
EPIK
Virtual Rehabilitation Platform Devised to Increase Self-reliance of People with
Limited Mobility
Sonia Garrote
1
, Azael J. Herrero
1,2
, Miguel Pedraza-Hueso
3
, Carlos González-Gutiérrez
3
,
María V. Fernández-San Román
3
, F. J. Díaz-Pernas
3
, Héctor Menéndez
2
,
Cristina M. Ferrero
2
and Mario Martínez-Zarzuela
3
1
Faculty of Health Sciences, European University Miguel de Cervantes, Valladolid, Spain
2
Research Center in Physical Disability, ASPAYM Castilla y León Foundation, Valladolid, Spain
3
Imaging and Telematics Group, University of Valladolid, Valladolid, Spain
Keywords: Exergames, Rehabilitation, Stroke, Physical Therapy, Microsoft Kinect, Elderly.
Abstract: In this paper we describe a virtual rehabilitation platform designed to improve balance of people with
physical impairment using the Microsoft® Kinect® sensor. Different types of users can interact with the
platform: Administrators, therapists, and final users (patients), using their own interfaces and modules. Six
modules have been designed: Profile, Administrator, Evaluation, Therapist, Game and Results; but only four
have been implemented so far: Administrator, Evaluation, Therapist and Game. The Administrator’s module
is used to generate a database of exercises. The Therapist’s module allows therapists to configure the game
training session using combinations of exercises from the database. The patients’ or game module includes a
3D immersive environment, where they perform the prescribed rehabilitation exercises, previously
configured by a therapist. The platform is in its first beta version and ready to be tested.
1 INTRODUCTION
The live expectancy in countries like Spain is about
79 years for males and 85 years for females (World
Health Organization –WHO-, 2012). Different
factors like medical advances, allow a lot of people
to survive until their seventies or so far. However, in
many cases elderly people suffer chronic illness and
pathologies that reduce their mobility and make
them being dependent. Nowadays, one of the health
problems with a higher incidence in elderly subjects
is stroke. The risk of stroke doubles every decade
after age 55 (Mackay and Mensha, 2004). Patients
who suffer a stroke spend prolonged stays in
intensive care units and have a markedly higher
mortality rate (Hornero et al, 2013). These patients
usually suffer a paralysis that compromises their
ability to perform activities of daily living (ADLs)
(Nichols-Larsen et al., 2005). In order to maximize
patient outcomes and reduce disability it is essential
to carry out programs of physical rehabilitation
(Saunders, 2014).
Some programs applied to stroke patients during
the acute phase are based on Early Supported
Discharge (ESD). ESD consists on attending to the
acute stroke care and rehabilitation unit and pretend
an early discharge from hospital performing a
supervised rehabilitation program at home. These
programs can reduce long-term dependency, the
length of hospital stays and admission to
institutional care units (Fisher, 2011; Fearon and
Langhorne, 2012).
Nonetheless, what happens after the acute phase
of a stoke patient? Should patients continue the
rehabilitation programs in the chronic/late post
stroke period? The Evidence Based Review of
Stroke Rehabilitation states that there is strong
evidence about the effectiveness of balance training
programs to improve health-related outcomes. This
review also asserts that task-specific gait training
improves the gait after stroke, treadmill training
alone (without partial weight support) increases gait
velocity, and virtual reality training enhances gait
recovery (Teasell et al., 2013).
The Spanish healthcare system does not provide
these rehabilitation programs to stroke patients
188
Garrote S., Herrero A., Pedraza-Hueso M., González-Gutiérrez C., Fernández-San Román M., Díaz-Pernas F., Menéndez H., Ferrero C. and
Martínez-Zarzuela M..
EPIK - Virtual Rehabilitation Platform Devised to Increase Self-reliance of People with Limited Mobility.
DOI: 10.5220/0005484301880193
In Proceedings of the 1st International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AgeingWell-
2015), pages 188-193
ISBN: 978-989-758-102-1
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

during the chronic phase of the illness. Stroke
patients have to pay for these programs and have to
attend to special health centers to receive the
therapy. Nevertheless, what happens if patients live
too far from the rehabilitation institutions?
Moreover, how could patients continue and reinforce
their rehabilitation at home?
Virtual reality systems, including video games,
can help to reach this purpose. In a recently
published review, it was concluded that video games
improve health outcomes in areas like psychological
therapy and physical therapy. However, the authors
suggest that more rigorous Random Clinical Trials
are needed to confirm this effectiveness (Primack et
al., 2012). Other researchers denote an increment in
the motivation of the patients towards physical
rehabilitation (Kato, 2010; Chang et al., 2011),
improvements in their motor skills and physical
condition (Jansen-Kosterink et al., 2013) or,
encouraging results for recovery of muscle force and
power of the lower limb for individuals with chronic
hemiparesis (Mirelman et al., 2010). These kinds of
developments are cost effective since they can
benefit a large number of patients and can improve
patients’ health.
Our multidisciplinary research group, which
includes physiotherapist, professionals in physical
activity and sport sciences, computer science
engineers and telecommunications engineers, aims
to design and implement virtual reality therapies
based on serious games.
This paper shows the technical specification of a
rehabilitation platform (EPIK) under development
by our research group. EPIK is similar to other
virtual rehabilitation systems like KiRes (Anton,
2013) that uses the Microsoft Kinect sensor to
interact with the users. In contrast to KiRes, the
administrator does not need to record his postures
using Kinect to create new exercises, so the time that
is needed to include a new exercises program into
the database is significantly decreased. Gamification
techniques such as an immersive 3D environment,
game levels, game modes, velocity, game session
time and victory points have been used to develop
EPIK. For this reason, the patient enjoys a “game
sensation” that increases his motivation, distracts
him from his illness and engages him to the system
decreasing the rate of neglect.
Other researchers (Su, 2013, Robertson et al.,
2013, Rajaratnam et al., 2013, Pirovano et al., 2012,
Muñoz et al., 2013), use Kinect based systems in the
physical rehabilitation area. However, those works
do not present a complete platform and do not either
include gamification nor have been tested using
random clinical trials. In a recent systematic review
(Da Gama et al., 2015) it is pointed that a complete
system must be developed to include aspects like
therapeutic configuration, different exercise
possibilities, guidance and feedback. EPIK has the
aim to pave the way to resolve all these lacks.
At this moment, we have designed a random
clinical trial (RCT), following the CONSORT
recommendations (Boutron et al., 2008) to test this
first prototype with users with reduced mobility
problems caused by a stroke. The RCT has been
performed in a physiotherapy research center. The
patients are in the chronic stage of their illness. The
results obtained in the tests will serve to improve the
platform and obtain the first operative release.
2 METHODS
2.1 Purpose of the System
The aim of the system is to improve the level of
independency of people with reduced mobility such
as elderly, subjects with physical disabilities or
physical damage, using a virtual platform for
physical training.
Although anyone can use this virtual platform as
a training tool, it has been designed with the aim of
improving the balance of users with reduced
mobility.
2.2 Technologies
The EPIK platform employs the Microsoft Kinect
v.2 sensor (http://www.microsoft.com/en-us/kinect
forwindows) to capture users’ movements and
includes a game module to train the users’ body.
The platform has been programmed with Unity
(http://unity3d.com/), a “game development
ecosystem” able to create interactive 3D and 2D
content and run it in multiplatform systems like
Desktop (PC, Mac and Linux), Web, iOS, Android
and consoles (i.e. Xbox, Wii, PS4).
The recommended hardware and software
configurations for EPIK are: a Microsoft Kinect
sensor v.2, a PC with Microsoft Windows v.8 or
later with the Kinect drivers installed and the
Microsoft recommended hardware configuration.
2.3 Main Features
The EPIK platform is comprised of these modules:
Profile module: it is used to maintain user’s basic
EPIK-VirtualRehabilitationPlatformDevisedtoIncreaseSelf-relianceofPeoplewithLimitedMobility
189

information: username, password, permissions,
patient’s clinical records. This module is under
development.
Administrator’s module: it is used to create a
database of exercises and classify them in levels. In
each level we can create groups of exercises –
specific human body positions that we call
‘silhouettes’–. Thus, a level can have different
groups. In beta version.
Evaluation module: it is used to evaluate the
range of movement (ROM) of the user joints. In beta
version.
Therapists’ module: the therapist can design the
game sessions for the user choosing groups of
exercises. In beta version.
Results module: to analyze the evolution of the
patient. This module is under development.
Game module: in the game module, two human
figures are showed to the patient. The first figure is
the virtual image of the user that is training, that is,
the user’s avatar. The second figure is a silhouette
moving towards the user’s avatar under a
configurable velocity. The user must adopt the pose
of the silhouette so that his avatar matches it in order
obtain different scores in the game (Figure 1). In
beta version.
Figure 1: The user’s avatar (in first plane) must to adopt
the position of the silhouette to imitate (in second plane).
The silhouette to imitate comes towards the user's avatar
with a predefined velocity.
2.4 Account Types
Depending on the type of user account, the user is
able (or not) to access a given module in the EPIK
platform, with more or less permissions.
Patient’s account: if you have a patient account,
you are the person who uses the platform for your
physical training. You can access to the next
modules: profile module with read permission,
evaluation module with execution permission, game
module to play the game sessions configured for you
and results module with read permission.
Administrator’s account: the administrator has
full access to all modules with full permissions. His
main job is to create the silhouettes by configuring
their positions and save them in the database. The
therapist uses this database to design the game
sessions of a patient.
Therapist’s account: a therapist has full access to
the Therapist’s module. In this module the therapist
can see all the silhouettes of the database classified
into levels and groups by the administrator using the
Administrator’s module. The therapist selects groups
of silhouettes for each patient’s game session. The
therapist can access the rest of the modules with full
permissions, except to the Administrator’s module.
2.5 Modules of the System
2.5.1 Administrator’s Module
In the Administrator’s module silhouettes for a given
level of difficulty can be created. Silhouettes can be
generated by rotating the skeletal joints of an avatar
up to the desired position (Figure 2). Silhouettes
being generated can be grouped to ease the
configuration of a rehabilitation session afterwards.
The Administrator’s module does not restrict the
type of silhouettes that the administrator can create.
It is the administrator who is responsible of
following a previously agreed protocol about the
type of exercises to be included on a specific level.
Figure 2: Window to create groups of silhouettes in a
level.
This protocol has, for each level, the type of
recommended movements. In Table 1 we can see the
types of exercises that protocol has for level 1. A
higher level should imply a greater difficulty. Our
physiotherapists and professionals in physical
activity and sport sciences have created this protocol
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
190

based in their experience with physically disabled
patients. The protocol has six levels of difficulty.
Here, we show only the first one, as an example.
In case that the protocol needs to be changed in
the future, it would not be necessary to change any
line of source code of the Administrator’s module,
because there are no restrictions to create whatever
silhouette that the administrator desires.
Table 1: Type of movements for level 1.
Level 1
Description Postures with trunk movements and
unilateral upper limb movements
Movements Shoulder abduction, horizontal
abduction, shoulder flexion, shoulder
extension, lateral trunk tilt, trunk flexion
and extension
Detail The silhouettes may adopt combinations
of these movements always with bipodal
support, legs hip width apart and knee
totally extended. Body weight will be
evenly distributed between both feet or
more weight on one leg than the other.
2.5.2 Evaluation Module
The evaluation module measures the maximum
ROM of each joint when certain movements are
performed. These movements are defined in the
evaluation protocol designed by our physiotherapists
and professionals in physical activity and sport
sciences (Table 2).
The patient stands opposite to the Microsoft
Kinect sensor and can see his own representation in
the screen (his avatar) on the right and an avatar
performing an exercise that he or she has to imitate
on the left (Figure 3).
Figure 3: Evaluation module.
Two performances of the same movements
(Table 2) have to be carried out by the patient. The
user performs the movements in real time while they
are showed in the screen. When the two sequences
of movements are finished, the system computes the
maximum ROM that he or she reaches, using the
information collected during the two performances.
All the movements start from a base position: the
body erect with the arms at the sides and the palms
forward. In each movement, the user tries to reach
his maximum ROM and then, returns to the base
position.
Table 2: Sequence of movements during the evaluation
phase.
Abduction of the right shoulder, then left and finally
both bilaterally
Flexion of the right shoulder, then left and finally both
bilaterally
Horizontal abduction of the right shoulder, then left and
finally both bilaterally
Extension of the right shoulder, then left and finally
both bilaterally
Trunk tilt left and right. Trunk flexion and extension
Abduction right hip and then left (only exercise with
unilateral support, not for hip abduction exercises in
bilateral support)
Right hip flexion and then left (only for unilateral
support exercises and knee flexion)
Bending both knees (squat)
Step to the right side. Step to the left side. Step forward
with the right foot. Step forward with the left foot
2.5.3 Therapist’s Module
In this module the therapist can configure the game
session for each user. A game session represents the
groups of exercises. It is possible to choose groups
of silhouettes from different levels. For example: the
therapist can choose two groups of silhouettes from
level one, and one group of silhouettes from level
two; or he can choose one group from level two, and
one group from level five. There is total flexibility to
select whatever the therapist wants.
2.5.4 Game Module
Once the therapist has created the game sessions for
a given patient, the game module can be ran.
First, we select the patient that is going to play.
Second, we select the avatar.
Third, we select one of the sessions configured
for this user.
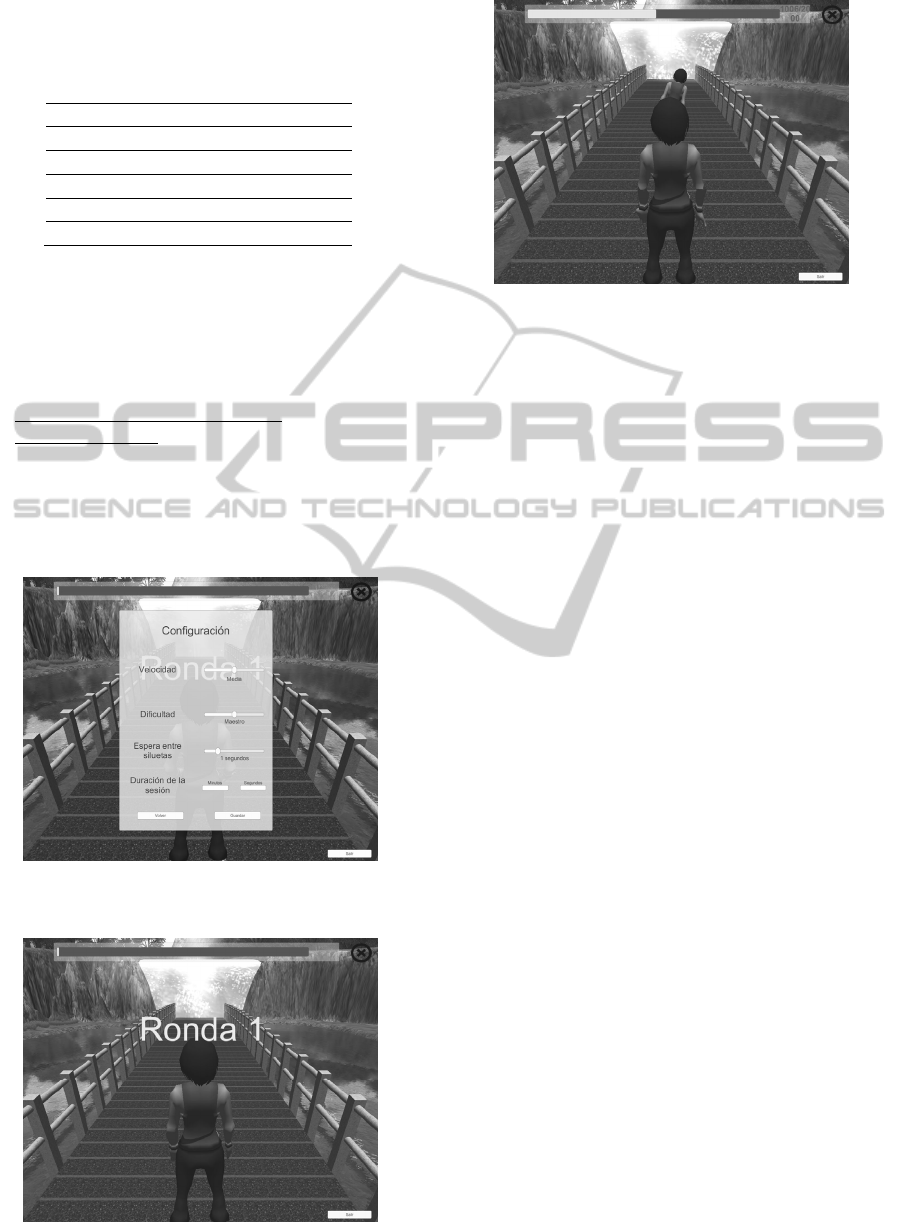
Fourth, we set the next parameters (Figure 4):
Speed: time it takes for the silhouette to reach the
user’s avatar (Figure 1). A higher speed implies a
greater difficulty.
Mode: this parameter is used to dynamically
adapt the silhouettes to be played using a percentage
of the maximum ROM that the user obtained in the
EPIK-VirtualRehabilitationPlatformDevisedtoIncreaseSelf-relianceofPeoplewithLimitedMobility
191
evaluation module. It is used to adjust the difficulty
of the game session.
Table 3: Types of Game Modes.
Mode % of the maximum ROM
Beginner 80%
Official 90%
Master 100%
Doctor 105%
Expert 110%
Suppose that, in the evaluation module, the user
performed an abduction movement of the arm and
his maximum ROM was 60º. If the therapist sets the
game session mode to beginner, the user will need to
rise his arm up to the 80% of 60º -48º- to obtain the
best score.
Waiting time between silhouettes.
Length of session: duration of a training session.
It is measured in minutes and seconds. The user
scores when he adopts the correct posture, in other
case there is no penalization. The concept of "life"
does not exist. Users do not loss a "life" when they
perform incorrect movements. The training session
Figure 4: Setting the session parameters in the game
module.
Figure 5: The first round of the game starts.
Figure 6: The user playing.
continues until the end or until it is paused. The
length of the session is a key configuration
parameter from the clinical point of view.
In the last step, the game starts (Figure 5), takes
place (Figure 6), finishes and saves results.
3 CONCLUSIONS
This paper presents the beta version of the EPIK
platform. A new Microsoft Kinect sensor based
system developed to improve balance through
training sessions played in a virtual 3D environment.
EPIK has a serious exergame that can be easily
configured to include exercises oriented to improve
patient’s movements velocity, coordination,
flexibility, etc.
All the EPIK modules have been designed with
the support of physical rehabilitation professionals.
Moreover, EPIK is being tested with stroke patients
today. The results of these tests will be used to
further improve the system and to have, in the near
future, an effective rehabilitation-assisted
technology with a real user centered design.
The aim is to construct a complete system using
a low cost sensor like Microsoft Kinect that will
address the evaluation and treatment cycle of a
patient in a simple and inexpensive way.
REFERENCES
Antón D., Goñi A., Illarramendi A., Torres-Unda J.J.,
Seco J., 2013. KiRes: A Kinect-based
telerehabilitation system. IEEE 15th International
Conference on e-Health Networking, Applications and
Services, 456-460.
Boutron I., Moher D., Altman D.G., Schulz K.F., Ravaud,
P., 2008. Extending the CONSORT statement to
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
192

randomized trials of nonpharmacologic treatment:
explanation and elaboration. Annals of Internal
Medicine, 148(4), 295-309.
Chang Y.-J., Chen S.-F., Huang J.-D., 2011. A Kinect
based system for physical rehabilitation: A pilot study
for young adults with motor disabilities. Research in
Developmental Disabilities, 32(6), 2566–2570.
Da Gama A., Fallavollita P., Teichrieb V., Navab, N.,
2015. Motor rehabilitation using Kinect: A systematic
review. Games for Health Journal, 4(2), 123-135.
Fearon P., Langhorne P., 2012. Services for reducing
duration of hospital care for acute stroke patients.
Cochrane Stroke Group, 9, 1-97.
Fisher R.J., Gaynor C., Kerr M., Langhorne P., Anderson
C., Bautz-Holter E., Indredavik B., Mayo N.E., Power
M., Rodgers H., Rønning O.M., Widén-Holmqvist L.,
Wolfe C.D., Walker M.F., 2011. A consensus on
stroke: early supported discharge. Stroke, 42(5), 1392-
1397.
Hornero .F, Martín E., Rodríguez R., Castellà M., Porras
C., Romero B., Maroto L., Pérez De La Sota E, 2013.
A multicentre Spanish study for multivariate
prediction of perioperative in-hospital cerebrovascular
accident after coronary bypass surgery: the PACK2
score. Interact Cardiovasc Thorac Surg, 17(2), 353-
358.
Jansen-Kosterink S.M., Huis in ’t Veld R., Schönauer C.,
Kaufmann H., Doz Mag P., Hermens H.J.,
Vollenbroek-Hutten M., 2013. A Serious Exergame
for Patients Suffering from Chronic Musculoskeletal
Back and Neck Paint. (Pilot Study). Games for Health
Journal: Research, Development, and Clinical
Applications, 2(5), 299-307.
Kato P.M., 2010. Video games in health care: Closing the
gap. Rev. Gen Psychol, 14(2), 113-121.
Mackay, J., Mensha G. A., 2004. The Atlas of Heart
Disease and Stroke. Risk factors. World Health
Organization (WHO), in conjunction with the USA's
Centers for Disease Control and Prevention (CDC) of
the U.S. Department of Health and Human Services,
and is strongly supported by NGOs such as the World
Heart Federation (WHF). Available: http://www.who.
int/cardiovascular_diseases/en/cvd_atlas_03_risk_fact
ors.pdf?ua=1 (Last visited Feb. 4, 2015).
Mirelman A., Patritti B. L., Bonato P., Deutsch J. E.,
2010. Effects of virtual reality training on gait
biomechanics of individuals post-stroke. Gait &
Posture, 31(4), 433-437.
Muñoz J., Henao O., López J., Villada J., 2013. BKI:
Brain Kinect Interface, a new hybrid BCI for
rehabilitation. Games for Health, 233-245.
Nichols-Larsen D.S., Clark P.C., Zeringue A., Greenspan
A., Blanton S., 2005. Factors influencing stroke
survivors' quality of life during subacute recovery.
Stroke, 36(7), 1480-1484.
Pirovano M., Mainetti R., Baud-Bovy G., Lanzi P.L.,
Borghese N.A., 2012. Self-adaptive games for
rehabilitation at home. Computational Intelligence and
Games (CIG), 2012 IEEE Conference on IEEE, 179-
186.
Primack B. A., Carroll M.V., McNamara M., Klem M.L,
King B., Rich M., Chan C.W., Nayak S., 2012. Role
of Video Games in Improving Health-Related
Outcomes A Systematic Review. American Journal of
Preventive Medicine, 42(6), 630-638.
Rajaratnam B., Gui KaiEn J., Lee JiaLin K., SweeSin K.,
Sim FenRu S., Enting L., Ang YiHsia E., KeatHwee
N., Yunfeng S., Woo YingHowe W., 2013. Does the
Inclusion of Virtual Reality Games within
Conventional Rehabilitation Enhance Balance
Retraining after a Recent Episode of Stroke?.
Rehabilitation research and practice, vol. 2013,
Article ID 649561, 6 pages.
Robertson C., Vink L., Regenbrecht H., Lutteroth C.,
Wünsche B.C., 2013. Mixed reality Kinect Mirror box
for stroke rehabilitation. 2013 28
th
International
Conference of Image and Vision Computing New
Zealand (IVCNZ), 231–235.
Saunders D.H., Greig C.A., Mead G.E., 2014. Physical
activity and exercise after stroke: review of multiple
meaningful benefits. Stroke, 45(12), 3742-3747.
Su C.J., 2013. Personal rehabilitation exercise assistant
with kinect and dynamic time warping. International
Journal of Information and Education Technology,
3(4), 448-454.
Teasell R., Foley N., Salter K., Richardson M., Allen L.,
Hussein N., Bhogal S., Jutai J., Speechley M., 2013.
Evidence - Based Review of Stroke Rehabilitation.
Executive Summary (16th Edition). EBERSR.
Available: http://www.ebrsr.com/ (Last visited Feb. 4,
2015).
World Health Organization (WHO), 2012. Global Health
Observatory Data Repository. Available:
http://apps.who.int/gho/data/node.main.688. (Last
visited Feb. 4, 2015).
EPIK-VirtualRehabilitationPlatformDevisedtoIncreaseSelf-relianceofPeoplewithLimitedMobility
193
