
SOA and Cloud based Architecture for Non-invasive Health
Monitoring
Mohamed Adel Serhani, Elarbi Badidi and Abdelghani Benharref
College of Information Technology, UAE University, Al-Ain, U.A.E.
Keywords: Chronic Diseases, Monitoring, Prevention, SOA, Cloud Computing.
Abstract: The increasing incidence of chronic diseases is becoming a heavy burden for both public and private
healthcare sectors. Many industrial and academic efforts are trying to alleviate this burden using various
clinical solutions. Establishment and execution of prevention plans and subjects’ monitoring are among the
promising solutions. In keeping with these efforts, we describe in this paper our proposed architecture, for
health monitoring of patients with chronic diseases. The architecture relies on the service Oriented
Architecture (SOA) and cloud computing for the implementation and integration of services from various
stakeholders. The monitoring scheme allows to proactively detect risks of disease’ aggravation and
dynamically generates and customizes prevention plans according to the patient’s health profile and context.
A prototype of our system is under development and preliminary data have been collected and analysed.
1 INTRODUCTION
Chronic and cardiovascular diseases (CVD) are
increasing at an unprecedented rate all over the
world. For instance, in the United Arab Emirates
(UAE) over 25% of fatalities in the UAE are caused
by cardiovascular diseases (BIM, 2010). Multiple
factors contribute to the prevalence of these
diseases: cholesterol, diabetes, high blood pressure,
physical inactivity, and smoking. Consistent with
statistics from the World Health Organization, the
UAE has the second highest rate of diabetes in the
world. Furthermore, research studies at the UAE
University estimate that up to 29% of the population
over 30 years old of the UAE has diabetes.
To tackle the rising incidence of chronic diseases
and their associated complications, a prevention
approach can contribute to reducing the risks of their
occurrence. Likewise, continuous monitoring of
subjects’ health condition is vital for detecting the
diseases’ symptoms as early as possible.
The implementation of monitoring, prevention,
and tracking mechanisms is becoming possible due
to the integration of different technologies, systems,
and communication infrastructures. These
technologies include sensing, pervasive computing,
and wireless and mobile computing technologies.
They are greatly impacting the healthcare industry,
which is undergoing fundamental changes by: (1)
Shifting from hospital-centric services to ubiquitous
and ambulatory systems (with homecare, day-care
clinics, remote healthcare), (2) Providing support for
the treatment of chronic diseases through active
involvement of patients, (3) Providing patients and
healthcare professionals with easy access to
important health information anytime/anywhere, and
(4) Optimizing healthcare costs.
In this paper, we propose an architecture for
monitoring and prevention of chronic diseases. The
system relies on SOA and cloud computing. SOA
has proven to be an adequate solution for integrating
heterogeneous systems, allowing application-to-
application communication over the internet,
reducing cost of integration, and making data
available to different stakeholders. The system will
allow deploying various services for continuous data
gathering, automatic monitoring, and taking
proactive measures to identify risk factors and
prevent subjects from severe heath consequences.
These services can be accessed from any computing
systems, and from mobile handheld devices smart-
phones and tablets. Besides, the system can be
integrated with other healthcare systems.
The remainder of this paper is organized as
follows: Section 2 discusses the state of the art in
health monitoring. Section 3 portrays our proposed
architecture for non-invasive health monitoring,
386
Adel Serhani M., Badidi E. and Benharref A..
SOA and Cloud based Architecture for Non-invasive Health Monitoring.
DOI: 10.5220/0004253103860389
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 386-389
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

which relies on SOA and cloud computing
technologies, and describes the monitoring process.
Section 4 presents the implementation and the
experiments we conducted. Section 5 concludes the
paper and highlights some future works.
2 RELATED WORK
Several research works and initiatives have
investigated the challenges of building e-health
solutions. These solutions differ on how they tackle
the integration issue given the heterogeneity of
systems, middleware, and architectures used to build
an e-Health system. Xiang et al. (Xiang et al., 2003)
proposed a distributed framework for a Web-based
telemedicine system, which uses CORBA
technology and a database fragmented on different
sites. The system requires an intermediary
middleware to handle the heterogeneity of heath
systems and huge development effort to adapt the
system to the integrated system requirements.
In (Omar and Bendiab, 2006), the authors
proposed a multi-layer SOA-based e-Health services
architecture, which has six main components that
define the interactions among the layers. The system
is generic. However, it describes only the
architectural design without detailing the
implementation and its challenges. In addition, their
proposed system hasn’t been implemented. Kart, F.
et al. (Kart et al., 2008) described a distributed e-
healthcare system that uses SOA as a mean of
designing, implementing, and managing healthcare
services. The users of the system are physicians,
nurses, pharmacists, and other professionals, as well
as patients. The system includes a clinic module, a
pharmacy module, and patient’s interfaces, which
are implemented as Web services. Various devices
can interact with these modules, including desktop
and server computers, Personal Digital Assistants
and smart phones, and even electronic medical
devices, such as blood pressure monitors.
The authors in (Hsieh et al., 2007) described the
design, the implementation, and the deployment of a
multi-tier Inpatient Healthcare Information System
based on SOA and on the HL7 message exchange
standard at the National Taiwan University Hospital
(NTUH). The services-tier includes Computerized-
Physician Order Entry (CPOE), Billing, Pharmacy,
and Diet. The authors in (Juneja et al., 2009)
investigated how healthcare organizations, using
SOA, can leverage their shared services to automate
multiple business processes and reinforce overall
interoperability. The authors in (Yang et al., 2008)
designed and developed a SOA-based platform for
home-care delivery to patients with chronic diseases.
This work shares some of the goals with our project
with regards to monitoring chronic diseases patients.
To promote interoperability among healthcare
organizations that are seeking to develop SOA-based
architectures, a joint collaboration effort among
standards groups, specifically HL7 and the Object
Management Group (OMG), was formed under the
name: Healthcare Services Specification Project
(HSSP). This effort intends to develop health
industry SOA standards. The intent of HSSP is to
produce standard services that define services’
responsibilities, behaviour, and interfaces so that
ubiquity can be achieved across implementations
and vendor products (HL7 and OMG, 2008).
Our solution is aligned with above initiatives and
addresses mainly the chronic diseases monitoring
and prevention. It also addresses some difficult
issues in the design of an e-health system and
protection of medical data. Our solution relies on
SOA to integrate different systems, data, and make it
available for CDs monitoring, and prevention. The
net implication of using SOA in our solution is that
it facilitates interoperation among various systems
that typically do not speak the same language. Using
a common SOA reduces the complexity of the
integration of heterogeneous systems. New services
can be developed to satisfy the needs of integration,
and existing system capabilities can also be
organized into services.
3 HEALTH MONITORING
ARCHITECTURE
3.1 Architecture Overview
Figure 1 depicts our proposed architecture for health
monitoring that allows the collection of health data
of patients and its dissemination to healthcare
professionals anytime and from everywhere. The
architecture takes advantage of the recent advances
in sensing technology, wireless and broadband
communication, computing capabilities of handheld
devices, services’ delivery, and cloud computing to
enable smart monitoring of patient’s vital health
parameters. Each layer of the architecture includes a
set of components that interact to provide an
integrated solution for monitoring patients’ health.
Non-Invasive Sensing Layer: this layer includes
various devices (e.g. sensors, smart-phones), which
sense one or more health parameters such as
SOAandCloudbasedArchitectureforNon-invasiveHealthMonitoring
387
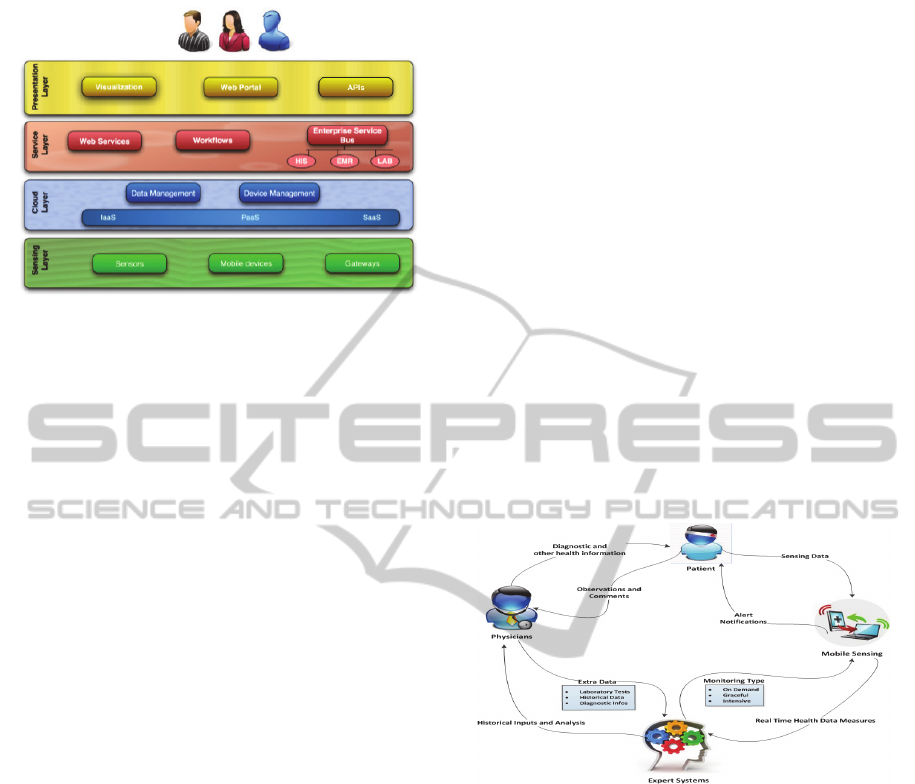
Figure 1: SOA & Cloud based Architecture for
Non-Invasive Health Monitoring.
blood pressure, blood sugar, body temperature, and
oxygen saturation. It also includes gateways that
collect data from sensors, perform some processing
(e.g. filtering), and store data on the Cloud.
Gateways generally provide an interface to access
and retrieve sensed data.
Cloud Layer: this layer serves as the underlying
infrastructure and platform that hosts data and
applications. It includes the following components:
Connectivity Management, Device Management,
Data Processing, and other cloud-based services that
support monitoring activities.
Service Layer: this layer allows integrating the
components involved in the monitoring process with
services of the healthcare information system. The
main components of this layer are: the Enterprise
Service Bus (ESB), which allows interoperation and
exchange of data among different sub-systems, Web
services, and Workflows Management.
Presentation Layer: this layer includes high-level
applications and services that access and process
health data obtained from the lowest layers of the
architecture. Examples of services are: report
generation, pattern mining and recognition tools, and
data visualization.
3.2 Monitoring Process
The monitoring process involves the patient,
healthcare professionals, sensing devices (mobile,
Sensors), and the engine system. The sensing
devices sense the patient’s health parameters and
send real-time data to a back-end server, which
includes a smart engine that processes and mines
collected data to detect any discrepancies in the
patient’s health data and report them to healthcare
professionals to take appropriate actions. The engine
offers a set of services to physicians and to the
patient’s assistance team. These services render
various kinds of data such as laboratory tests,
demographic, anthropometric, and biological data,
which support physicians in taking appropriate
actions.
Figure 2 depicts interactions among main
monitoring actors. Collected data is sent to a mobile
device, which stores it in a cloud repository. Once
the data is available on the Cloud, the surveillance
centre of a hospital can access these data and notify
appropriate health professionals if immediate action
is required in response to any observed irregularities
of monitored health parameters. Also, physicians
can access the cloud to retrieve historical data of the
patient for further investigation purpose. They can
recommend prevention and action plans for the
treatment of the patient conditions. A prevention
plan may recommend, for instance, practicing
regular sport exercises, following a diet plan,
changing the food habits and the lifestyle, etc. An
action plan, however, consists of a series of actions
that might include medications, re-education, etc.
Figure 2: Mobile health monitoring process.
4 IMPLEMENTATION
We conducted a series of experiments to monitor
and collect data about temperature, blood pressure,
ECG, heart rate, and blood sugar of some subjects.
Sensors sensed real-time data and transmitted it to a
mobile device (Samsung Galaxy Note running
Android 4), which stored them in a Cloud data
repository. We developed a mobile application to
parse the data stored in the cloud to generate,
visualize, and interpret the monitoring results.
Figure 3 depicts the main interface of the
application.
HEALTHINF2013-InternationalConferenceonHealthInformatics
388

Figure 3: Snapshot of the mobile health application.
Figure 4 shows results of monitoring the ECG;
the user can scroll left or right to see rest of graph.
Figure 4: Results of ECG monitoring.
Figure 5 shows a graph that resulted from
monitoring a patient blood sugar while fasting and
after meals for a period of 40 days.
5 CONCLUSIONS
With the advances in sensing technology,
monitoring the health of patients using diverse non-
intrusive sensors is becoming a promising solution
for dealing with the increasing incidence of CD
worldwide. Monitoring allows to continuously
observe vital parameters such as temperature, blood
pressure, and ECG of a patient.
In this paper we described our proposed
architecture, for health monitoring of patients with
chronic diseases. It uses the SOA and cloud
computing technologies to implement and integrate
services from various stakeholders. Its monitoring
scheme allows to proactively detect risks of disease’
aggravation and to dynamically generate and
customize prevention plans consistent with the
patient’s health profile and condition. A prototype of
our system is under development. We collected and
analysed preliminary data of few patients.
Figure 5: Results of blood sugar monitoring.
ACKNOWLEDGEMENTS
This work is sponsored by UAE University under
NRF grant #21T020.
REFERENCES
BIM, 2010. Over 25% of deaths in the UAE are caused by
cardiovascular disease. http://www.bi-me.com/
main.php?id=46797&t=1&c=35&cg=4&mset=.
HAAD, 2011. Public Health Priorities and Goals.
http://www.haad.ae/haad/tabid/228/Default.aspx.
HL7 & OMG, 2008. The practical Guide for SOA in
Health Care: A real World Approach to Planning,
designing, and deploying SOA, version 1.0.
http://hssp.wikispaces.com/PracticalGuide.
Hsieh, S., Weng, Y., Yang, T., Lai, F., Cheng, P., Ping,
X., Jan, M., Lin, J. & Peng, C., 2007. Middleware
based inpatient healthcare information system. In
Proc. of BIBE 2007, the 7th IEEE International
Conference on Bioinformatics and Bioengineering.
Juneja, G., Dournaee, B., Natoli, J. & Birkel, S. 2009.
SOA in healthcare (Part II). SOA Magazine.
Kart, F., Moser, L. E. & Melliar-Smith, P. M., 2008.
Building a distributed e-healthcare system using SOA.
IT professional, 10, 24-30.
Omar, W. M., & Bendiab, A. T., 2006. E-health support
services based on service-oriented architecture. IT
professional, 8, 35-41.
Xiang, Y., Gu, Q. & Li, Z., 2003.A distributed framework
of Web-based telemedicine system. In Proc. of CBMS
2003, the 16th IEEE Symposium on Computer-Based
Medical Systems, 108-113.
Yang, C. L., Chang, Y. K. & Chu, C. P, 2008. Modeling
Services to Construct Service-Oriented Healthcare
Architecture for Digital Home-Care Business.In Proc.
of SEKE'2008, the International Conference on
Software Engineering & Knowledge Engineering.
Sum m ary of T est R esults
Y ou resu lts sh ow irregu lar v alu es o f B loo d Sugar,
especially after m eals.
N orm al B S Fasting < 1 20 m lg
N orm al Po st B S < 150 m lg
Advices
Adjust your meals
Practice sp o rt
Take eno ugh rest
Consult a physician
SOAandCloudbasedArchitectureforNon-invasiveHealthMonitoring
389
