
Towards a Better Understanding of EHR Systems using Architectural
Views
Liliana Dobrica
1
, Cernian Alexandra
1
and Traian C. Ionescu
2
1
Faculty of Automation and Computers, University POLITEHNICA of Bucharest, Bucharest, Romania
2
SIVECO Romania SA, Sos. Bucuresti-Ploiesti, Bucharest, Romania
Keywords: EHR, HL7, Standards, Architecture Views, Models, UML.
Abstract: The content of this paper addresses the issue of understanding electronic health records (EHRs) systems
under a developer perspective on the existent confusion about this concept. The current standard definition
of EHR is discussed in terms of the main characteristics, data models and functional decomposition for
clinical research. The key components of these models are identified and specified under two considerations
namely, direct care and support. Also they are organized in architectural views describing an EHR system
infrastructure for records management. The value of this work is the architecture centric approach by
creating graphical representations of the system architecture based on top level standard descriptions.
1 INTRODUCTION
All healthcare and scientific authorities worldwide
are realising the importance of developing global
infrastructures for exchange of patient and
healthcare data, services and provide wider
opportunities for clinical research. In European
countries health policy is influenced by the
developments at the international level and by the
standards set by the World Health Organisation
(Ribeiro et al., 2010). Enabling EHR systems
implementations provides many benefits, including
improved access, quality and efficiency of patient
care, as well as promoting research and coordination
of services at lower costs (Vdovjak et al., 2012)
(Bonney, 2012) . Nowadays an integrated system in
the health care domain represents one of the most
challenging problem. Its realization is not only
difficult, but also poorly understood by system
developers. The literature very clearly indicates that
a clean, simple and easy to operate concept of an
EHR system does not exist (EHR-IMPACT, 2008).
Among the requirements and constraints that have to
be satisfied we can mention a higher diversity and
complexity, increased quality, productivity and reuse
content, standardization. Due to the escalating
complexity level of EHR systems and the
technology trends, a coherent and integrated strategy
for EHR systems development is required.
Architecture-based development of a system is a
solution to solving these problems. There are well-
known benefits of the introduction of this concept in
the life-cycle development of software systems.
Architecture is considered the first asset in an
architecture-centric development process and from
this point of view an analysis at this level should
reveal requirements conflicts and incomplete design
descriptions from a particular stakeholder
perspective. Many research efforts have been
concentrated on ensuring that these major issues are
addressed at the architectural level.
This paper introduces the EHR vision shedding
also light on the existent confusion about this
concept. In literature several types of health records
have been used with approximately the same
meaning. The current standard definition of EHR is
discussed in terms of the main characteristics and
their variability of levels in sharing patient health
information. Thereafter, the key components of an
EHR system are identified and discussed under
various considerations.
In particular, the rest of this paper is structured as
follows: Section 2 presents an overview of the EHR
definition and architecture-based software systems
development concepts. The major concepts that
could be included in data and functional models with
the focus on architectural structural and behaviour
views are detailed and graphically represented in
section 3. Conclusions state the value of
362
Dobrica L., Alexandra C. and C. Ionescu T..
Towards a Better Understanding of EHR Systems using Architectural Views.
DOI: 10.5220/0004246603620365
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 362-365
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

architecture-centric development of integrated EHR
systems.
2 EHR OVERVIEW
The idea of EHR was born as an alternative to an
existent healthcare system (Waegemann, 2003). The
added value of EHR services aims to improve
patient safety, quality and efficiency of patient care,
and reduce healthcare delivery costs. (Hoffman and
Podgurski, 2008). The major value of integrated
EHRs is that they collect data once, then use it
multiple times to serve different needs of the
administrator to obtain data for billing, a nurse to
report an adverse reaction, and a researcher to
analyze the efficacy of medications (MITRE, 2006).
EHR has been a key research in medical
informatics for many years. The literature provides
several concepts that are used with approximately
the same meaning including Personal Health Record
(PHR), Electronic Medical Record (EMR),
Electronic Patient Record (EPR), Electronic Health
Record (EHR) and Computerized Patient Record
(CPR). Most of them refer to the electronic
collection of medical information, performed by the
patient himself or herself, by a particular healthcare
institution, or by a global, integrated system. Overall
it is a systematic collection of electronic health
information about individual patients or populations
in a digital form. In particular, electronic health
record is defined as “digitally stored health care
information about an individual’s lifetime with the
purpose of supporting continuity of care, education
and research, and ensuring confidentiality at all
times” (Iakovidis, 1998). An idealistic definition and
concept, probably not yet brought to real life is that
“EHRs are repositories of electronically maintained
information about individuals’ lifetime health status
and healthcare, stored such that they can serve the
multiple legitimate users of the record” (EHR-
IMPACT, 2008). EHR contains all possible health
relevant data of a person and other health-related
information, always established beyond an
institutional framework (regional, national, global),
web-based, and participation of citizen in creating
the record (Edwards, 2007). HIMSS Analytics
differentiates between EMR and EHR in order to
reduce confusion (Garets and David, 2006).
EHR complexity resides in a multitude of
interdependent elements which must be organized.
To handle this complexity, a software architectural
(SA) approach is necessary as it helps to consider
separation of concerns realized through different
levels of abstraction, dynamism and aggregation
levels and (static/dynamic, local/global,
functional/extra-functional) (Dobrica and Ovaska,
2010). As is often the case in the field of eHealth,
the knowledge acquired in software engineering is
not really exploited, although it helps to manage
complexity. In particular, they can be used to
develop EHR systems architecture. SA description is
designed to address the different perspectives one
could have on the system. Each perspective is a view
(Bass et al, 2011).The information relevant to one
view is different from that of others and should be
described using the most appropriate technique.
Several models have been proposed that include a
number of views that should be described in the
software architecture. The view models address the
static structure, the dynamic aspect, the physical
layout and the development of the system. In
general, it is the responsibility of the architect to
decide which view to use for describing SA.
3 EHR SYSTEM MODELS
A clear distinction is made between the EHR and an
EHR system. The standard ISO/TR 20514:2005
discusses about two different views of the scope of
the EHR, which are Core EHR and Extended EHR.
Core EHR is limited to clinical information and is
defined by the requirements for its record
architecture. It is based on the adoption of the
system-of-systems approach. This allows more
modular health information systems to be built,
ranging from a simple environment with just the
EHR, a terminology service and some reference
data, to a much bigger and more elaborate
environment including many additional services
such as decision support, workflow management,
order management, patient administration, billing,
scheduling, resource allocation, etc. Extended EHR
is a superset of the Core EHR and includes not only
clinical information, but the whole health
information landscape.
Currently there is a standardization effort
towards consensus on EHR system functionality
(ANSI/HL7 EHR CRFP, 2009) in the definition of
an EHR system functional model and functional
profiles for various dedicated functionalities
including clinical research (EHR-CR) (ANSI/HL7
EHR CRFP, 2004). The EHR system functional
model is decomposed in three important sections:
Direct Care, Supportive and Information
Infrastructure. These sections gather functions which
are grouped in several important categories and sub-
categories. An UML Component diagram as shown
TowardsaBetterUnderstandingofEHRSystemsusingArchitecturalViews
363
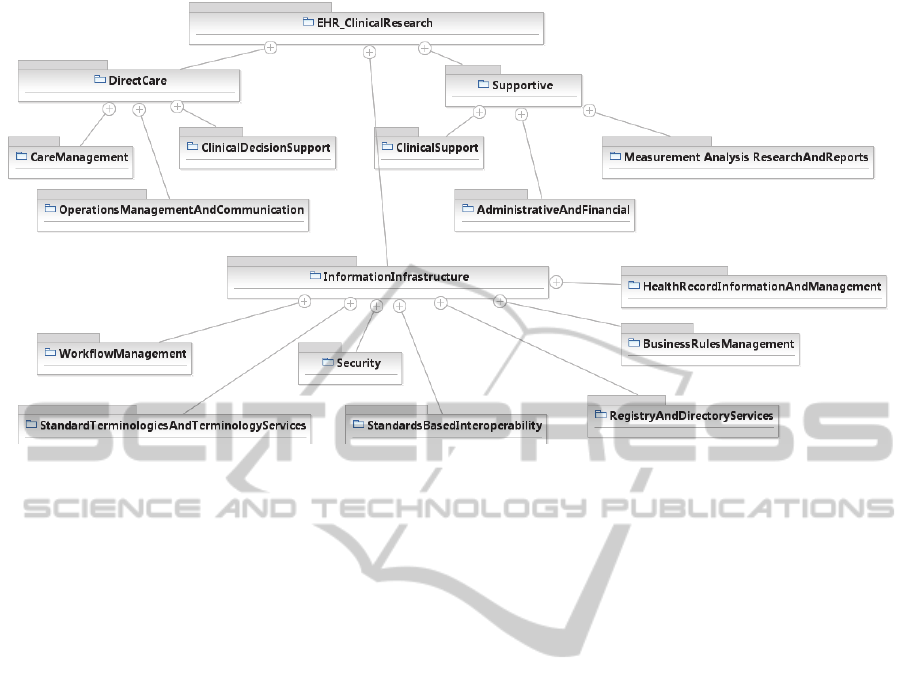
Figure 1: EHR – CR functional model.
Fig. 1 presents the EHR functional model for a
better understanding of the domain, concepts and
relations among them.
EHR-CR data model may be graphically
represented as an UML Class Diagram. Complex
data types specified by names, attributes and
operations are interconnected based on composition,
aggregation, generalization or other association
relationships. The static aspect is represented and
realized by attributes and behaviour/ dynamic aspect
is visible and realized by using operations of classes.
HL7-CR Direct Care Data Model includes classes
such as Electronic Health Record, Patient,
PatientRecord, Demographic Information,
PatientDeographics, KeyDemographic Information,
PatientHistory, etc. PatientRecord Class includes
attributes such as ID, Name, Demographic
Information, LabResults, Current medication lists
and Problem List. Behavior is given by operations
like create, identify, maintain and,
calculatePatientAge.
A standardized solution of EHR Records
Management based on a HL7 needs to pay attention
to six key infrastructure components: security, health
record information and management, standard
terminologies and terminology services, standards-
based interoperability, business rules management
and workflow management. A conceptual structural
view, based on UML component diagram is
represented in Fig. 2.
4 CONCLUSIONS
In this paper we analyzed the recent standards on
EHR-related concepts to facilitate exchange of
EHRs between EHR systems. The aim was the
understanding of standard requirements in order to
develop compliant EHR systems. Our method was
based on architecture-centric software systems
development. The current standard definition of
EHR concept has been discussed in terms of the
main characteristics, data models and functional
decomposition for clinical research. The key
components of these models have been identified
and specified under various considerations namely,
direct care and support. Also they have been
organized in architectural views describing an EHR
system infrastructure for records management. The
value of this work is the architecture centric
approach by creating graphical representations of the
system architecture based on top level descriptions
of standards.
Our approach based on architectural views has
an immense potential to improve the understanding
of EHR systems as well as reduce time and risks in
development stages. However, for this approach’s
success it is necessary to create a cooperation culture
among stakeholders.
HEALTHINF2013-InternationalConferenceonHealthInformatics
364

Figure 2: HL7 EHR records management profile.
ACKNOWLEDGEMENTS
This work is supported by a grant of Romanian
National Authority for Scientific Research CNDI-
UEFISCDI, project number E! 7201 and the
European Research Project Linked2Safety
(www.linked2safety-project.eu).
REFERENCES
Iakovidis I.,1998. Towards personal health record: current
situation, obstacles and trends in implementation of
electronic healthcare record in Europe, Int. J. Medical
Informatics 52, 128, 105-117
EHR-IMPACT, 2008. D1.2. Report on the conceptual
framework of interoperable electronic health record
and ePrescribing systems, EHR Impact project, 2008,
accessed www.ehr-impact.eu
Dobrica L, Ovaska E, 2010. Service based development of
a cross domain reference architecture, in
Communications in Computer and Information
Science, vol. 69, pp. 305-318, Ed. Springer
Bass L., P. Clements, R. Kazman, 2011. Documenting
software Architecture, Ed. Addison-Wesley
Edwards E., Gartner Research. 2007 Electronic Health
Records: Essential IT Functions and Supporting
Infrastructure
Garets D., M. Davis, 2006. Electronic Medical Records vs.
Electronic Health Records: Yes, there is a difference,
A HIMSS Analytics White Paper
MITRE. 2006. NIH National Center for Research
Resources, Electronic Health Records Overview. The
MITRE Corporation
Ribeiro, L., Kunha J.P., Cruz-Correira R., 2010.
Information Systems Heterogeneity and
Interoperability inside Hospitals – A survey, Procs of
Int. Conf HEALTHINF, pp. 337-343
Vdovjak R., Claerhout B, Bucur A., 2012. Bridging the
gap between clinical research and care. Procs of Int.
Conf HEALTHINF, pp. 281-286
Bonney W., 2012. Enabling factors for achieving greater
greater success in electronic medical record initiatives.
Procs of Int. Conf HEALTHINF, pp. 5-11
Hoffman S, Podgurski A.2008. Finding a Cure: The Case
for Regulation and Oversight of Electronic Health
Record Systems. Harvard Journal of Law and
Technology 22. 2008;(no. 1):107
ISO/TR 20514:2005. 2005. Health Informatics –
Electronic Health Record – Definition, scope and
context
Waegemann P. 2003. EHR vs. CPR vs. EMR, Healthcare
Informatics
ANSI/HL7 EHR CRFP, R1-2009, 2009. HL7 EHR
Clinical Research Functional Profile, Release 1
HL7 EHR System Functional Model. 2004. A major
development towards consensus on Electronic Health
Record System Functionality, A White Paper
TowardsaBetterUnderstandingofEHRSystemsusingArchitecturalViews
365
