
Strong and Meaningful Use of Healthcare Information Systems (HIS)
Arkalgud Ramaprasad
1, 2
and Thant Syn
1
1
School of Business Administration, University of Miami, 5250 University Drive, Coral Gables, FL, U.S.A.
2
College of Business Administration, University of Illinois at Chicago, 601 S Morgan Street, Chicago, IL, U.S.A.
Keywords: Ontology, Meaningful Use, Healthcare Information Systems, Electronic Health Records.
Abstract: The translation of science to practice to policy for meaningful use of healthcare information system (HIS) is
embedded in a complex milieu of meaningful, meaningless, non-, and mis- use of the system by a variety of
stakeholders seeking to manage the cost, quality, safety, and parity of healthcare. The problem of HIS use
can be modeled as an ontology which encapsulates the core logic of use. The ontology includes the three
components of translation, the four types of use, the key stakeholders, and the four basic outcomes. It is a
comprehensive structured natural-language model which can be extended and refined. It is parsimonious
and can be easily understood and interpreted by all the stakeholders. We argue that such a model is
necessary to develop a roadmap for strengthening the meaningful use of HIS. In its absence meaningful use
of HIS will be weak.
1 INTRODUCTION
A strong science is a foundation for effective
practice; a deep knowledge of practice is a
foundation for effective policies; and an ongoing
assessment of the outcomes of the practices and
policies provides feedback to redirect the science,
practice, and policies. We draw upon Platt’s (Platt,
1964) concept of ‘strong inference’ to articulate the
concept of strong science, practice, and policy as
disciplines which will help clearly resolve
equivocalities at each stage of translation. For the
continuous translation of science to practice to
policy and the feedback to be effective, the
translation/feedback focus has to be symmetrical.
The dysfunctions of asymmetric focus in
healthcare are evident from history. It took a long
time for the US health system to emphasize the
prevention of illnesses as much as it did their cure,
increasing the cost of healthcare. A recent study
highlighted the cost of the focus on breast cancer
cure to the exclusion of its prevention from
consideration (Interagency Breast Cancer and
Environmental Research Coordinating Committee,
2013). Similarly, while there are many studies of
health disparities, there are very few of health
parities, disease parities, and disease disparities. In
PubMed literature between 2002 and 2012, the
dominant – almost exclusive – focus is on health
disparities (Ramaprasad and Thirumalai, 2012).
Last, while there is voluminous literature on
eliminating obesity there is very little on increasing
the opposite of obesity, for which there isn’t even a
formal word – even the language comes in the way.
Should the opposite of obesity be called normalcy,
un-obesity, non-obesity, or nobesity?
As healthcare information systems (HIS) have
become central to the delivery of healthcare, the
science, practice, and policy of their use have
become an important concern. The science of use of
HIS is focused on the technical design of the
systems, human-computer interactions, and the
cognitive, behavioral, and social aspects of its use.
The practice of use of HIS is focused on the
implementation of the systems, managing the
change, and the outcomes of the change. The
policies of the use of HIS are focused on guidelines
at the different levels of healthcare institutions
(clinics, hospitals, etc.), governments (local, state,
federal, etc.), and other stakeholders about their use.
Ideally the science, practice, and policy have to be
aligned – the challenge is to do so.
While in the US a staged plan to encourage their
use, with incentives, goals, and measures has been
introduced, the issue is of concern in other countries
too. This paper plays off the phrase ‘meaningful use’
coined in the US for the purpose. The staged
incentive program has spawned a considerable
381
Ramaprasad A. and Syn T..
Strong and Meaningful Use of Healthcare Information Systems (HIS).
DOI: 10.5220/0004870303810386
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2014), pages 381-386
ISBN: 978-989-758-010-9
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)
amount of literature on the science, practice, and
policy of meaningful use. We argue that such a
focus is asymmetric and hence will be ineffective.
While the phrase may correctly describe the desired
state of the use of HIS, to achieve it one has to study
the use in the context of other possible states,
namely: meaningless use, non-use, and mis-use.
For example, consider the implementation of
drug-drug and drug-allergy interaction checks.
These checks will directly affect the quality and
safety (Crosson et al., 2012, Rahmner et al., 2012,
Spina et al., 2011) outcomes of healthcare (Classen
et al., 2011). Their effectiveness will depend upon
the providers’ response to the alerts issued based on
the checks. Recent assessment shows that more than
90% of the alerts are overridden due to alert fatigue
(Smithburger et al., 2011, Phansalkar et al., 2012b,
Crosson et al., 2012), information overload (Callen
et al., 2011), poor user interface Design (Seidling et
al., 2011, Gaikwad et al., 2007, Rahmner et al.,
2012), poor specification of the critical interactions
(Gaikwad et al., 2007), and inadequate analysis
(Phansalkar et al., 2012a, Takarabe et al., 2011) of
the interactions.
Thus the alternatives to meaningful use are not
just a semantic play on words but realities in the
context of many information systems, including
HIS. A user going through the motions of using a
system, just for appearance, while not really
integrating it into his or her decision making
processes would be an example of meaningless use.
Idle information systems and functionalities are a
common occurrence indicating non-use. Worse, use
of the system for fraud would be misuse – an
important concern given the escalation in healthcare
fraud. Instead of considering any use other than
meaningful use as being simply aberrant, it would be
appropriate to consider them as part of the use
continuum.
The dynamics of meaningful use are not
necessarily the opposite of that of meaningless use;
the dynamics of non-use are not simply the opposite
of use. An asymmetrical science of meaningful use
of HIS will result not only in a weak science but also
in weak practices and policies too. A symmetrical
approach to HIS use is needed. We argue that
meaningful use of HIS has to be studied explicitly in
conjunction with meaningless use, non-use, and mis-
use of these systems to develop (a) a strong science
of use of HIS, and (b) translate the science into
strong practices and policies for use of HIS.
All the four types of use coexist in any HIS, in
different proportions. Expert stakeholders may use it
meaningfully; novice stakeholders may use it
meaninglessly or not use it; and fraudsters may
misuse it. Incentivized stakeholders may use it
meaninglessly, enough to obtain the incentives; non-
incentivized stakeholders may not use it at all. How
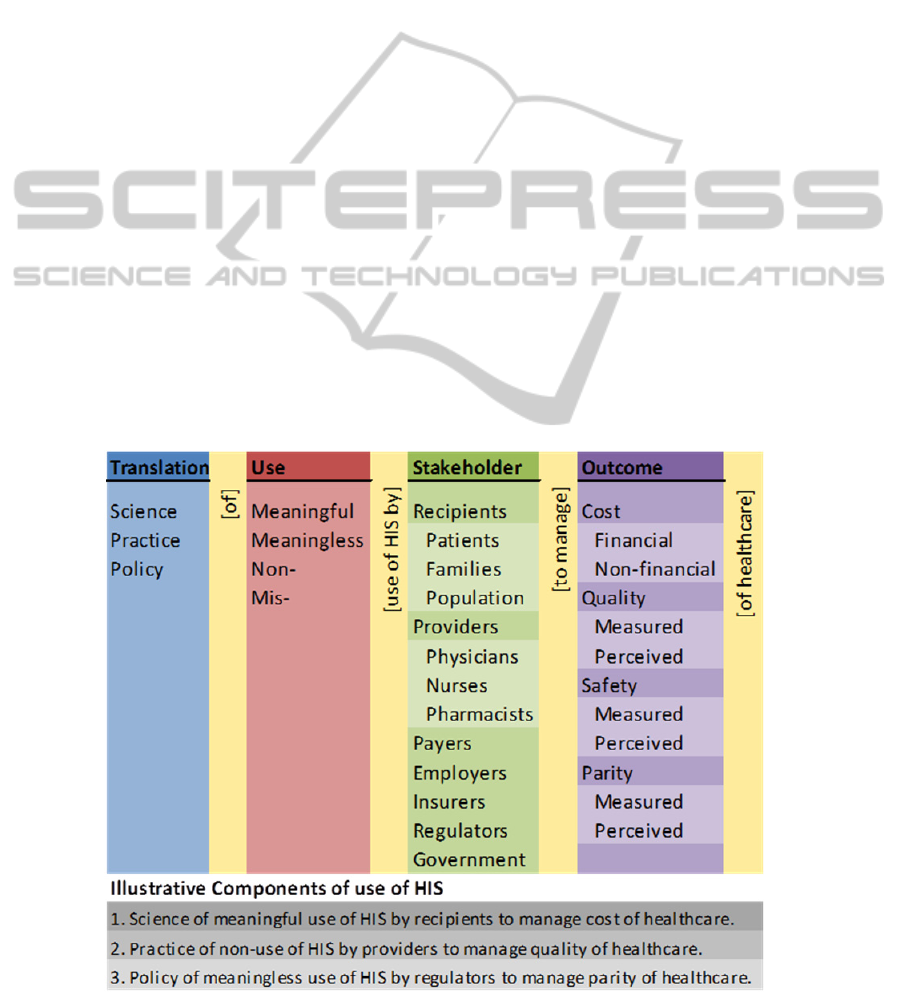
Figure 1: Ontology of Use of Healthcare Information Systems.
HEALTHINF2014-InternationalConferenceonHealthInformatics
382

much the stakeholders, as a whole, use it
meaningfully, meaninglessly, not at all, or misuse it
will determine the impact of HIS on cost, quality,
safety, and parity of healthcare – the four outcomes
sought from the meaningful use programs. It would
be foolhardy to expect that the HIS will be used
meaningfully to the complete exclusion of non-use
and meaningless use. The combinations of
translation (Science, Practice, and Policy), use,
stakeholders, and outcomes of HIS use have to be
addressed systemically, systematically, and
symmetrically to transform healthcare.
The use of HIS in healthcare described above is
complex problem. Its complexity has to be
deconstructed. Its core logic and all the components
can be conceptualized using the ontology shown in
Figure 1. It is a structured natural language model of
the problem. It can be used to analyze the extant
literature and develop a roadmap for the science,
practice, and policy of HIS. We will discuss the
construction of the ontology and application to
developing the roadmap.
2 ONTOLOGY OF USE OF HIS
We have conceptualized the ontology of use of HIS
along four dimensions, namely: (a) Translation, (b)
Use, (c) Stakeholder, and (d) Outcome. In the
following we will discuss each dimension.
There is nothing sacrosanct about these four
dimensions – it is simply the lens through which we
have chosen to study the problem. They are
parsimonious and fundamental for the task at hand.
One could conceivably add a spatial dimension to
study geographical differences or add a temporal
dimension to study the evolution of meaningful use.
These dimensions can be added in subsequent
analysis too, if necessary, because the ontology is
extensible.
2.1 Translation
Science, Practice, and Policy are separate knowledge
domains yet tightly connected. The Translation
dimension encapsulates the continuous process of
translation of (a) science to practice, and (b) practice
to policy. It also encapsulates the continuous
feedback (a) from practice to science, and (b) from
policy to practice and then to science.
The Translation dimension is shown as an
ordinal taxonomy of the three elements in Figure 1 –
it presumes the commonly used order of translation
from Science to Practice to Policy. The order may be
changed to reflect a different point of view. Or, they
could be simply considered to be nominal. Should
one modify the translation process by adding another
step or refining an existing one, the modification can
be encoded in the dimension as an additional
category or subcategory. For example, Assessment
may be added as a fourth element of Translation, or
Science may be subcategorized into Basic and
Applied sciences.
The translation and feedback processes are
neither natural nor automatic. In the absence of these
continuous links, the three will tend to become
disconnected and ineffective. There are significant
incentives for disconnection and disincentives for
integration. The different disciplinary homes for the
three domains are an incentive for disconnection.
The lack of support for interdisciplinary work is a
disincentive for integration. The lack of seriousness
about assessment and learning is both an incentive
for disconnection and disincentive for integration.
Findings from the emerging discipline of
translational science should help, in the long run.
However, the new science is primarily focused on
translation of biomedical research and not HIS.
2.2 Use
Meaningful use has been very salient in the
literature, especially due to the incentive program
instituted by CMS (Blumenthal, 2009). It is a good
phrase; it is desirable; but, an exclusive focus on it is
dysfunctional. Meaningless use, which can be
construed as the opposite of meaningful use, has
been suggested in criticisms of HIS but has not been
a significant object of study, as for example in the
context of alert overrides discussed earlier. One
underlying assumption may be that the two are
mutually exclusive complementary categories, as a
consequence of which the presence of one is seen as
an indicator of the absence of the other. Thus
increase in one would result in a decrease of the
other – a zero-sum situation. However, the
complementary assumption would be incorrect if the
two are concurrent categories, both coexisting
simultaneously. The zero-sum assumption would not
hold. Both meaningful and meaningless use could
vary independently. We believe the two are
concurrent.
Similarly, non-use is often seen as an indicator of
the failure or ineffectiveness of an HIS, but not as an
explicit object of study. It should be considered as
such in the use spectrum. It may be a sign of poor
design, over design – too many functions without
much use, poor training, or simply ignorance. It
StrongandMeaningfulUseofHealthcareInformationSystems(HIS)
383

includes aspects of the HIS which could be used to
improve the outcomes and aren’t. Non-use too can
coexist with meaningful and meaningless use.
Last, but not the least (a cliché, but very
appropriate here), while there is a lot of attention
given to healthcare fraud using HIS such as
upcoding, illegal billing, etc. they have not been
grouped together as mis-use of HIS. There are lesser
forms of misuse too which can affect outcomes such
as cutting and pasting medical notes propagating
past errors, careless checking of boxes, etc.
The Use dimension in the ontology
conceptualizes the four types of use as part of a
continuum. They are independent and can coexist –
one is not defined as a negation or by the absence of
another. The categories are can be considered to be
complete. If necessary, the dimension can be
modified by adding categories or refining existing
ones with subcategories.
2.3 Stakeholder
The stakeholders are the users of the HIS. The seven
broad categories of stakeholders in the ontology are
the Recipients of, the Providers of, the Payers for,
the Employers (of recipients) of, the Insurers of, the
Regulators of healthcare, and the Government. The
recipients of healthcare may be individual Patients,
patient Families, or a Population. These are shown
as subcategories of Recipients in the ontology.
Similarly, the subcategories of Providers are
Physicians, Nurses, and Pharmacists. The
Stakeholder dimension can be extended by adding
more categories, reduced by eliminating categories,
refined by adding subcategories, coarsened by
combining categories or subcategories. Through
these operations the use of HIS can be studied at
different levels of granularity. The categories, as
shown, are nominal – they may be reordered without
loss of information. They may also be ordered based
on, for example, their importance or sequence in the
process of healthcare delivery.
The use of HIS by stakeholders can vary
significantly and so could their desired outcomes.
While the Payer may consider the use of HIS for
managing costs of healthcare as being Meaningful,
the Provider may see it as Mis-use. The variations in
the perceptions of the different types of Use and the
priorities of the different Outcomes have to be part
of the Science, Practice, and Policy of use of HIS.
There is a considerable amount of interaction
between the stakeholders using the HIS and also
because of it. The Providers and the Recipients may
see the lab results simultaneously using the HIS,
which may lead to better care. On the other hand an
insurer may mine the data on a Provider’s care
history and question his or her practices, resulting in
conflict and tension. These interactions can be
mapped by crossing the categories of Stakeholders
in a two-dimensional table, and have to be
considered in the development of the Science,
Practice, and Policy. Higher order dimensions are
more complex. They exist and can be mapped with
higher order tables. The taxonomy of stakeholders
can be used to develop a cognitive map of the
interaction among them. It must be noted that the
interactions can be two-way and not just one-way,
and multi-way in the case of higher order
interactions. The identification and recognition of
this symmetry will be central to the development of
a strong science, practice, and policy of use off HIS.
2.4 Outcome
Cost, Quality, Safety, and Parity of healthcare are
the four outcomes specified in the CMS Stages 1 and
2 criteria (Centers for Medicare & Medicaid
Services). They are more or less universal. We have
subcategorized Cost as Financial and Non-financial,
and the other three as Measured and Perceived. The
dichotomous distinctions are important – their
information bases are different and they are not
perfectly correlated. Perceived quality, for example,
may be at variance with measured quality.
The order of the outcomes listing reflects the
general emphasis in the CMS criteria; however, the
order may vary by stakeholder or be changed. As
with other dimensions the granularity of Outcomes
can be changed by varying the categories and
subcategories.
There can be a considerable amount of
interaction between the outcomes. For example,
improvements in Quality may affect the Cost;
improvements in Safety may decrease the Cost; and
improvements in Quality may improve Safety. These
and higher order interactions too can be mapped by
crossing the Outcome categories in a two-or higher-
dimensional table. As with stakeholders the
taxonomy of outcomes can be used to develop a
cognitive map of the interactions among them. And
these interactions too can be one-way, two-way, or
multi-way.
3 COMPONENTS OF USE OF HIS
The components of use of HIS can be enumerated by
concatenating natural English sentences from the
HEALTHINF2014-InternationalConferenceonHealthInformatics
384

four dimensions (columns) and the interleaved
words/phrases between the columns as illustrated at
the bottom of Figure 1. They are:
1. Science of meaningful use of HIS by recipients
to manage cost of healthcare. For example, use
of the internet by patients and their families to
compare the cost of surgery in different facilities.
2. Practice of non-use of HIS by providers to
manage quality of healthcare. For example,
override of drug-drug interaction alerts by
physicians.
3. Policy of meaningless use of HIS by regulators
to manage parity of healthcare. For example, use
of poor public health data on parity of healthcare
for regulating diet in school meals.
The ontology encapsulates 336 (3*4*7*4) first-
level components and 1,056 (3*4*11*8) second-
level components of use of HIS. The ontology
provides a convenient way of studying them without
enumerating them – the latter would run into many
pages.
Looked at differently, the ontology is a complete,
closed description of the problem of use of HIS. It is
a visualization of the problem space of science,
practice, and policy of HIS. We underscore the
indefinite article ‘a’ to indicate the possibility of
other formulations as well as refinements and
extensions of the present formulation. New
dimensions can be added or current dimensions
reduced. New categories and subcategories can be
added or current ones collapsed or removed. By
manipulating the ontology in these ways one can
obtain different perspectives on the problem at
different levels of granularity.
It must be noted that addition/reduction of
dimensions/categories changes the number of
components combinatorially. Thus, the additions can
dramatically increase the complexity at the cost of
parsimony. The two opposing forces have to be
balanced for an effective study of the science,
practice, and policy of the use of HIS. Our objective
is to make parts of the problem and the whole
problem visible parsimoniously – on less than a
single page.
Ideally, a systematic, systemic, and symmetric
study of the science, practice, and policy of use of
HIS should consider all the components. Some of
the components may be instantiated as in the
illustrations above. When they are instantiated
frequently we can call them the ‘bright’ spots; when
instantiated infrequently we can call them the ‘light’
spots. There are likely many ‘bright’ spots regarding
meaningful use and ‘light’ spots regarding non-use.
Some components may not be instantiated at all. The
absence of instantiation may be because the
component has been overlooked or it is infeasible.
We will call the overlooked components the ‘blind’
spots, and the infeasible components the ‘blank’
spots. It is difficult to determine a priori whether an
absent component is a ‘blind’ or a ‘blank’ spot.
There are likely many ‘blind/blank’ spots regarding
meaningless use.
The extant literature – scientific, practice, and
policy – on the use of HIS can be exhaustively
mapped to the ontology using qualitative analysis
tools like consensus coding and NVivo. Some
articles may cover multiple components of the
ontology, some multiple snippets (parts of a
component), and some may cover a few components
or snippets. Some articles may not map to the
ontology at all which may suggest the need to
modify the ontology to accommodate overlooked
elements of the problem.
Such a mapping will highlight the ‘bright’,
‘light’, and ‘blind/blank’ spots in the science,
practice, and policy of use of HIS. These maps can
be analyzed to determine the gaps (a) within the
science, practice, and policy, and (b) between the
science, practice, and policy of use of HIS. The
former are discipline gaps and the latter translation
gaps. An analysis of the antecedents and
consequences of these gaps will help develop a
roadmap for science, practice, and policy for HIS.
In the conclusion we will describe how mapping
the ‘bright’, ‘light’, and ‘blind/blank’ spots in the
literature using the ontology can be used to develop
a roadmap for science, practice, and policy of HIS.
4 CONCLUSION: ROADMAP
FOR STRONG AND
MEANIGFUL USE OF HIS
The roadmap for a strong science, practice, and
policy of HIS cannot be asymmetric – it cannot have
only left turns or right turns; it cannot focus only on
meaningful use and not consider meaningless, non-,
and mis-use. One way to improve the roadmap is to
bridge the gaps between the ideal (as portrayed by
the ontology) and the real (as portrayed by the
bright, light, blind/blank spots).
A ‘bright’ spot in a domain may be the
consequence of the priority set by the funding
agency or the gatekeepers of the domain. On the
other hand, it could also be the consequence of a
‘herd’ effect – it is easier to obtain grants and
StrongandMeaningfulUseofHealthcareInformationSystems(HIS)
385

publish ‘more of the same’. If the former, the
brightness of the spot may be functional and the
emphasis should be maintained; if the latter, it may
be dysfunctional and emphasis should be changed. A
‘light’ spot may indicate its lack of importance or
that it is an emergent focus. Last, a ‘blank’ spot may
be unimportant or important but overlooked. If
unimportant it may need to be so; if important the
emphasis needs to be changed.
A ‘bright’ spot in science and a corresponding
‘blank/blind’ spot in practice may indicate the need
for translation or the practical irrelevance of the
research. By the same token, a ‘blank/blind’ spot in
science and a corresponding ‘bright’ spot in practice
may indicate misplaced practice or a practice which
needs to be researched.
Thus through an analysis of the antecedents and
consequences of the gaps within the domains of
science, practice, and policy and between them using
the ontology one can construct a better roadmap for
use of HIS. While we have focused the discussion in
this paper broadly on the use of HIS, the method can
be used to develop better roadmaps in specific areas
of healthcare where information systems play a
critical role – for example, long-term breast cancer
care, care for chronic illnesses, and tele-healthcare.
We believe a systematic, systemic, and symmetric
approach to these problems should be the standard.
REFERENCES
Blumenthal, D. 2009. Stimulating the adoption of health
information technology. New England Journal of
Medicine, 360, 1477-1479.
Callen, J. L., Westbrook, J. I., Georgiou, A. & Li, J. 2011.
Failure to Follow-Up Test Results for Ambulatory
Patients: A Systematic Review. Journal of General
Internal Medicine, 27, 1334-1348.
Centers for Medicare & Medicaid Services. Meaningful
Use (Online). Available: https://www.cms.gov/
Regulations-and-
Guidance/Legislation/EHRIncentivePrograms/Meanin
gful_Use.html.
Classen, D. C., Phansalkar, S. & Bates, D. W. 2011.
Critical drug-drug interactions for use in electronic
health records systems with computerized physician
order entry: review of leading approaches. Journal of
Patient Safety, 7, 61-65.
Crosson, J. C., Schueth, A. J., Isaacson, N. & Bell, D. S.
2012. Early adopters of electronic prescribing struggle
to make meaningful use of formulary checks and
medication history documentation. The Journal of the
American Board of Family Medicine, 25, 24-32.
Gaikwad, R., Sketris, I., Shepherd, M. & Duffy, J. 2007.
Evaluation of accuracy of drug interaction alerts
triggered by two electronic medical record systems in
primary healthcare. Health informatics journal, 13,
163-177.
Interagency Breast Cancer and Environmental Research
Coordinating Committee 2013. Breast Cancer and the
Environment: Prioritizing Prevention.
http://www.niehs.nih.gov/about/assets/docs/ibcercc_fu
ll.pdf.
Phansalkar, S., Desai, A. A., Bell, D., Yoshida, E., Doole,
J., Czochanski, M., Middleton, B. & Bates, D. W.
2012a. High-priority drug–drug interactions for use in
electronic health records. Journal of the American
Medical Informatics Association, 19, 735-743.
Phansalkar, S., van der Sijs, H., Tucker, A. D., Desai, A.
A., Bell, D. S., Teich, J. M., Middleton, B. & Bates, D.
W. 2012b. Drug–drug interactions that should be non-
interruptive in order to reduce alert fatigue in
electronic health records. Journal of the American
Medical Informatics Association.
Platt, J. R. 1964. Strong inference. Science, 146, 347-353.
Rahmner, P. B., Eiermann, B., Korkmaz, S., Gustafsson,
L. L., Gruvén, M., Maxwell, S., Eichle, H.-G. & Vég,
A. 2012. Physicians' reported needs of drug
information at point of care in Sweden. British Journal
of Clinical Pharmacology, 73, 115-125.
Ramaprasad, A. & Thirumalai, M. 2012. Managing
Population Health: An Ontological Framework
(Poster). 2012 Summit on the Science of Eliminating
Health Disparities. Washington DC, USA.
Seidling, H. M., Phansalkar, S., Seger, D. L., Paterno, M.
D., Shaykevich, S., Haefeli, W. E. & Bates, D. W.
2011. Factors influencing alert acceptance: a novel
approach for predicting the success of clinical decision
support. Journal of the American Medical Informatics
Association, 18, 479-484.
Smithburger, P. L., Buckley, M. S., Bejian, S.,
Burenheide, K. & Kane-Gill, S. L. 2011. A critical
evaluation of clinical decision support for the
detection of drug-drug interactions. Expert Opinion on
Drug Safety, 10, 871-882.
Spina, J. R., Glassman, P. A., Simon, B., Lanto, A., Lee,
M., Cunningham, F. & Good, C. B. 2011. Potential
Safety Gaps in Order Entry and Automated Drug
Alerts: A Nationwide Survey of VA Physician Self-
Reported Practices With Computerized Order Entry.
Medical Care, 49, 904-910.
Takarabe, M., Shigemizu, D., Kotera, M., Goto, S. &
Kanehisa, M. 2011. Network-Based Analysis and
Characterization of Adverse Drug–Drug Interactions.
Journal of chemical information and modeling, 51,
2977-2985.
HEALTHINF2014-InternationalConferenceonHealthInformatics
386
