
Modelling Domain Knowledge of Speech and Language Therapy with
an OWL Ontology and OpenEHR Archetypes
Vladimir Robles-Bykbaev
1,2
, Martín López-Nores
2
, José Pazos-Arias
2
, Jorge García-Duque
2
and Juan Ochoa-Zambrano
1
1
GI-IATa, CIDII, Universidad Politécnica Salesiana, Calle Vieja 12-30, Cuenca, Ecuador
2
AtlantTIC Research Center for Information and Communication Technologies, Department of Telematics Engineering,
University of Vigo, Vigo, Spain
Keywords: Health Informatics, Speech and Language Therapy, Ontology, Archetypes.
Abstract: Researchers in the area of health informatics have made significant progress in the standardization of ICT
tools to support the management, storage, retrieval and exchange of health-related data. However, the
adoption of these advances is largely uneven across different areas. We present a comprehensive knowledge
model for the realm of Speech and Language Therapy (SLT), based on an OWL ontology, normalized
vocabularies and OpenEHR constructs. This model, validated by several collaborating institutions, is being
used as the cornerstone to build a comprehensive framework with supporting tools for the different people
involved in SLT, including therapists, patients and their relatives, and students.
1 INTRODUCTION
With estimations of nearly one billion people in the
world living with some form a disability, adequate
access to healthcare and rehabilitation services has
become a major issue in global politics (WHO,
2011). The area of speech and language disorders is
a small and often overlooked part of this picture,
even though the development of proper
communication skills is an important mainstay in a
person’s life, given that it allows him/her to express
his/her feelings, needs and opinions as an active
member of society. Nowadays there are no reliable
and representative statistics of people suffering from
communication disorders in the world, but the
existing data show a complex outlook, due to the
number of people affected (e.g. around 15 million
people suffer from stutter in the world, whereas
about 6 millions in the United States have other
language impairments) and the lack of systematic
approaches to develop and provide services of
Speech and Language Therapy (SLT) (WHO, 2011;
NIDCD, 2014).
SLT is a complex discipline that relates to many
aspects of the patients’ health condition, social
environment and cognitive development.
Accordingly, there are many people involved in the
SLT processes (patients and their relatives, doctors,
teachers, speech and language pathologists, …) and
the flows of information (among homes, hospitals,
schools, clinics, …) are very complex. On these
grounds, it is important to develop a knowledge
model of the SLT domain using standardized formal
artifacts, in order to facilitate the exchange of
information and thus foster the creation of
convenient ICT tools, with which to support the
initial speech-language diagnosis, the design of
personalized therapy plans, the treatment of the wide
spectrum of disorders, the monitoring of the
patients’ progress from the different points of view,
and many other activities.
Most of research conducted hitherto in ICTs
applied to the SLT area have focused on developing
expert systems to support diagnosis and treatments
of specific disorders, like dysphagia (Sharma et al.,
2013), dysarthria and dyslalia (Schipor et al., 2012)
or swallowing difficulties (Ward, Burns, Theodoros
and Russell, 2014). These works did not pay any
attention to the issues of sharing, maintaining and
porting the clinical data over different platforms;
rather, they relied on ad hoc languages, data
structures and procedures. Only a few recent studies
have used conceptualizations and classifications ––
in the form of an ontology–– to support the
operation of an expert system aimed at the initial
585
Robles-Bykbaev V., Pazos-Arias J., López-Nores M., García-Duque J. and Ochoa-Zambrano J..
Modelling Domain Knowledge of Speech and Language Therapy with an OWL Ontology and OpenEHR Archetypes .
DOI: 10.5220/0005279405850591
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 585-591
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

diagnosis of language disorders (Martín Ruiz et al.,
2014) but, to the best of our knowledge, there have
been no approaches to support SLT within a fully
integrative framework for clinicians and students,
pathologists, patients, relatives and other potential
users. In response to that, we hereby present a
knowledge model for SLT that provides the
foundations to build a comprehensive set of
supporting tools for the following activities, among
others:
Accessing, sharing and querying the information
according to specialized taxonomies of SLT
concepts and user types.
Automating statistical procedures to analyse the
patients' evolution, the effectiveness of the
applied therapies, common SLT patterns,
behavioural patterns, etc.
Automating the adaptation of contents to put in
therapy plans or learning courses, according to
SLT taxonomies and patient/student profiles.
Integrating assistive technologies to provide
support during the therapy sessions: robot
assistants, mobile applications, remote software-
monitoring, etc.
Developing inference mechanisms for
recommender and decision-support systems to
assist in the preparation of therapy plans, the
evaluation of exercise results, the generation of
case studies, etc.
Porting the data-structures through different
architectures and systems.
Our knowledge model, preliminarily validated by
SLPs from several collaborating institutions of
speech and language therapy of Azuay - Ecuador, is
based on an ontology that integrates concepts from
standardized vocabularies from the American
Speech-Language-Hearing Association (ASHA,
2014) and constructs from OpenEHR, an
international standard to model healthcare
information (www.openehr.org). Ontologies have
been previously used in the e-health domain to
model clinical data repositories (Rubi et al., 2014),
whereas our research contribution has to do with
using an ontology as an enabling tool for a set of
ICT-based healthcare services in a very specific
area.
The paper is organized as follows. The core ideas
relating to the construction of the ontology are
presented in Section 2, whereas Section 3 provides
details about the methodology followed to populate
it with instances of disorders, case studies, diagnosis
information, exercises, etc. Section 4 contains an
overview of a group of ICT tools we are developing
on top of the knowledge model to support different
aspects of SLT, including an expert system to
automate the generation of therapy plans, a
web/mobile portal to deliver training courses to
students of phonoaudiology and a robotic assistant to
support SLT sessions.
2 AN ONTOLOGY FOR SLT
Next, we will describe the main structures and
elements of our proposed model. In the same way,
we present two main diagrams to facilitate the
comprehension of the model developed and how it is
integrated in the research context for a
comprehensive solution supporting SLT.
In order to provide a formal representation of the
main health care concepts related with SLT and
obtain the domain knowledge contained in the
ontology, a team of engineers, SLPs and doctors of
several collaborating institutions of special
education have selected some of the most
representative disorders, speech-language areas, and
therapy-evaluation strategies. These were:
- Disorders (according to the classification
provided in ASHA, 2014): dysarthria, expressive
language disorder, dysphasia, dysphonia, speech
and language developmental delay due to hearing
loss, problems with swallowing and mastication,
fluency disorder, moderate intellectual
disabilities, severe intellectual disabilities,
profound intellectual disabilities, infantile
cerebral palsy (with the aim to offer SLT to
children), and epilepsy and recurrent seizures.
- Language and speech areas: expressive
language, articulation, receptive language, oral
structure and function, hearing, and linguistic
formulation.
- Therapy strategies: the ontology allows
establishing several semantic relations between
the therapy, educational contents, rehabilitation
concepts, the patient's profile and the SL skills.
Thereby, a speech-language skill must be able to
adapt to patient's profile with which is related.
For example, for a patient that suffers from
cerebral palsy and severe athetosis and cannot
produce speech, the SL skill representing
communication through voice must
automatically change to represent an alternative
communication way (signs, gestures, etc.).
Likewise, a given therapy plan could contain or
not all SL areas before mentioned, under that a
patient can only suffer a functional dyslalia and
HEALTHINF2015-InternationalConferenceonHealthInformatics
586
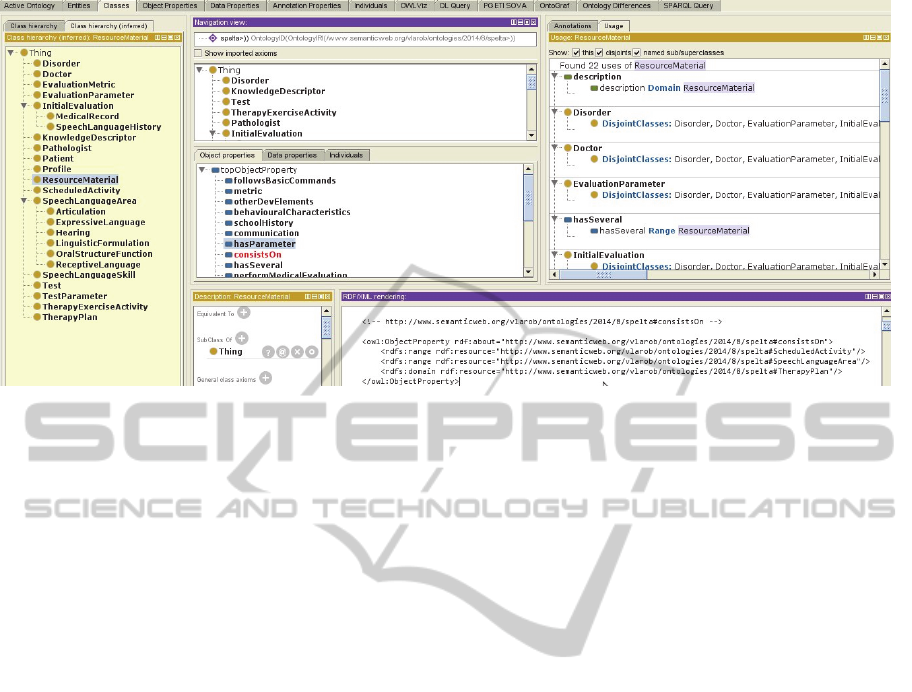
Figure 1: A tool snapshot showing some of the main elements and relations of the proposed ontology.
solely needs to do articulation reinforcement
activities.
In Figure 1 we can see a screen capture of the
class view menu in Protege (Riaño et al., 2012),
depicting the hierarchy of classes, some of the object
properties defined, some relations between
ResourceMaterial and other classes, and the RDF
(Resource Description Framework) source.
Figure 2 depicts a summarized view of the static
structure (class diagram) of the knowledge model to
support the SLT. The presented elements show the
generalization and associations concepts as well as
some of the main attributes of some classes. The key
concepts, relations and information structures are as
follows:
- Initial patient evaluation. In order to determine
the best alternative to design a general therapy
plan (the general guidelines to conduct therapy
and stimulation exercises and activities), it is
necessary to conduct an initial patient diagnostic.
This diagnostic allows to determine the general
medical condition (suffered diseases, serious
surgeries or injuries, prescribed medications, …),
initial condition, development history (i.e. data
about fundamental aspects of the patient's
childhood, such as the age at which he/she was
able to sit up or walk) and basic skills of speech
and language (communication skills, behavioural
characteristics, hearing condition and school
record). The initial patient evaluation is
represented by MedicalRecord and
SpeechLanguageHistory classes, and is
conducted by doctors and speech-language
pathologists (Doctor and Pathologist classes).
- Patient’s Profile. A patient’s profile is
characterized by the initial evaluation, his/her
personal data (name, date of birth, genre, ethnic
group, etc.) and his/her speech-language
screening (cognitive age, receptive language age,
expressive language age, education level and
suffered disorders). In order to prepare the
patient's profile, it is necessary to evaluate
him/her using special tests that belong to specific
areas of Speech and Language (SL). The tests are
represented by Test class and consist of several
evaluation parameters (EvaluationParameter)
that can represent a test question, a SL screening
concept or a medical evaluation/screening
parameter. Likewise, each test is related
semantically with the disorders (class Disorder)
that it helps to diagnose.
- Therapy. With the aim of developing a therapy
plan, the SLPs must know the patient's skills in
the several areas (SL, physical and cognitive).
The SL skills are represented by
SpeechLanguageSkill class and are characterized
by the area to which they belong
(SpeechLanguageArea). Similarly, an SL skill
has several attributes that describe the knowledge
to learn in the school context or in the language
pillars (knowledge area, name, cognitive level,
skill's description, etc.). With the goal to help
patients to develop certain skills, a SLP needs to
conduct several therapy exercises and activities.
These exercises are represented by the
TherapyActivityExercise class, have attributes
that describe how to be performed (duration,
repetitions, complexity, etc.), and consist of
several material or resources (class
ResourceMaterial).
ModellingDomainKnowledgeofSpeechandLanguageTherapywithanOWLOntologyandOpenEHRArchetypes
587

Figure 2: Partial view of the class diagram of the developed knowledge base (the monitoring concept is not shown).
- Monitoring (not shown in figures). Given that an
SL evaluation is commonly conducted three
times during the therapy period (at beginning, in
the middle and at end), we propose to store the
results of each of these evaluations, with the aim
of enabling data mining activities and statistical
analysis.
3 POPULATING THE
ONTOLOGY WITH INSTANCES
OF OPENEHR ARCHETYPES
The ability to use clinical concepts supported by
standardized vocabularies and international medical
guidelines, just like the ability to share and port the
clinical information (semantic interoperability), is
one of the most important features needed to support
information systems for the healthcare area,
regardless of nature and final objective (expert
system, decision support system, data mining, ...). In
this line, clinical archetypes appear as formal
definitions of specific clinical concepts, defined as
specializations of a generic reference model, that
provide a mechanism to express data structures in a
shared and interoperable way (Lezcano et al., 2011).
The OpenEHR specifications proposed using clinical
archetypes to represent and manage information, in
ways that have been proven to achieve good results
in several healthcare areas like inter-institutional
health data integration (Vieira-Marques et al., 2014),
primary care attention in public institutions
(Bacelar-Silva et al., 2013) and the development of
health information systems (Kallel et al., 2011). On
these grounds, we propose to use archetypes to
represent the SLT formal definitions using
vocabularies standardized by American Speech-
Language-Hearing Association (ASHA, 2014). With
the proposed model we can use ontologies to
describe all SLT concepts using different levels of
granularity, while the archetypes allow us to specify
the information that should be captured in order to
conduct each stage of SLT.
Figure 3 depicts an example of the main
archetype (type composite), that has the following
slots (sections): medical baseline screening, speech
and language screening, therapy plan, and patient's
profile.
Each one of these sections is defined in a
separate archetype; for example, the speech and
language screening section has several entries
(evaluation date, additional comments, ...),
HEALTHINF2015-InternationalConferenceonHealthInformatics
588
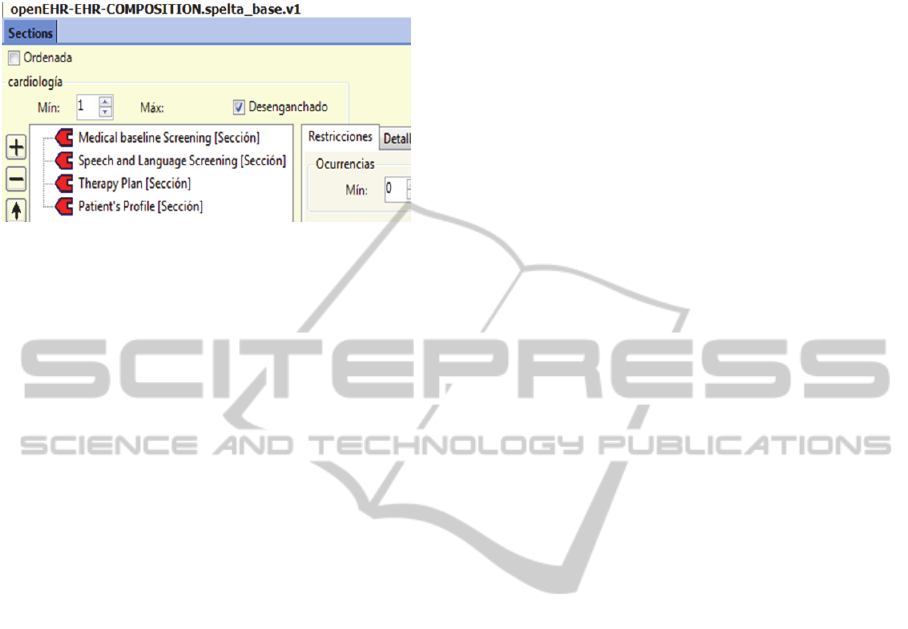
evaluation entries (if patient is able to follow basic
commands, ...), and so on.
Figure 3: Screen capture of the main archetype
(composition) of the proposed knowledge model.
4 RESEARCH CONTEXT FOR
THE SLT KNOWLEDGE
MODEL
With the aim of evaluating the proposed model, we
have collected 130 real cases of children suffering
from different kinds of speech-language disorders.
Each of these cases was evaluated by doctors and
SLPs from collaborating institutions. Likewise, all
cases were collected using an online information
system and contain the information structures
mentioned in Section 2. Using this information, we
are performing a stage to verify the consistency of
the model.
Furthermore, we are developing several ICT
tools to support different aspects of SLT, including
an expert system to automate the generation of
therapy plans, a web/mobile portal to deliver
training courses to students of phonoaudiology and a
robotic assistant to support SLT sessions. This
environment of SLT backing tools consists in the
following elements (Figure 4):
- Database Layer. All the information represented
in the knowledge model is stored in the database.
Given that our ICTs tools include a mobile
version of the support system for SLT, the
information collected using mobile devices is
previously stored in his own local base and then
will be synchronized with the server database.
- Knowledge Model. This layer contains the
ontologies, the archetypes and the standardized
vocabulary aforementioned.
- Expert System Layer. The expert system is able
to automatically infer speech-language therapy
plans, using those plans manually developed by
SLPs. In order to infer a new plan, the system
uses the patient's profile information, the results
obtained in the screening tests, and the patient's
skills/weakness in the speech-language areas
mentioned in the section 2. Moreover, the
content generation is a process that produces new
exercises and therapy activities for patients that
suffer slight or moderate speech-language
disorders.
- User Interface Layer. In this layer are provided
software and hardware tools to support the different
activities conducted by SLPs or students. The
mobile application contains the screening tests to
help to reduce time during the SL patient's
evaluation. Likewise, it is able to query the
information contained in the server database
(patient's profile, previous evaluation results,
progress reports, ...). The web training system for
students is focused in learning activities for future
SLPs: asking to develop therapy plans, analysing
cases (according to given disorders and language
skills), and others. The desktop application has the
same functionalities of the mobile version, and is
intended for providing portability. The robotic
therapy and monitoring assistant consists of two
elements: a mobile device (smartphone or tablet) and
a displacement electronic platform. In the mobile
device is presented an avatar that interacts with
patients (especially children), and is able to tell
stories, detect some hand gestures (if the user wears
a glove of certain color), receive voice orders, and
has a remote console to be controlled in “manual
mode” by the SLPs. The platform allows robot to
move in the floor using two servomotors.
The Figure 4 presents 3 elements: in the left side
(a) is shown a screen capture of the desktop version
to support SLT where are depicted the patient's
progress in the 5 speech-language therapy areas (the
expressive language and articulation are presented
together). In the centre (b) of the figure we can see
an interaction between the robot and children
suffering from different speech and language
disorders. The robot is telling a story with the aim to
relax the children, as previous activity to start the
therapy. In the right side of the figure (c) is shown a
photo of the robot, where is possible to see the
avatar displayed in the mobile device screen as well
as the displacement platform.
5 CONCLUSIONS
The proposed approach presents an innovative
model that relies on ontologies, archetypes and
standardized vocabularies, and provides an
integrative environment able to include new therapy
ModellingDomainKnowledgeofSpeechandLanguageTherapywithanOWLOntologyandOpenEHRArchetypes
589

Figure 4: Screen capture of some applications belonging to user’s layer.
reinforcement pedagogical elements, applications for
monitoring and educational software (robotic
assistant, mobile versions of the application,
educational web-based system, ....). In the same
way, this model supports the semantic portability
and is capable to support data mining processes and
intelligent content generation (automatic SLT plans
generation). Moreover, the researches carried out are
focused on finding/providing solutions to treatment
of some specific disorders, initial screening of
disorders or the use of ontologies to sustain more
elaborated processes in the initial SL diagnosis.
As future work in the speech-language therapy
domain-modelling, we are starting to extend our
model with the aim of covering some deeper areas of
knowledge, like the automatic generation of specific
therapy plans based on daily activities and
considering these elements: the existing levels of
granularity of the patient's cognitive development,
the incidence of other disorders (cerebral palsy,
athetosis ...), etc.
ACKNOWLEDGEMENTS
The authors from the University of Vigo have been
supported by the European Regional Development
Fund (ERDF) and Xunta de Galicia under project
CN 2012/260 “Consolidation of Research Units:
AtlantTIC”, and by the Ministerio de Educación y
Ciencia (Gobierno de España) research project
TIN2013-42774-R (partly financed with FEDER
funds). We would like to thank the support provided
by María Augusta Zambrano and the "Jesús para los
Niños" foundation of Cañar, Ecuador.
REFERENCES
American Speech-Language-Hearing Association
(ASHA), 2014. International Classification of
Diseases, Tenth Revision - Clinical Modification,
Related to Speech, Language, and Swallowing
Disorders. (ICD_10_CM).
Bacelar-Silva, G. M., Cesar, H., Braga, P., and Guimaraes,
R., 2013. OpenEHR-based pervasive health
information system for primary care: First Brazilian
Experience for Public Care. In Computer-Based
Medical Systems (CBMS), 2013 IEEE 26th
International Symposium on, pp. 572-873. IEEE.
Kallel, F., Ellouze, A. S., and Bouaziz, R., 2011.
Generating Context-Awarness Interface for Medical
Applications. In Developments in E-systems
Engineering (DeSE), 2011, pp. 105-110. IEEE.
Lezcano, L., Sicilia, M. A., and Rodríguez-Solano, C.,
2011. Integrating reasoning and clinical archetypes
using OWL ontologies and SWRL rules. In Journal of
biomedical informatics, vol. 44, no. 2, pp. 343-353.
Martín Ruiz, M. L., Valero Duboy, M. Á., Torcal
Loriente, C., and Pau de la Cruz, I., 2014. Evaluating a
Web-Based Clinical Decision Support System for
Language Disorders Screening in a Nursery School. In
Journal of medical Internet research, vol. 16.
National Institute of Deafness and Other Communication
Disorders (NIDCD), 2014. Statistics on Voice, Speech
and Language.
Riaño, David, and et al., 2012. An ontology-based
personalization of health-care knowledge to support
clinical decisions for chronically ill patients. In
Journal of biomedical informatics, vol. 45, no 3.
Rubi, R., Pastor, X. and Lozano, E., 2014. OWLing
Clinical Data Repositories With the Ontology Web
Language. In JMIR Medical Informatics, vol. 2, no 2.
Sharma, S., Ward, E. C., Burns, C., Theodoros, D., and
Russell, T., 2013. Assessing dysphagia via
telerehabilitation: Patient perceptions and satisfaction.
In International journal of speech-language
pathology, vol. 15, pp. 176-183.
Schipor, O. A., Pentiuc, S. G. and Schipor, M. D., 2012.
HEALTHINF2015-InternationalConferenceonHealthInformatics
590

Automatic Assessment of Pronunciation Quality of
Children within Assisted Speech Therapy. In
Electronics & Electrical Engineering, pp. 15-18.
Vieira-Marques, P., Patriarca-Almeida, J., Frade, S.,
Bacelar-Silva, G., Robles, S., and Cruz-Correia, R.,
2014. OpenEHR aware multi agent system for inter-
institutional health data integration. In Information
Systems and Technologies (CISTI), 2014 9th Iberian
Conference on, pp. 1-6. IEEE.
Ward, E. C., Burns, C. L., Theodoros, D. G., and Russell,
T. G., 2014. Impact of dysphagia severity on clinical
decision making via telerehabilitation. In Telemedicine
and e-Health.
World Health Organization (WHO) and World Bank,
2011. World Report on Disability, Malta: WHO Press.
ModellingDomainKnowledgeofSpeechandLanguageTherapywithanOWLOntologyandOpenEHRArchetypes
591
