
Patient Empowerment as a Cognitive Process
Eleni Kaldoudi
1
and Nikos Makris
2
1
School of Medicine, Democritus University of Thrace, Dragana, Alexandroupoli, Greece
2
School of Educational Sciences, N. Chili, Alexandroupoli, Greece
Keywords: Patient Empowerment, Cognitive Process, Empowerment Model, Awareness, Engagement, Control.
Abstract: The concept of patient empowerment has emerged as a new paradigm that can help improve medical
outcomes while lowering costs of treatment by facilitating self-directed behavior change. Patient
empowerment has gained even more popularity since the 1990’s, due to the emergent of eHealth and its
focus on putting the patient in the centre of the interest. Current literature provides systematic reviews of the
area, and shows that well defined areas (or dimensions) have eventually emerged in the field. In this paper
we argue that patient empowerment should be treated formally as a cognitive process. We thus propose a
cognitive model that consists of three major levels of increasing complexity and importance: awareness,
engagement and control. We also describe the different constituents of each level and their implications for
patient empowerment interventions, focusing on interventions based on information and communication
technologies. Finally, we discuss the implications of this model for the design and evaluation of patient
empowerment interventions.
1 INTRODUCTION
Patient empowerment has emerged as a new
paradigm to improve medical outcomes through
self-directed behavior change. Conceptually,
‘empowerment’ relates to (a) the goal of individuals
to have control over their quality of life, and (b) the
process via which individuals can achieve this goal.
Patient empowerment seems particularly promising
in the management of chronic diseases
(Chatzimarkakis, 2010; Anderson and Funnel, 2010)
and is directly connected with personalized patient
services, education and preventive measures. The
research community accepts that better health
outcomes can be achieved by improving a person's
ability to understand and manage his or her own
health and disease, negotiate with different teams of
health professionals, and navigate the complexities
of health systems (The Lancet, 2012).
Empowerment appears in many different
contexts, always as a cognitive process – that of
enhancing the capacity of individuals or groups to
make choices and to transform those choices into
desired actions and outcomes. For example, human
resource management research recognizes
empowerment as a cognitive process; studies therein
investigate interventions that are designed,
developed and assessed following a cognitive model
of the empowerment process (Robbins et al, 2002;
Thomas and Velthouse, 1990).
In this paper we argue that patient empowerment
should be treated as a cognitive process. We also
propose a cognitive model and we describe its
different constituents and their implications for the
design and evaluation of patient empowerment ICT
(i.e. information and communication technology)
interventions. Finally, we discuss future work to
deploy and validate the proposed model.
2 PATIENT EMPOWERMENT
Julian Rappaport (Rappaport, 1987) defined
empowerment as “a process, a mechanism by which
people, organizations, and communities gain
mastery over their affairs”. Empowerment, in its
most general sense, refers to the ability of humans to
gain understanding and control over personal, social,
economic and political forces in order to take action
to improve their life (Israel et al, 1994). In health
science, patient empowerment is understood as an
enabling process or outcome (Freire, 1993;
McAllister et al, 2012) by which patients are
encouraged to autonomous self-regulation, self-
605
Kaldoudi E. and Makris N..
Patient Empowerment as a Cognitive Process.
DOI: 10.5220/0005281906050610
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 605-610
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

management and self-efficacy in order to achieve
maximum health and wellness (Lau, 2002).
Empowerment can therefore be described as a
process where the purpose of an educational
intervention is to increase patients’ ability to think
critically and act autonomously; while it can also be
viewed as an outcome when an enhanced sense of
self-efficacy occurs as a result of the process
(Anderson and Funnell, 2010).
The concept of patient empowerment has
emerged in 1970s in USA and UK as part of the rise
of New Right politics (Traynor, 2003). The concept
eventually evolved as a new paradigm that can help
improve medical outcomes while lowering costs of
treatment by facilitating self-directed behavior
change. The concept seems particularly promising in
the management of chronic diseases
(Chatzimarkakis, 2010; Anderson and Funnel, 2010)
and it is directly connected with personalized patient
services, education and preventive measures. Patient
empowerment has gained even more popularity
since the 1990’s, due to the emergent of eHealth and
its focus on putting the patient in the centre of the
interest. A recent review (Ajoulat et al, 2007) shows
that patient empowerment services mainly aim at
educational programs seeking patient reinforcement.
Indeed, patient education interventions seem to have
taken the lead in the early attempts to strengthen
patients. To illustrate this we have searched PubMed
database for the term ‘patient education’. Figure 1
shows the results (red line), as a plot of number of
papers per year for the last five decades. According
to this graph, published works on “patient
education” first started to appear during the 1960s,
following an increasing curve from the mid-70s until
2006, when their yearly numbers started to decline.
At the same time, research interest begun to focus on
the related concepts of ‘patient engagement’ and
‘patient empowerment’. PubMed searches with these
terms (also plotted in Figure 1, with green and blue
lines respectively) indicate an increasing research
interest, especially during the last decade.
Reviews of the field reveal three basic
dimensions of patient empowerment: education,
engagement, and control (Ouschan et al, 2000,
Unver and Atzori, 2013). Patient education is
perceived as a set of planned educational activities
designed to improve patient health behavior and
health status. Its main purpose is to maintain or to
improve patient health as well as to train the patient
to become able to actively participate in his or her
own healthcare treatment by increasing self-efficacy
(Bandura, 1977). Patient engagement involves two
different concepts: cooperation with health providers
and an active engagement in managing one’s own
health status and disease. The control dimension
refers to the patient’s ability to actively participate in
strategic decisions about his or her health and
disease management.
Although there is a clear distinction between
these three dimensions, often empowerment
interventions include all three dimensions in their
goal and, eventually, in their design. This has
obvious implications for the methodology and tools
that will be used to evaluate the specific
intervention. For example, evaluation of patient
education interventions should examine expected
outcomes such as: understanding health information;
ability to recognize new or warming signs or
symptoms of disease progression and transition; and
self-satisfaction of being well-informed on the
treatment options of his or her condition or disease.
The evaluation of interventions targeting patient
participation should exam different outcomes such
as: the degree of patients’ involvement in treatment
plans; lifestyle and behaviour changes; and the
ability and willingness to share information and
feelings. Finally, evaluation of interventions that
attempt to increase patient control should take into
account outcomes such as confidence in the ability
to make decisions about treatment plans,
maintaining a personal health record, and other
major choices related to health management.
Research so far has revealed interdependencies
between these dimensions. For instance, Roter and
Hall (1992), extensively researched the
communication between doctors and patients and
have noticed that patient education helped patients
gain more control and management of their health,
which in turn encourage patients to ask more
questions and be more active regarding their health
treatment. Moreover, researches revealed that the
maintenance of control by obtaining information
about health statuses, lead to an increased
participation ratio in decision-making regarding
treatment (Makoul et al, 1995). Furthermore,
DiMatteo et al (1994) conclude that patient
education or structural changes to the medical
interaction (i.e. doctor and patient co-authoring
medical records) have led patients to play. more
active roles and develop a greater sense of control of
their health and lives. Despite such findings, current
literature lacks of a tiered, hierarchical approach
towards patient empowerment.
HEALTHINF2015-InternationalConferenceonHealthInformatics
606

0
500
1000
1500
2000
2500
3000
3500
4000
4500
5000
pubished papers per year
year of publication
patienteducation
patientengagement
patientempowerment
Figure 1: Plot of the PubMed search results for the terms “patient education” (red dashed line), “patient engagement” (green
dotted line), and “patient empowerment” (blue compact line). The results of the 3 searches are plotted as number of
published papers per year for the year range 1960 to 2013.
3 A COGNITIVE APPROACH TO
PATIENT EMPOWERMENT
In its core meaning, empowerment is strongly
related to the control on one’s own action. In this
respect, empowerment could be considered as a
complex construct that involves various cognitive
processes and skills (Falk-Rafael, 2001).
Specifically, some of its basic elements include:
knowledge acquisition, through perception, thinking
and learning, awareness of one’s own current
conditions and /or needs, active participation in the
management of the current or future condition and in
the relevant decision making. (Rappaport, 1984)
Following the overall approach of cognitive
psychology, we propose to treat patient
empowerment in terms of three levels of increasing
complexity and importance: awareness, participation
and control (Figure 2).
3.1 Awareness
The first and most basic level refers to the complex
task of health awareness. The patient (or the healthy
citizen in general) should be aware of: his or her
own health status; health related risks and lifestyle
or environment induced hazards; potential disease
progression to more severe stages; potential disease
transition to other comorbidities; measures needed to
stay healthy and/or prevent disease occurrence,
progression or transition.
This level corresponds to the educational
dimension as in current literature. However, we
believe that it is more appropriate to treat it as a
personal awareness of one’s own health rather than
the process of formal education. This underscores
the fact that the patient should clearly understand the
implications of the information provided and is able
to act upon it. In any case, this level on its own can
be viewed as an educational process with three sub-
levels of increasing complexity (Davenport and
Prusak, 2000): information gathering (i.e. simple
facts), knowledge (i.e. information with a purpose),
and understanding (i.e. conscious knowledge and
achievement of explanation). Supporting access to
information is the easiest and most straightforward
task for patient empowerment interventions, be it via
conventional channels of printed material, or via the
nowadays more popular channels based on the
internet and even mobile personal devices
Indeed, today there are many authoritative on-
line databases that provide education material
designed specifically for the patient. One notable
example is the effort of the National Library of
Medicine USA, who provides also the MedLinePlus
(www.nlm.nih.gov/medlineplus/) service for patient
information. Another important example is the
EUPATI network funded by EU. which is a
comprehensive collaborative effort towards
educating the patients so that can take active part in
their treatment and in the research towards new
treatments.
Structuring and organizing information with a
particular educational purpose refers to knowledge.
Managing and supporting this second level of the
PatientEmpowermentasaCognitiveProcess
607
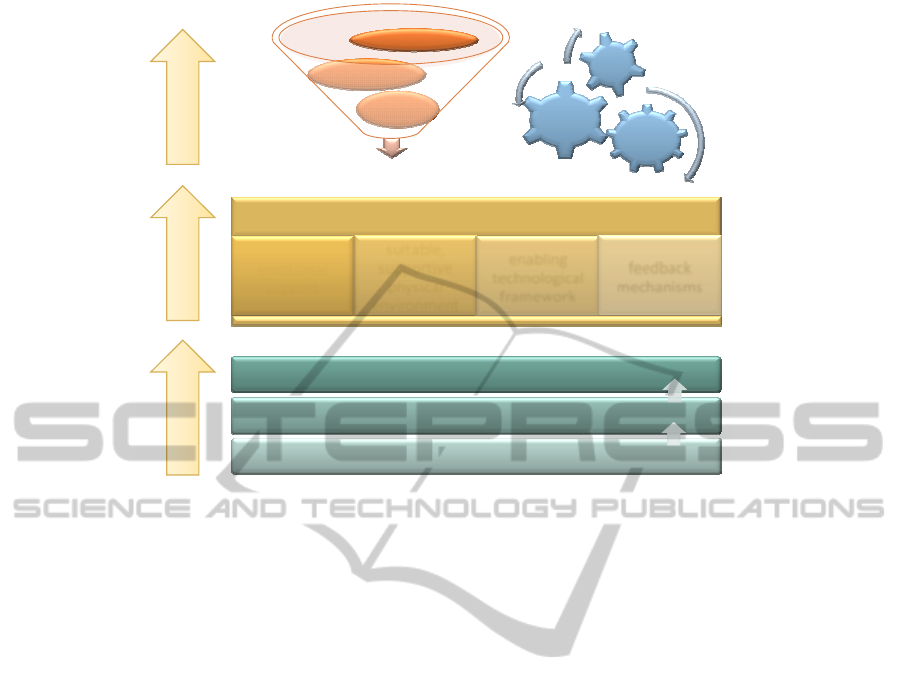
understanding:personalhealthconditionawareness
knowledge:relevant,structuredinformationwithapurpose
information:dataandinformationaggregation
awareness engagement control
action,participation
emotional
support
suitable,
supportive
physical
environment
enabling
technological
framework
feedback
mechanisms
cognitive
emotional
soc
ial
shareddecision
decision
support
collaboration
communication
mindchange
Figure 2: Patient empowerment modelled as a cognitive process. There are three distinct levels of increasing complexity
and importance: awareness, engagement and control. Each level presents its own contributing factors.
educational process is a rather complex issue.
Semantic eHealth interventions can certainly help by
providing relevant semantic medical concept maps
that will allow available medical evidence to be
presented to the patient within context. Also,
advanced visual analytics may offer alternative ways
for patients to grasp difficult medical concepts. The
final step of understanding relates to the patient’s
ability to realize his or her personal condition in
relation to the medical evidence. This actually
means achievement of health awareness. In order to
support this, interventions should follow a combined
approach of coupling medical knowledge to the
personal characteristics of the patient. This
personalization most often will require integration of
personal health data, real-time biomedical sensor
measurements, and data related to lifestyle and
behaviour, beliefs and intentions as harvested via
semantic analysis of unstructured personal data
available in web based social networks.
3.2 Engagement
This second level of patient empowerment strives to
achieve patient engagement in the health care
process. Here we should emphasize active and
proactive participation in managing the disease and
its treatment and in preventing disease progression
and transition. Successful patient participation can
really be achieved only when the patient is health
aware. However, this is not the only prerequisite.
The patient additionally needs emotional strength, a
suitable, supportive physical environment, an
enabling framework and last but not least accurate
feedback in order to be able to re-adjust participation
Emotional strength can generally be reinforced
by easing the communication with health providers
and most importantly within social groups. Both can
be easily supported by common eHealth
interventions that allow an easy and seamless
communication with health providers or provide the
environment for on-line social support groups.
Creating a supportive physical environment may
prove more intriguing. As we cannot easily alter
physical environments to help patients, we could
instead try to alter something equally important: the
perceived environment. Here, future eHealth
interventions should provide the means to identify
resources and opportunities the environment already
provides, which the patient (or its digital assistant)
can exploit to increase the level and quality of
participation in disease management. A simplistic
example would involve an application that
highlights a route within a city suitable for
wheelchairs or places that offer salt free foods.
For the patient to be able to participate
effectively in personal health management a number
of other tools and services often need to be available
– these comprise what we call the enabling
framework. These may include specialized
HEALTHINF2015-InternationalConferenceonHealthInformatics
608

equipment and/or digital interventions that provide
the necessary prerequisites for the patient to be able
to act. Fortunately, nowadays a wealth of such
underline technologies are available, ranging from
personal wearable health sensors to cloud based
personal health applications and dedicated personal
assistants. Finally, active participation requires
improvement of the self-efficacy (Bandura, 1977).
That is, it is necessary for the individual to know her
own abilities and skills or to estimate accurately her
needs for being able to be engaged in action. One of
the most crucial tools for the formation of the self-
efficacy is the accurate feedback, positive or
negative, for individual’s action that is received
from the external environment. Only active
engagement can be meaningful and effective in
fulfilling its aims.
3.3 Control
Control in this context can include two different
aspects: decision making and mind changing.
Decision making refers to a collaborative process
where patient and health professionals discuss and
interact to reach a shared decision. A prerequisite for
this is the patient to be health aware and also
actively involved in her health management. Only
then, the patients’ participation in decision making
should be effective. However, this aspect of control
involves extensive communication and
collaboration. Both are widely supported by current
eHealth applications in a variety of ways, including
also advanced collaboration environments and
shared digital spaces. Some interesting examples
include the emergent technology of personal health
records, owned by the patients themselves, who
however can give targeted access to their health
providers when needed. Also considerable research
work is available in the field of medical decision
support systems, which can be generally viewed as
either (a) the so-called ‘strong’ artificial intelligence
systems whose behaviour is at some level
indistinguishable from humans; or (b) an alternative
approach that looks at human cognition and decides
how it can be supported in complex or difficult
situations, something like a form of ‘cognitive
prosthesis’ that will support the human in a task
(Coreira, 2003). In any case, shared decision support
interventions need to take into account both patients
and health professionals and integrate data and
events from various sources of personal health data
and medical evidence. On the other hand, control of
action involves very internal cognitive processes –
what we refer to as mind changing, that is the
capacity to modify one’s own mental states like
beliefs or intentions . This entails the representation
of causal determinants of lasting behaviour change
from the perspective of the individual, including
perceptions, cognitions, and emotions. Together,
they describe the personal-level motivational
signature of direct goal-seeking behaviour (Piaget,
1976).
This level of empowerment is probably the most
demanding, since it is based on highly
interdisciplinary research which involves
behavioural scientists, psychologists, behaviour
simulation and experiments and finally information
scientists. Attempts to support mind changing need
to take into account individuals' motivations,
attitudes and habits, understand them and then
design an intervention which is aimed at changing
representations first, and then behaviours. Mind
changing is at the basis of human social interactions
because it means that we can identify others' mental
states and act upon them (Conte, 1995). This can be
obtained by several means: communicative actions,
like requests, commands, evaluations, assertions,
etc. and non-communicative actions, which aim to
modify the emotions, feelings, and beliefs of others
without directly stating one’s intentions.
4 CONCLUSIONS
The main point of this research is to justify how the
precise distinction of the three levels of patient
empowerment helps with its application, and help
the patient receive it more smoothly and easily. The
advantages of this process are that we can evaluate
each level separately and not only the final outcome,
identifying possible shortcomings and correcting
them along the way. In other words, the evaluation
and monitoring of patient empowerment have more
clear targets, thus provide new opportunities for
researchers to determinate where and when their
strategy should change. We plan to test the validity
of the model for the evaluation of a novel service
environment for providing personalized
empowerment and shared decision support services
for cardiorenal disease and comorbidities, as part of
the FP7-ICT project CARRE: Personalized Patient
Empowerment and Shared Decision Support for
Cardiorenal Disease and Comorbidities (Grant no.
611140). The project aims to create a set of
empowerment interventions that address all level of
the proposed empowerment model. In particular: (a)
provide visual model of disease comorbidities
trajectories, based on current medical evidence
PatientEmpowermentasaCognitiveProcess
609

(awareness: information aggregation and
knowledge); (b) personalize the risk model based on
his personal medical data and real-time sensors to
support status awareness (awareness:
understanding); (c) use the personalized model in
conjunction with real time monitoring to create a set
of alarms to enable patient engagement
(engagement: enabling framework); and (d) provide
advanced decision support services based on the
real-time coupling of medical evidence, personal
health status and intentions and beliefs, as deduced
from social web data mining (control). The ultimate
goal is to identify available evaluation tools for each
different part of the model and thus provide a
complete framework for the design and evaluation of
patient empowerment interventions.
ACKNOWLEDGEMENTS
This work was supported by the FP7-ICT project
CARRE (No. 611140), funded in part by the
European Commission.
REFERENCES
Ajoulat I, d’Hoore W., and Deccache A., 2007. Patient
empowerment in theory and in practice: Polysemy of
Cacophony, Patient Education & Counseling, 66:13-
20.
Anderson R.M., Funnell M.M., 2010. Patient
empowerment: myths and misconceptions. Patient
Educ Couns. 79(3):277-82.
Bandura, A. (1977) Self-efficacy: Toward a unifying
theory of behavioral change. Psychological Review,
84, 191-215.
Chatzimarkakis J., Why patients should be more
empowered, J Diab Science Technol, 4:1570-1573,
2010.
Coreira E., Guide to Health Informatics: 25: Clinical
decision support systems, 2nd Ed., Oxford Univ.
Press, NY, 2003.
Conte R, Castelfranchi C. Cognitive Social Action.
London: UCL Press, 1995.
Davenport, T.H., and Prusak L., 2000. Working
knowledge: how organizations manage what they
know. Boston, MA: Harvard Business School Press.
DiMatteo, M. R., Reiter, R. C., & Gambone, J. C., 1994.,
Enhancing Medication Adherence Through
Communication and Informed Collaborative Choice,
Health Communication, 6(4), 253-265.
Falk-Rafael A.R. (2001). Empowerment as a process of
evolving consciousness. A model of empowered
caring. Advances in Nursing Science, 24, 1, 1-6.
Freire P., 1993. Pedagogy of the oppressed., New York:
Continuum.
Israel, B. A. Checkoway, B. Schultz, A. and Zimmerman,
M., 1994. Health Education and Community
Empowerment: Conceptualizing and Measuring
Perceptions of Individual, Organizational and
Community Control. Health Education Quarterly
21(2): 149-170.
Lau D.H., 2002. Patient empowerment – a patient-centred
approach to improve care. Hong Kong Med J. 8 (5):
372-374.
Makoul, G., Arnston, P. & Schofield T., 1995. ‘‘Health
Promotion in Primary Care: Physician-Patient
Communication and Decision Making About
Prescription Medications,’’ Social Science Medicine,
41(9), 1241-1254.
McAllister M, Dunn G, Payne K, Davies L, Todd C.,
2012. Patient empowerment: the need to consider it as
a measurable patient-reported outcome for chronic
conditions. BMC Health Serv Res. 13;12:157.
Ouschan Robyn MMgt, Sweeney Jillian C., Johnson
Lester W., 2000. Dimensions of Patient
Empowerment, Health Marketing Quarterly, 18:1-2,
99-114.
Piaget, G. (1976). The grasp of consciousness. Action and
concept in the young child. Cambridge: Harvard
university press.
Rappaport J., 1987. Terms of empowerment/exemplars of
prevention: Toward a theory for community
psychology. American Journal of Community
Psychology, 15, 121-144.
Rappaport, J. (1984). Studies in empowerment:
Introduction to the issue. Prevention in Human
Services, 3, 1-7.
Robbins T.L, M.D. Crino, L.D. Fredendall, 2002. An
integrative model of the empowerment process.,
Human Resource Management Review, 12, 419–443.
Roter, D. I. and Hall, J. A., 1992. Doctors Talking With
Patients/Patients Talking With Doctors, London,
Auburn House.
The Lancet, 2012. Patient Empowerment – who empowers
whom? The Lancet, 379(9827): 1677.
Thomas K.W., Velthouse B.A., 1990. Cognitive Elements
of Empowerment An “Interpretive” Model of
Instrinsic Task Motivation, Academy of Management
Review, 15:4:666-681.
Traynor M., 2003. A Brief History of Empowerment:
Response to a Discussion with Julianne Cheek.
Primary Health Care Research and Development,
4:129-136.
Unver O., Atzori W., 2013, Deliverable 3.2.
Questionnaire for Patient Empowerment Assessment,
The SUSTAINS FP7 ICT PSP European Commission
project, No. 191905.
HEALTHINF2015-InternationalConferenceonHealthInformatics
610
