadequate technical performance as well as low us-
ability of these systems is considered to be among the
major barriers for successful implementation (Broens
et al., 2007).
Our aim was to develop a remote monitoring
and treatment platform for elderly and patients with
chronic disorders, to support them in developing
and maintaining an active lifestyle and improving
their physical condition, either independently or su-
pervised remotely by their healthcare professionals.
The platform, focussed on continuous monitoring and
feedback to the users is called the Continuous Care &
Coaching Platform or C3PO. In this paper, we de-
scribe the development of the platform and its com-
ponents: sensors, Smartphone, server and web por-
tal. Section 2 starts with a short overview of the cur-
rent state of the art of telemedicine platforms and re-
search. We then describe the process of our user-
centred design approach, starting with the lessons
learned from previously developed remote monitor-
ing systems, the development of functional and tech-
nical requirements, the platform design, and system’s
evaluation. Finally, we discuss the ongoing work in
improving the platform and discuss the future of re-
mote monitoring and treatment systems.
2 BACKGROUND
The field of telemedicine research is large, and rapidly
expanding. A systematic review of reviews by Eke-
land et al. (Ekeland et al., 2010) found 1593 reviews
of telemedicine systems published since 1998. Hav-
ing included 80 reviews in their analysis, the authors
found only 21 reviews that concluded telemedicine
to be effective, and 18 that concluded that evidence
is “promising but incomplete”. Similar results can
be found when looking into telemedicine applications
targeting physical activity interventions (an important
focus of C3PO). A systematic review by LaPlante
and Peng (Laplante and Peng, 2011) analyzed 31 e-
Health intervention publications targetting physical
activity between 2006 and 2010. Four of the 7 stud-
ies that used pure control groups showed support for
e-Health, while the others showed no significant dif-
ferences. The authors conclude that although it is dif-
ficult to argue for the benefits of e-Health compared to
classic interventions, none of the evaluated platforms
fared worse than its control setting. Thus it seems that
more research in the area of telemedicine, as well as
more standardized and thorough evaluations of its ef-
fects are necessary. This conclusion is also found in
a review conducted by Polisena et al. who studied
home telehealth systems for Chronic Obstructive Pul-
monary Disease (COPD), one of the important target
groups for the platform. The authors reviewed 9 stud-
ies, and concluded that although emergency depart-
ment visits and hospitalization rated declined, other
outcome parameters varied between studies (Polisena
et al., 2010).
Telemedicine platforms come in many shapes and
forms, some focussing more on vital sign monitoring
for e.g. elderly (Czabke et al., 2011) or cardiac pa-
tients (Kumar et al., 2008; Jones et al., 2009); oth-
ers focus more on the human-computer interaction
through television (Burkow et al., 2008), smartphones
(op den Akker et al., 2010; Wieringa et al., 2011;
St
˚
ahl et al., 2008; Chen et al., 2009), web-based com-
munities (Lewis et al., 2008) or web portals (Her-
mens and Vollenbroek-Hutten, 2008). A full review
of all the related aspects of telemedicine platforms
would be out of the scope of this paper. It is how-
ever important to recognize their complexity in both
technical and societal sense, and we strongly believe
that careful attention to all aspects, as well as broad
user involvement throughout all the stages of devel-
EHST/ICGREEN 2012
20

opment can contribute to the potential success of any
telemedicine application.
3 FIRST LESSONS LEARNED
In 2006, development started on an ambulant activity
monitoring system. In this first version of the plat-
form, a 3D motion sensor (XSens MT9) was used to-
gether with a data logger. The sensor contained three
separate uni-axial piezoelectric accelerometers with a
range of 2g, and was connected over a wire to the
data logger. Both devices were worn on a belt on the
waist. In one of our first studies on daily physical
activity, we used the MT9 to measure the activity lev-
els of chronic low back pain (CLBP) patients in their
everyday lives and compared the results of the ex-
perimental group with those of healthy controls (Van
Weering et al., 2009). Participants wore the devices
for 7 consecutive days from 7:00 am until midnight
for a maximum of 17 hours per day. After the mea-
surement week, the memory card from the data log-
ger was read out and the data was analyzed. These
first studies gave us valuable insights in the activity
patterns of CLBP patients, showing for example their
tendency to be much more active in the mornings and
much less active in the evenings compared to healthy
controls. But it had an obvious disadvantage in terms
of its size and was not comfortable to wear for long
periods of time. Therefore, we started the develop-
ment of a new version in 2008.
The second itertation of the platform consisted of
a wireless 3D accelerometer (XSens MTx-w) and an
HTC Smartphone. The sensor connects wirelessly via
Bluetooth to the Smartphone, which can be worn on a
belt clip or in a pocket. The use of a wireless connec-
tion between the sensor and the Smartphone meant
the system was easier to operate and more flexible
in terms of its placement on the patient’s waist. The
use of a Smartphone also provided us with the op-
tion of designing real-time feedback on the stream-
ing input data and consequently allowed us to de-
sign fully ambulatory interventions. The Smartphone
could be used to show the patient a real-time graph
of his daily activity compared to reference values and
based on this provide timely feedback messages de-
signed to encourage the patient to change his phys-
ical activity behaviour. The platform was used in
a number of studies for monitoring everyday activ-
ity patterns in patients with different conditions in-
cluding chronic low back pain, chronic fatigue syn-
drome (CFS) and chronic obstructive pulmonary dis-
ease (COPD); it was also trialled on cancer survivors
and obese subjects. In each of these groups, the pa-
tient’s physical activity plays a role in the progres-
sion of his condition and general quality of life. In
COPD, for example, patients are symptomatic even
when performing normal daily life activities. This
causes the patient to avoid activity, leading to a de-
crease in physical fitness which causes a rise in the
incidence of COPD exacerbations. In this case, im-
proving the physical activity behaviour can offset this
downward spiral that is so commonly seen in COPD.
The Smartphone application also prompts patients to
answer questions presented at fixed time intervals dur-
ing the day on self-perceived activity performance, to
rate their level of pain (in case of CLBP), dyspnoea
(in case of COPD), fatigue (in case of CFS, COPD)
or to provide information on food intake (in case of
obesity) by means of visual analogue scales (VAS).
The feedback intervention studies showed that use of
the system for a period of several weeks resulted in
decreased symptoms and increased activity levels.
Although the second version of the platform was
an obvious improvement in terms of usability and
flexibility, new issues emerged during the use of this
system in the various studies. The wireless Bluetooth
connection between the sensor and Smartphone was a
drain on the batteries of both devices. For the Smart-
phone we had to use extended battery packs, making
the devices more bulky than they needed to be, and for
the sensor, the drain on the batteries meant the device
would often run out of power after 12 hours of opera-
tion. Another issue was data loss. Because the sensor
sends out its raw sampled values continuously, each
time the Bluetooth connection is dropped, data is lost.
These limitations as well as further advancements in
the field of wireless sensor technology and mobile de-
vices led to a further cycle of design and development
and a new version of the platform, described in the
next section of this article.
4 REQUIREMENTS AND DESIGN
In the following two sections we will explain the
process of requirements elicitation for the new plat-
form, called the Continuous Care & Coaching Plat-
form (C3PO) as well as the design of each of its indi-
vidual components.
4.1 Requirements
Early versions of the platform were mainly designed
for research purposes, but the experimental studies in-
dicated that the system had potential utility as a be-
havioral intervention tool. However, it also became
clear that the system needed to be redesigned to bet-
Development and Evaluation of a Sensor-based System for Remote Monitoring and Treatment of Chronic Diseases - The
Continuous Care & Coaching Platform
21
ter meet the user’s needs in terms of being more user
friendly and being able to be integrated into the daily
work practices of the health care professionals. The
early involvement of patients and professionals in the
requirements analysis and the design process is cru-
cial for this. Therefore, for developing the require-
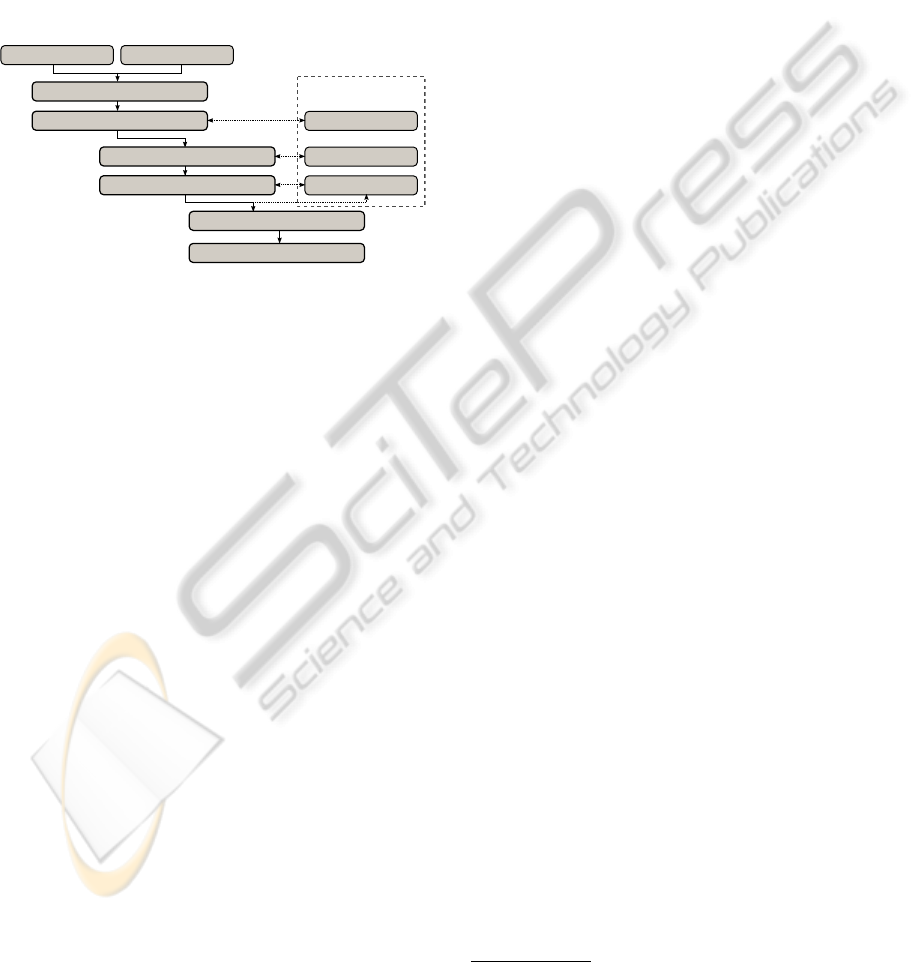
ments of C3PO, we chose to apply an iterative, user-
centred design approach, as shown in Figure 1. In this
approach the designers take the users as the starting
point for design and involve them in the evaluation of
design choices.
User knowledge
State of the art
Scenario refinement (FICS)
Scenario (PACT)
Functional requirements
Technical specifications
System design
Platform implementation
Conceptual
Functional
Technical
Evaluation
Figure 1: General iterative design process of the platform.
Exactly how to usefully involve users in the de-
velopment process is far from obvious because of
the knowledge gap between the users and developers
and their differences in language use which seriously
complicates effective communication (Huis in’t Veld
et al., 2010). Scenarios are considered an effective
technique to bridge these gaps (Carroll, 2000). A sce-
nario is a detailed storyline that describes the users
daily activity in the setting of the envisioned applica-
tion of the system to be designed, from which require-
ments can be elicited.
A scenario was developed following the People-
Activity-Context-Technology (PACT) framework.
Using this approach forces to think about all the
relevant stakeholders that will be using the new
system, the actions that they perform and the (med-
ical) context in which they perform them, as well
as the technological innovations that are necessary
for successful implementation. Incorporating the
principles of evidence-based medicine into PACT
scenario development provides a starting point for
more effective and efficient design of telemedicine
applications (Huis in’t Veld et al., 2010). On the
one hand, we performed a state of the art literature
research, and on the other hand we assessed the
users medical knowledge and needs by means of
questionnaires, PACT tables and interviews. From
this approach the possibility to have more insight into
the health status of the patient for both patient and
professional became apparent and the clear need to
involve the healthcare professional in the treatment
emerged. Besides the user-centred perspective of
PACT, the “designer-centric” components related to
system use were added to the scenario: Function and
events, Interactions and usability issues, Content and
structure, Style and aesthetics (FICS) (Benyon and
Macaulay, 2002). The FICS approach is more system
descriptive and provides insights for technicians
to consider the technical specifications. It became
apparent that the platform needed a clear distinction
between sensors, the Smartphone, server applications
and web portals, as these are the high level building
blocks for each of our telemedicine applications.
Besides the clear separation of these building blocks,
each of the platform components should have a
modular set up as well, so they can be easily extended
or changed to serve different user groups. Finally,
from the requirements and analysis of the gathered
data, there were strong indicators that the way we
provide feedback to the patients was rather sub-
optimal in terms of its coaching ability. The scenario
was updated, containing PACT elements combined
with FICS elements. From the developed scenario,
requirements were elicited by group discussions in a
participatory design setting, for example conducted
during plenary project meetings where both users
and developers were present. For this purpose,
tables, textual descriptions, and mock-ups were used.
The requirements were prioritized following the
MoSCoW method (must have, should have, could
have, wouldnt have). A must have for the platform
included for example: “The system must continuously
monitor the amount of activity, the activity pattern,
and activity intensity”. The addition of an emergency
alarm function on the other hand was an example
of a could have. Following this iterative design
approach
1
, the platform was designed, implemented
and evaluated. The evaluation covered conceptual
(lessons learned), functional (e.g. usability) and
technical (e.g. battery time) aspects, and the scenario
and requirements were updated accordingly. More
details regarding the evaluation are given in Section
5.
4.2 The Platform
From applying the iterative approach described
above, it emerged that the activity monitoring system
had to be highly flexible and configurable to accom-
modate the various requirements coming from differ-
ent research projects and research goals. Each study
employs its own experiment protocol and the different
1
Multiple groups of end-users (totalling around 50),
covering a variety of patient populations where involved
throughout a number of different projects.
EHST/ICGREEN 2012
22

protocols included different procedures such as use of
a web portal, or showing a graph to the patient, or pro-
viding regular feedback messages, or prompting the
user to answer various types of questions. We also
want to offer support for easy integration of different
sensor types and the possibility to use multiple sen-
sors simultaneously. Figure 2 gives a high level view
of the architecture.
Sensor
Smartphone
Syncer
Server
Syncer
Data
Base
DBServer
Web Portal
Patient
Care Provider
Server
Figure 2: High level architecture overview of the platform.
The individual components are explained in more
detail below.
Sensors. The ProMove-3D wireless sensor was de-
signed to provide a trade-off among performance,
computational and storage resources, wireless capa-
bilities, low-power operation and wearable form fac-
tor. The sensor node can capture, process and com-
municate wireless full 3D motion and orientation in-
formation. The main building blocks of the sensor
node are the following:
• The sensor modules, including accelerometer, gy-
roscope and magnetic compass. All chips are
single-chip, three-axial, fully digital sensors. The
possibility exists to include additional sensors.
• The master microcontroller, which implements all
sensor sampling and handling, synchronization
mechanisms and the application logic.
• The wireless modules. ProMove-3D implements
IEEE 802.15.4 compatible wireless communica-
tion in the 2.4 GHz license-free band as well
as Bluetooth communication through an optional
module.
Through this design, the ProMove-3D becomes a
versatile sensor node supporting a large range of ac-
tivity sensing applications. It can operate as a long-
term activity monitoring device, with low power con-
sumption, long sleep cycles and intermittent wireless
communication for periodic data transfers. At the
other end of the spectrum, it can support high data
rate, full 3D motion and orientation data capturing
and streaming wireless within accurate synchroniza-
tion bounds for accurate motion analysis. Figure 3
shows the sensor node from top, side and bottom. The
side cap is detachable and gives access for charging
the battery. When the cap is attached, the node is au-
tomatically switched on. The node can be worn by
means of a multi-functional clip holder, which allows
various attachments. Two modalities are depicted in
Figure 3: a belt clip, which is meant to be used for
wearing the node around the waist, and an elastic
band clip, which is meant to be used for wrapping the
node with an elastic band, for example around limb
segments.
Figure 3: ProMove-3D node top view with clip holder (left),
side view with belt clip (middle) and bottom view with elas-
tic band clip (right).
Smartphone. In order to ensure flexibility — an
important system requirement — we designed a
Smartphone software framework in which applica-
tions can be defined by linking together various mod-
ules. Each module performs a typically small, clearly
defined task and delivers its output to a central com-
munication module, called the Hub. Other modules
can subscribe to this information and are notified
when new output becomes available. For example: a
BluetoothModule is tasked with opening, maintaining
and closing Bluetooth connections within the device.
As output it delivers a stream of data coming from the
sensor, as well as updates regarding the status of the
connection. A UserInterfaceModule can subscribe to
the status messages and provide the user with a warn-
ing if a Bluetooth connection is lost. Software de-
velopers are free to develop their modules without
specific limitations and, as long as they adhere to the
simple communication protocol with the central Hub,
they can share their output with other modules. In
order to provide the connection between the Smart-
phone and server side services, such as web portals
that provide information to healthcare professionals,
the AndroidSync module takes care of synchronizing
data between Smartphone and server.
Server. On the server side of the platform, the core
component is R2D2 (the Roessingh Research and
Development Database). R2D2 is designed to han-
dle a wide variety of data types such as streaming bio
signal data, questionnaire results, context information
and subject information. R2D2 offers a fixed struc-
ture for storing data uniformly from multiple research
Development and Evaluation of a Sensor-based System for Remote Monitoring and Treatment of Chronic Diseases - The
Continuous Care & Coaching Platform
23

Figure 4: The old (left) and new (right) versions of the
Smartphones and graphical user interface.
projects and applications. This uniform way of stor-
ing data makes it possible to do simple comparison
studies on data gathered by different researchers in
different projects. The design of the data structure is
based on two core principles: (1) the subject is at the
top of the data structure, and (2) all measured data
is linked to a timeline. A subject is an anonymous
participant in a research project and all data that is
measured is subsequently linked to a subject. Fur-
thermore, for all data that is stored, the time at which
the data was gathered is the important factor in link-
ing various layers of data to each other. The subject’s
activity data, for example, is stored in a signal layer
as a constant stream of <time, value>-pairs that indi-
cate their performed activity intensity during the day.
Another layer is used for storing the time at which the
subject received feedback from the system and which
exact message was displayed to the user; these are
events that are stored in an event layer. Similar lay-
ers exist for storing interval data (in which a period of
time can be labelled as e.g. walking or lying), ques-
tionnaire data (in which questionnaire results can be
stored) and video data (if a camera is used for e.g.
gait analysis). Figure 5 shows a screenshot of a data
viewer application, the RRDToolkit, showing various
layers of measured data on a timeline. A server ap-
plication handles secure synchronous access to the
database. Password protected user accounts provide
access to the various sets of data that are stored in the
database, and locking mechanisms are in place to pre-
vent simultaneous write operations, that could result
in data corruption.
Web Portal. To provide a useful view on the data
for biomedical researchers, patients and healthcare
professionals, we designed a modular framework for
developing web portals, in much the same way as the
Figure 5: A screenshot of the RRDToolkit, a data viewer for
researchers, showing an activity graph (signal layer), feed-
back events (event layers) and weather data (interval layers)
for a day of measurement of a Chronic Low Back Pain pa-
tient.
Smartphone application. Different remote monitoring
and treatment applications focus on different types of
measurements and different types of feedback, but a
general component in many applications is a portal
that allows patients and healthcare professionals to
track disease progression or health status. The pri-
mary goal of the web portal is to display measurement
data to the patient or the healthcare professional in an
easy to understand way. Figure 6 shows a screenshot
of the web portal developed within the Dutch “Condi-
tionCoach” project, showing the view for COPD pa-
tients who are able to track their own levels of physi-
cal activity, and progression over the week, month or
year. But the portal can also be used for gathering
new data. For example, an electronic triage applica-
tion was developed for COPD patients where patients
receive a set of questions on their health status (Effing
et al., 2009) on a daily basis via the portal and can give
their responses via the portal. In a trial with COPD
patients, subjects were asked daily if their symptoms
were more severe than normal. If the patient answered
“yes”, they were asked to report on all their symptoms
irrespective of whether the level of each was normal,
slightly increased, or greatly increased. A rule-based
system (an action plan) implemented on the web por-
tal decides when the patient needs to start taking med-
ication. This diary form was successfully used in clin-
ical care as part of a regime of self-treatment of exac-
erbations in COPD patients.
5 EVALUATION
Earlier versions of the platform, and especially the
second platform iteration was extensively evaluated
in trials with different patient groups and their health-
care professionals by means of questionnaires and in-
depth semi-structured interviews. An important out-
EHST/ICGREEN 2012
24

Figure 6: Screenshot of the Dutch CoCo (ConditionCoach)
project web portal, showing a weekly overview of activity
data (center) and links to all the separate available modules
(top) for a patient.
come was the perceived acceptability of the system,
especially by physical therapists.
For C3PO, a small-scale evaluation study was per-
formed to optimize the usability, and to assess inten-
tion of use of the patients. In the Netherlands, six pa-
tients with a clinical diagnosis of stable COPD were
included. COPD is a patient group of mainly elderly
people, who are in many cases not as familiar with
modern technology as younger generations. The ex-
periment was designed to simulate daily use of the
system and daily life activities in a laboratory set-
ting. Each patient wore the system while performing
a number of daily life tasks in the laboratory setting
while the system measured activity levels and gave
feedback. Usability scores were assessed by the Sys-
tem Usability Scale (SUS). For the activity monitor-
ing and feedback a mean SUS score of 67.1 was found
(range: 47.5 - 90.0), which corresponds to the aver-
age scores found in the literature, but also indicated
that usability should be improved. A questionnaire,
specifically designed for the platform, was filled in by
the patients to assess the usability of specific parts of
the system. The questionnaire consisted of 27 state-
ments about the system with a 7-point Likert scale
ranging from ‘strongly disagree’ to ‘strongly agree’.
Example statements include: “The meaning of the
graph is not clear to me” or “I find it easy to un-
lock the Smartphone”. The questionnaire results pro-
vided us with detailed information about every aspect
of the Smartphone application and highlighted further
points for improvement. These improvements were
implemented before clinical trials started and we ex-
pect that the usability score will improve following
the modifications to the application.
The web portal was evaluated in a separate trial.
An evaluation study was carried out into the experi-
ences of end-users during a four week testing period
with the C3PO portal. Data was collected through in-
depth semi-structured interviews with five COPD pa-
tients, two physical therapists, one nurse practitioner
and two lung specialists, and through participative ob-
servations. Five aspects of acceptability of innova-
tions were addressed (relative advantage, compatibil-
ity, ease of use, image, and voluntariness). Quantita-
tive data was used as a secondary source of data pro-
viding supportive information.
There was a perceived high potential acceptabil-
ity, especially to physical therapists. The electronic
diary was considered easy to use and possibly of high
value to both patients and professionals. The use of a
web based portal was accepted by patients but profes-
sionals experienced it as time consuming and hence
professionals’ acceptance was lower than patients’ ac-
ceptance. Quantitative data showed that patients used
the portal at variable hours throughout the day, for 3 to
4 minutes per session. In addition, several points for
enhancing the portal emerged. These improvements
were implemented and, to increase acceptance by the
professionals, the portal was improved in close col-
laboration with the healthcare professionals. Taking
into account the feedback from patients and health-
care professionals allowed us to build a remote mon-
itoring and treatment platform with a high usability
and acceptability for its different classes of end-users.
6 DISCUSSION AND WORK IN
PROGRESS
Over the years many small and larger trials with a
wide variety of patients have been performed, and
following each trial the feedback from the various
users was taken into account. The re-design and re-
implementation of the C3PO platform resulted in a
system that is stable and flexible in operation, as well
as simple to use for patients and healthcare profes-
sionals alike. However, one of the major issues that
arose from the requirements and analysis of older ver-
sions of the platform has not yet been fully addressed.
This concerns automated coaching, the means to pro-
vide real time feedback to the patients on their daily
physical activity in order to encourage behavioural
change. In the current platform, feedback is still
simplistic: feedback messages are presented at fixed
time intervals, related to the amount of activity per-
formed compared to a reference value. Because ef-
fective coaching is a crucial element in affecting be-
havioural change, current research is focussing on de-
veloping an intelligent coach that runs on the Smart-
phone and acts as a personal companion that helps
Development and Evaluation of a Sensor-based System for Remote Monitoring and Treatment of Chronic Diseases - The
Continuous Care & Coaching Platform
25

patients achieve their activity goals. It is based on
the principles that feedback should be tailored to in-
dividual users in terms of its timing, content and style
of presentation to the patient. The next evolution of
the system will be able to learn to predict the opti-
mum timing for providing feedback by analyzing pre-
viously given feedback messages and learning when
a patient is likely to respond well to a given message
by relating relevant context factors to patient compli-
ance (op den Akker et al., 2010). In related work by
Wieringa et al. (Wieringa et al., 2011) the Smart-
phone application also learns to adapt the feedback
message content to the patient. Feedback messages
are stored in a structured manner based on message
content and style. During operation, the system stores
the reaction of the patient to each feedback instance
in order to make informed decisions on which type of
messages are most likely to elicit a positive response
the next time feedback is needed. As for the mode and
style of presentation of feedback to the patient, this re-
mains a significant challenge in Human Computer In-
teraction research. Ongoing and planned research will
evaluate the effects of the smart feedback coach on
patient’s physical activity patterns and their percep-
tion of the system in terms of usability and treatment
compliance. Currently, trials are running in which
COPD patients will use the smart feedback coach for
a period of three months. In the meantime, large scale
evaluations of the remote monitoring and treatment
platform are running in which the platform is used in
a daily clinical care setting. These larger scale eval-
uations will show us how the system performs under
stress and will enable us to receive valuable feedback
on the latest version of the platform which can help
us to keep improving the system.
Based on the results of the research described in
this paper, we are confident that C3PO has the poten-
tial to contribute to delivering more cost effective and
qualitative healthcare. We believe our approach will
be part of the solution by providing more cost effec-
tive rehabilitation and secondary prevention since it
supports self management of patients; thereby shift-
ing the focus of control towards the patient. Using
C3PO the patient can determine where, when and how
intensively he follows his treatment regimen. It also
enables the health care professional to treat more pa-
tients at the same time, decreasing the per-patient cost
of highly trained personnel. Last but not least, auto-
matic data collection is facilitated by the use of this
technology and the data aggregated will result in large
corpora of clinical data which has the potential to sup-
port evidence based medicine. On the one hand it en-
ables an efficient comparison of efficacy of different
interventions, and on the other, data mining can gen-
erate new clinical knowledge of general relevance as
well as determining optimal treatments for a specific
patient.
ACKNOWLEDGMENTS
The C3PO platform is a group effort from the Roess-
ingh Research and Development, Telemedicine Clus-
ter and the authors would like to thank all of our col-
leagues for their commitment to the platform devel-
opment.
REFERENCES
Benyon, D. and Macaulay, C. (2002). Scenarios and the
HCI-SE design problem. Interacting with Computers,
14(4):397–405.
Berg, M. (1999). Patient care information systems and
health care work: a sociotechnical approach. Interna-
tional Journal of Medical Informatics, 55(2):87–101.
Broens, T. H., Huis In’t Veld, R. M., Vollenbroek-Hutten,
M. M., Hermens, H. J., Van Halteren, A. T., and
Nieuwenhuis, L. J. (2007). Determinants of success-
ful telemedicine implementations: a literature study.
Journal of Telemedicine and Telecare, 13(6):303–309.
Burkow, T. M., Vognild, L. K., Krogstad, T., Borch, N. l.,
Ostengen, G., Bratvold, A., and Risberg, M. J. (2008).
An easy to use and affordable home-based personal
eHealth system for chronic disease management based
on free open source software. Studies In Health Tech-
nology And Informatics, 136:83–88.
Carroll, J. (2000). Five reasons for scenario-based design.
Interacting with Computers, 13(1):43–60.
Chen, G., Yan, B., Shin, M., Kotz, D., and Berke, E. (2009).
MPCS: Mobile-phone based patient compliance sys-
tem for chronic illness care. Mobile and Ubiquitous
Systems Networking Services MobiQuitous 2009 Mo-
biQuitous 09 6th Annual International, pages 1–7.
Czabke, A., Loeschke, J., and Lueth, T. C. (2011). Concept
and modular telemedicine platform for measuring of
vital signs, ADL and behavioral patterns of elderly in
home settings. Architecture, pages 3164–3167.
Effing, T., Kerstjens, H., van der Valk, P., Zielhuis, G., and
van der Palen, J. (2009). (Cost)-effectiveness of self-
treatment of exacerbations on the severity of exacer-
bations in patients with COPD: the COPE II study.
Thorax, 64(11):956–962.
Ekeland, A. G., Bowes, A., and Flottorp, S. (2010). Effec-
tiveness of telemedicine: a systematic review of re-
views. International Journal of Medical Informatics,
79(11):736–771.
Hermens, H. J. and Vollenbroek-Hutten, M. M. (2008).
Towards remote monitoring and remotely supervised
training. Journal of Electromyography and Kinesiol-
ogy, 18(6):908–19.
EHST/ICGREEN 2012
26

Huis in’t Veld, R. M., Widya, I. A., Bults, R. G., Sandsj
¨
o,
L., Hermens, H. J., and Vollenbroek-Hutten, M. M.
(2010). A scenario guideline for designing new tele-
treatments: a multidisciplinary approach. Journal of
Telemedicine and Telecare, 16(6):302–307.
Jones, V. M., Hermens, H. J., Leijdekkers, P., and Rienks,
R. (2009). Extending remote patient monitoring with
mobile real time clinical decision support. In Annual
Symposium of the IEEEEMBS Benelux Chapter.
Kumar, S., Kambhatla, K., Hu, F., Lifson, M., and Xiao,
Y. (2008). Ubiquitous Computing for Remote Cardiac
Patient Monitoring: A Survey. International journal
of telemedicine and applications, 2008(iv):459185.
Laplante, C. and Peng, W. (2011). A Systematic Review
of e-Health Interventions for Physical Activity: An
Analysis of Study Design, Intervention Characteris-
tics, and Outcomes. Telemedicine and ehealth: the
official journal of the American Telemedicine Associ-
ation, 17(7):509–523.
Lewis, B., Williams, D., Dunsiger, S., Sciamanna, C.,
Whiteley, J., Napolitano, M., Bock, B., Jakicic, J.,
Getz, M., and Marcus, B. (2008). User attitudes to-
wards physical activity websites in a randomized con-
trolled trial. Preventive Medicine, 47(5):508–513.
op den Akker, H., Jones, V. M., and Hermens, H. J. (2010).
Predicting Feedback Compliance in a Teletreatment
Application. In Proceedings of ISABEL 2010: the
3rd International Symposium on Applied Sciences in
Biomedical and Communication Technologies, Rome,
Italy.
Polisena, J., Tran, K., Cimon, K., Hutton, B., McGill,
S., Palmer, K., and Scott, R. E. (2010). Home
telehealth for chronic obstructive pulmonary disease:
a systematic review and meta-analysis. Journal of
Telemedicine and Telecare, 16(3):120–127.
St
˚
ahl, O., Gamb
¨
ack, B., Hansen, P., Turunen, M., and Haku-
linen, J. (2008). A Mobile Fitness Companion. Sci-
ence And Technology.
United Nations, Department of Economic and Social Af-
fairs, Population Division (2002). World Population
Ageing 1950-2050. United Nations Publications, New
York, USA.
Van Weering, M. G., Vollenbroek-Hutten, M. M., T
¨
onis,
T. M., and Hermens, H. J. (2009). Daily physi-
cal activities in chronic lower back pain patients as-
sessed with accelerometry. European Journal of Pain,
13(6):649–654.
Wieringa, W., op den Akker, H., Jones, V. M., op den Akker,
R., and Hermens, H. J. (2011). Ontology-Based Gen-
eration of Dynamic Feedback on Physical Activity. In
Proceedings of the 13th Conference on Artificial In-
telligence in Medicine (AIME), pages 55–59, Bled,
Slovenia. Springer.
Development and Evaluation of a Sensor-based System for Remote Monitoring and Treatment of Chronic Diseases - The
Continuous Care & Coaching Platform
27
