Brain-Computer Interface and Functional Electrical Stimulation for
Neurorehabilitation of Hand in Sub-acute Tetraplegic Patients
Functional and Neurological Outcomes
Bethel C. A. Osuagwu
1
, Leslie Wallace
2
,
Mathew Fraser
2
and Aleksandra Vuckovic
1
1
School of Engineering, College of Engineering and Science, University of Glasgow, Glasgow, U.K.
2
Queen Elizabeth National Spinal Injuries Unit, Southern General Hospital, Glasgow, U.K.
Keywords: Brain Computer Interface, Functional Electrical Stimulation, Neurorehabilitation, Tetraplegia, Hand.
Abstract: The aim of this paper is to compare neurological and functional outcomes between two groups of subacute
hospitalised patients with incomplete tetraplegia receiving two experimental therapies. Seven patients
received 20 sessions of Brain Computer Interface (BCI) controlled Functional Electrical Stimulation (FES)
while five patients received 20 sessions of passive FES. The treatment assessment measures were EEG during
movement attempt, Somatosensory evoked potential (SSEP) of the ulnar and median nerve and the range of
movement of both wrists. Patients in both groups initially had intense cortical activity during a movement
attempt, which was wide-spread, not restricted to the sensory-motor cortex. Following the treatment, cortical
activity restored towards the activity in able-bodied people in BCI-FES group only. SSEP also returned in 3
patients in BCI-FES group while in FES group no changes were noticed. The range of movement improved
in both groups and results are inconclusive due to the small number of participants. This study confirms the
feasibility of prolonged BCI-FES therapy in a hospital setting. The results indicate better neurological
recovery in BCI-FES group. Larger and longer studies are required to assess the potential advantage of BCI-
FES on functional recovery.
1 INTRODUCTION
Brain Computer Interfaces (BCI) controlled
functional electrical stimulation (FES) has two main
applications for neurologically injured patients: to
restore the lost function as an assistive device for a
long term use (Pfurtscheller et al. 2003) or to improve
a partially preserved function. In the latter case, BCI-
FES is used as a rehabilitative device on a short-term
basis (Fei et al. 2008, Daly et al. 2009, Tan et al. 2011,
Tam et al. 2011, Young et al. 2014, Mukaino et al.
2014, Li et al. 2014). The main advantage of
rehabilitation based on BCI-FES over FES alone is
that it is based on patient’s active intention to move
and it simultaneously activates sensory and motor
pathways, thus promoting neuroplasticity based on
associative, Hebbian learning (Hebb 1949).
Experiments on able-bodied people showed that
Motor Evoked Potential (MEP) is enhanced more
when the grasp function was guided by BCI-FES than
when it was guided by either BCI or FES alone
(McGie et al.2014).
Most publications advocating BCI-FES for
rehabilitation purposes are case studies on stroke
patients (Fei et al. 2008, Daly et al. 2009, Tan et al.
2011, Tam et al. 2011, Young et al. 2014, Mukaino et
al. 2014). Larger studies or studies including other
groups of patients are rare. Only recently a BCI-FES
study on stroke patients has been published including
a control and a treatment group (Li et al. 2014). Li et
al. showed that patients receiving BCI-FES achieved
better functional and neurological recovery than
patients receiving FES alone. Another randomised
controlled trial on stroke patients (Kim et al. 2015)
showed better functional improvement in patients
receiving BCI-FES as compared to patients receiving
FES only, but failed to present any result showing
brain activity pre and post therapy. Also recently, our
group showed the feasibility of BCI-FES therapy on
spinal cord injured patients. In that study on two
patients early after injury, we showed that BCI-FES
could be therapeutically used in incomplete
tetraplegic patients in a hospital setting (Vuckovic et
al. 2015). In the current study, we further explore the
potential of BCI-FES for rehabilitation of hand
functions in people with tetraplegia (high level spinal
Osuagwu, B., Wallace, L., Fraser, M. and Vuckovic, A..
Brain-Computer Interface and Functional Electrical Stimulation for Neurorehabilitation of Hand in Sub-acute Tetraplegic Patients - Functional and Neurological Outcomes.
In Proceedings of the 3rd International Congress on Neurotechnology, Electronics and Informatics (NEUROTECHNIX 2015), pages 15-23
ISBN: 978-989-758-161-8
Copyright
c
2015 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
15
cord injury SCI). We compare neurological and
functional outcome between the group of patients
receiving 20 sessions of BCI-FES hand therapy with
a matched control group receiving the same number
of therapy sessions with passive FES.
2 MATHERIALS AND METHODS
2.1 Patients
Twelve subacute patients with tetraplegia (12 male,
51.7±18.4 min 20, max 75) participated in the study.
All patients were three months or less post-injury,
were still at the hospital and had therefore received
daily standard hand therapy in addition to the
experimental therapy (Table 1). Their level of injury
was cervical, C4-C7 affecting both hands. All patients
had incomplete injury, ASIA B or C, meaning that
they had partially preserved sensation by no
preserved movement (ASIA B) or had partially
preserved both sensation and movement (ASIA C)
(Marino et al., 2003). Because of the small number of
patients with SCI, a semi-random order of
recruitment was created in advance assigning patients
to the one or the other treatment group. Patients were
assigned upon recruitment to a corresponding group
(20 patients in total are planned for the whole study,
that is still running).
The study has been approved by the National
Healthcare Service Regional Ethical Committee. This
study is a registered clinical trial NCT01852279.
2.2 Initial and Final Assessments
The study consisted of three phases: initial
assessment, treatment and final assessment. Initial
and final assessment consisted of identical tests. Test
were divided into neurological and functional. The
neurological tests comprised of
electroencephalography (EEG) recording during left
and right hand movement attempts (MA) and somato-
sensory evoked potential (SSEP) of the median and
ulnar nerves of both hands. The functional
assessments consisted of measurement of the range of
movement of the left and right wrist and Manual
Oxford Scale muscle test MMT (Porter, 2013) of
hand and arm muscles. MMT test has 6 grades (0=no
contractions felt in the muscle, 5=hold test position
against strong pressure). Due to the nature of the
injury, initially patients had better preserved
voluntary control of muscles in shoulders and upper
arms (MMT=3 to 4) than of the forearm, wrist and
hand. Initial MMT of the forearm/hand muscles was
between 0 and 2 (MMT=2 moves through the range
of motion through a horizontal plane, i.e. cannot resist
gravity). Formarm/hand muscles involved supinator,
pronator, extensor digitorum communis, extensor
carpi radialis brevis and longus, flexor carpi radialis
and flexor digitorum profundis. Due to the large
number of assessed muscles, the MMT outcome will
be presented elsewhere. Functional and neurological
assessments were performed on different days, to
minimise patients’ discomfort.
2.2.1 Cue-based Movement Attempt
A standard cue-based paradigm was implemented
with rtsBCI, a part of the open source Biosig toolbox
(Vidaurre et al. 2011), implemented under Simulink,
MATLAB (Mathworks, USA). Patients sited in their
wheelchairs approximately 1.5 from a computer
screen. A trial started at t=-3 s and ended at t=3 s. At
t=-1s a warning cue (a cross) was presented at the
screen. At t=0s an execution cue (an arrow) appeared
on the screen. After t=3s the screen stayed blank for
a random period of 1-3 s before the next trial. Total
time between two trials was random, between 7s and
9s. There were two types of arrows, an arrow pointing
to the right for MA of the right hand and to the left for
the MA of the left hand. Patients were instructed to
attempt waving their hand continuously from t=0s till
t=3s. Note that unlike able-bodied persons, paralysed
people can differentiate between imagination of
movement and movement attempt, in the absence of
overt movements. Because the aim of the study was
the restoration of voluntary hand movement, we
considered MA being more appropriate task than the
imagination of movement. There were 120 trials (60
for each hand) divided in 4 runs each consisting of 30
trails (15 for each hand)
During this task patients’ EEG was measured with
48 electrodes placed according to the 10/10 system
(Jurcak et al, 2007) using usbamp device (Guger
technologies, Austria). Electrodes covered the central
region of the sensory-motor cortex, parietal cortex
and sparsely covered the frontal and occipito-
temporal cortices. Forty seven electrodes were used
to record EEG while one electrode was placed at the
lateral cantus of the orbicularis oculi of the right eye
to record electrooculogram (EOG). EEG was
recorded with respect to the linked-ear reference with
the sampling frequency of 256 samples/s. Impedance
was kept under 5 kΩ. A ground electrode was placed
at the electrode location AFz. EEG signal was filtered
on-line between 0.5 and 60 Hz and notch-filtered at
NEUROTECHNIX 2015 - International Congress on Neurotechnology, Electronics and Informatics
16
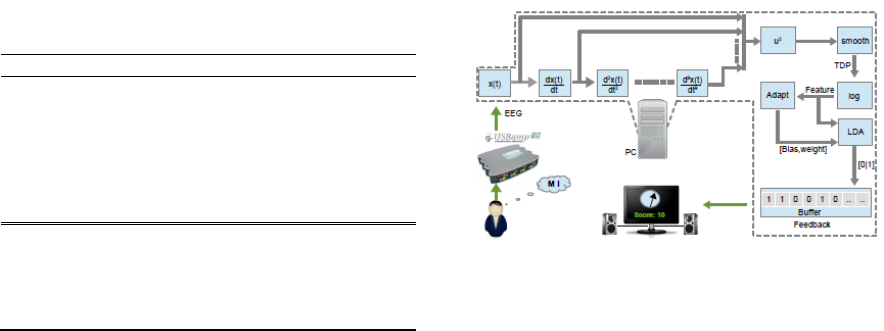
Table 1: Information about patients. First 7 patients
received BCI-FES therapy, last five received FES therapy.
Patient Injury level ASIA Age
1 C6 C 70
2 C4 B 25
3 C6 B 32
4 C5 C 20
5 C6 C 74
6 C5 B 51
7 C6/7 C 61
8 C5 C 36
9 C5/6 C 61
10 C6 C 75
11 C4 B 51
12 C6 C 64
50 Hz using the IIR digital Butterworth filter built
into a modular amplifier.
2.2.2 Off-line Analysis of EEG during
Movement Attempt
Continuous data were split into trials starting at t=-3
and ending at t=3s, with respect to the execution cue.
Datasets of each patients were decomposed into
independent components (IC) (Hyvarinen, and Oja,
2000) using Infomax algorithm implemented in
EEGlab (Delorme and Makeig, 2004) under Matlab
(Mathworks, USA). Components were visually
inspected and components corresponding to noise
(line noise, EOG, EMG and ECG) were removed and
signal was back projected into EEG domain. A
common average reference was computed for all
channels.
Time-frequency analysis was performed in
EEGlab based on event-related spectral perturbation,
which is an extension of the event-related
synchronisation/desynchronisation (ERD/ERS)
(Pfurtscheller and da Sliva, 1999). A baseline period
was from t=-2s till t=-1s. The Morlet wavelet
transform was used to perform a time-frequency
analysis in 3-60 Hz, with a Hanning-tapered window
applied and the number of cycles set to 3 at the lowest
frequency.
An average ERD/ERS across patients was created
using Study structure in EEGlab. Average ERD/ERS
scalp maps for a chosen frequency band and time
window were created through Study structure. The
statistical non-parametric method with Holm’s
correction for multiple comparisons (Holm, 1979)
was used to test for statistically significant differences
between ERD/ERS scalp maps before and after
treatments of patients within a group, with a
significance level set to p=0.05.
Figure 1: BCI setup showing computation of TDP.
2.2.3 Somato-sensory Evoked Potential
Somatosensory evoked potential is a response of the
central nervous system to an electrical stimulation
(Gugino and Chabot, 1990). The SSEP may infer
motor functions on the assumption that an injury
severe enough to a damage the sensory pathways
may also affect motor pathways. The SSEP was
analysed to detect the latency and the amplitude of the
N20 peaks that occurs around 20ms following an
electrical stimulus. In able-bodied people N20 latency
is highly repeatable. The increased delay of N20 is an
indicator of the damage of the neural pathways. The
damage results in axon demyelination which causes
reduced propagation velocity along the axon,
manifested as the increased latency of N20 peak. In
more severe cases, the amplitude of N20 is reduced
or it is completely absent (Curt and Dietz 1999). The
recovery of the neural pathways, followed by re-
myelination, results in re-appearance of the N20 and
in reduced N20 latency.
In the current study SSEP was measured for the
left and right median and ulnar nerves, as these two
nerves share innervation of the wrist and fingers. All
the four nerves were stimulated separately, one at the
time using a single pulse electrical stimulation
(Model DS7, Digitimer,UK). Electrodes were
attached on the surface of the skin above the
corresponding nerves at the wrist. A stimulation
intensity was set so that a small visible twitch could
be observed at the thumb for the median nerve and at
the little finger for the ulnar nerve. For each nerve,
electrical stimulation was delivered 250 times with a
frequency of 3 Hz. SSEP of the right hand median and
ulnar nerve was measured at the electrode location
CP3 and of the left hand nerves at the electrode
location CP4. EEG was recorded with usbamp, with
a sample rate of 4800 Hz, band passed between 2-
2000 Hz and notch filtered at 50 Hz. Individual
responses were averaged with respect to the onset of
stimulation.
Brain-Computer Interface and Functional Electrical Stimulation for Neurorehabilitation of Hand in Sub-acute Tetraplegic Patients -
Functional and Neurological Outcomes
17

2.2.4 Measurement of the Range of Motion
of the Wrist
In patients with incomplete tetraplegia who have
partially preserved control of movement, the range of
motion (ROM) is reduced, as compared to the able-
bodied people. The ROM of the right and left hand
wrist, during extension and flexion was measured
using Zebris system (Zebris Medical GmbH,
Germany). The measurement procedure is based on
the travel time measurement of ultrasonic pulses. The
pulses are emitted by three stationary transmitters and
are recorded by small markers which are ultrasound
microphones. The Zebris system markers were placed
on bony landmarks on the subject’s hand at the radius
(marker 1), carpometacarpal joint (marker 2) and the
carpometacarpal bone (of the index finger or the
thumb, marker 3). The ROM was calculated as an
angle between intersecting imaginary lines formed
between markers 1-2 and markers 2-3.
2.3 Therapy Sessions
Treatment consisted of 20 sessions, each lasting
approximately one hour, organised 3-5 times weekly,
depending on patients’ availability. One group of
patients received active therapy; they attempted hand
movement that was detected by BCI which then
activated FES applied to their hand muscles (BCI-
FES group). The other group of patients received
passive on-off FES therapy (FES group). They got
the same amount of FES stimulation as BCI-FES
group but the stimulator was activated automatically.
In both groups, therapy was applied on both hands, as
spinal cord injury typically affects both hands, though
not necessarily to the same extent.
2.3.1 Off-line Brain Computer Interface
based on Movement Attempt
The BCI algorithm was based on time-domain
parameters (TDP) (Vidaurre et al. 2009). On each
day, a quick off-line session was recorded consisting
of 20 trials for each hand, following the experimental
protocol described in 2.2.1. In our previous study on
able-bodied people (Osuagwu and Vuckovic 2014),
we showed that such short recording session results
in an initial classification accuracy between 75% and
100%. Note that off-line classifier parameters are
further updated and refined during on-line BCI, as
described later in the text. During therapy sessions,
patients’ EEG was recorded from three pairs of
bipolar electrodes located over the sensory-motor
cortex, CP3-CF3, CPz-CFz and CP4-CF4. EEG was
recorded with usbamp, band-filtered online between
0.5 and 30 Hz (5
th
order Butterworth filter), with
sampling frequency 256 Hz. The ground electrode
was attached to the ear. The impedance was kept
under 5 kΩ.
Time domain parameters were calculated for 7-30
Hz EEG frequency band using equation 1
()
pj
j
dt
j
tdX
TDP ,...0var =
=
(1)
Where X(j) is a wide-band EEG, t is a current sample,
j is a derivative (p=9), ‘var’ is a variance operator and
‹.› was used to present smoothing/averaging
operator. Smoothing was a result of applying a one
second long moving average filter. The variance
operator in this equation acts as the band-power
operator since the variance of the band-passed filtered
signal is equal to the bandpower (Vidaurre et al.
2009). The BCI setup showing computation of TDP
is shown in Fig. 1. The squaring and smoothing (Fig.
1), performed over 1s is a part of a band-power
calculation. Following this, logarithmic
transformation of TDP parameters was performed to
enforce normal distribution required for classifier
based on linear discriminant analysis (LDA)
(Fukunaga, 1990).
2.3.2 On-line Brain Computer Interface
based on Movement Attempt
During therapy a session, BCI was used on-line with
classifiers to discriminate between a hand movement
and no movement. To improve performance of BCI
on-line LDA classifier, the mean values of both
classes and the within class covariance matrix were
updated during training. The on-line adaptation was
necessary due to small number of off-line trials. Short
off-line training was needed due to a limited time
patients had for the study, which had to fit within their
daily routine (typically 1 hour for BCI setup and for
training of both hands).
The difficulty of activation of BCI was adjustable,
so difficulty can be e.g. increased to reduce the false
positive rate or decreased to make a task easier for a
patients who is tired or has a low concentration. The
difficulty was adjusted by setting the length of EEG
sequence in which a desired class (left or right hand)
had to be successfully detected. A classifier made a
decision based on EEG sequence of length b
(typically b=1.5-2s, while maximum allowed length
B=3s or 768 samples). However, a classifier could
make a decision based on a portion period called f.
NEUROTECHNIX 2015 - International Congress on Neurotechnology, Electronics and Informatics
18

So if a total sequence for a particular training day is
b=2s, with maximum sequence B=3s and f=75% then
difficulty d is 50%.
5.0
3
75.02
=
⋅
=
⋅
=
s
s
B
fb
d
(2)
On each therapy session a patient performed 30-
40 MA of each hand, separated in sub-sessions
consisting of 20 trials. Each successfully detected
movement attempt resulted in the activation of FES,
as described below. During therapy sessions, patient
sit in front of a computer screen. They were instructed
to attempt a movement upon the appearance of a
visual cue. A feedback in the form of a gauge was
provided to patients. They were told that during MA,
when the gauge indicator reaches 0, there will be
activation of a set of electrodes attached to their hand
muscles in a predefined order. After each 10 trial sub-
session patients got visual information on the screen
about their performance.
2.3.3 Functional Electrical Stimulation
Functional electrical stimulation was delivered using
a multichannel FES device (Rehastim, Hasomed,
Germany). Four bipolar electrodes were attached over
the wrist and hand/thumb extensor and flexor muscles
to assist patients to perform grasp by opening and
closing their hand. The electrodes were attached to
sequentially stimulate the extensor digitorum,
extensor pollicis longus, flexor digitorum
superficialis and flexor policis brevis. The first two
muscles are extensors and the latter two are flexor
muscles. Stimulation of the first two muscles resulted
in opening of the hand and four fingers (index finger
to pinkie), followed by thumb abduction; subsequent
stimulation of two flexor muscles resulted in closing
of the hand. The whole stimulation sequence lasted
10s. Frequency of stimulation was 26 Hz, pulse width
was 200 µs and the current amplitude varied between
15 mA and 35 mA and was individually chosen for
each patient to produce visible muscle contraction
without discomfort. The same setup was used for both
patient groups. The main difference was that BCI-
FES group had to activate FES by attempting to open
and close hand and for FES group stimulator was
activated automatically in 10s on and 10 off sequence.
3 RESULTS
3.1 Attempted Movement ERD/ERS
Average ERD/ERS scalp maps during MA for both
groups were created for θ, α, β1 (12-16 Hz) and β1
(16-24 Hz) bands. A difference in scalp maps before
and after therapy was calculated for each group.
Largest difference were found for BCI-FES group in
β1 for both hands (Fig 2). Both groups had strong
parietally shifted activity before the therapy. Only in
patients, receiving BCI-FES, following the therapy,
the activity ‘restored’, shifting back to the central
cortical region. The lateralisation of ERD during MA
of the left and right hand can also be noticed in Fig
2a,b, column ‘BCI-FES’, row ‘After’. Red dots in
bottom rows in Fig 2a and b show electrodes, located
Figure 2: Event related synchronisation/ desynchronisation
scalp maps for 12-16 Hz, averaged over t=0.5-2s, during
movement attempt in two patient groups before and after 20
therapy sessions. (a) the right hand and (b) the left hand.
Brain-Computer Interface and Functional Electrical Stimulation for Neurorehabilitation of Hand in Sub-acute Tetraplegic Patients -
Functional and Neurological Outcomes
19

in the parietal cortex in BCI-FES group, in which
ERD has significantly changed after the therapy.
Previous studies indicate that parietal shift is due to
an injury (Fig 2a.,b, both groups, row ‘Before’) and
that in patients who functionally recover, cortical
activity shifts back towards the central region (Green
et al. 1998), as in able-bodied people. In BCI-FES
group similar trend could be noticed in all other
frequency bands, being also statistically significant
for the left hand in the α band, and for the right hand
in the θ band. No statistically significant changes
(apart from one electrode showed in Fig 2a, bottom
row) were noticed in FES group.
3.2 Somato-sensory Evoked Potential
Seven patients from BCI-FES and four from BCI
were available for this test. Table 2 shows in how
many patients N20 peak was visible in SSEP of the
medial and ulnar nerve. Results in the table are
presented as pre/post therapy.
Table 2: The number of patients who had visible N20 peak
in their SSEP pre/post therapy in both patent groups.
Median Ulnar
left right left right
BCI/FES 4/6 2/5 1/3 1/2
FES 2/2 1/0 1/1 0/0
In all patients in BCI-FES group, who initially had
visible SSEP, the N20 latency was reduced post-
therapy. The average N20 latency over 7 SSEP in
total was 25.0±3.1 ms pre-therapy and 23.5±2.7ms
post-therapy, being an indicator of neurological
recovery. On the contrary, in FES group, N20 latency
slightly increased from 23.5±1.6 ms to 23.9±1.9 ms.
Figure 3 shows an example of N20 pre and post
therapy in patient 1 who received BCI-FES therapy.
Location of the N20 has shifted towards a lower
latency post therapy and the amplitude (peak to peak)
increased.
3.3 The Range of Motion
Five patients from BCI-FES group and three patients
from FES were available for both initial and final
assessment of ROM of the wrist. All patients in both
groups, except patient 11 from FES group, had the
increased range of motion of wrist following the
therapy (Fig 4). Numerical values of ROM before and
after the therapy, expressed as the degrees of an angle,
are shown separately for flexion and extension of the
right hand wrist. An increase in ROM indicates
functional recovery. Due to the small number of
participants it was not possible to perform a statistical
analysis.
4 DISCUSSION
This study demonstrates the application of BCI-FES
as a rehabilitative device for patients with incomplete
tetraplegia. We used BCI based on time domain
parameters with on-line adaptation (Vidaurre et al.
2009), which allowed short off-line training. Patients
who are still in a hospital and receive standard
treatment, have a very limited time for a BCI-FES
therapy (Rupp 2014). BCI algorithms should
therefore have quick electrode setup and should
require minimum (if any) daily offline adjustment of
parameters. We used 6 electrodes for 3 bipolar
recording, that is much smaller than the number of
electrodes used for algorithms based on common
spatial patterns (16-63 electrodes, Fei et al. 2008, Li
et al. 2014) and comparable with the number of
electrodes for algorithms based on time-frequency
parameters in a selected frequency band (2-12
electrodes, Tam et al. 2011, Mukaino et al. 2014,
Young et al. 2014, Vuckovic et al. 2015).
Due to the injury to the spinal cord rather than to
the brain, most research groups consider BCI-FES to
Figure 3: Somato-sensory evoked potential of the left ulnar
nerve (note N20 peaks between 20 and 30 ms) in patient 1.
be an assistive rather than rehabilitative device for
spinal cord injured patients. This paper, however,
compares neurological and functional outcome of two
hand therapies in incomplete sub-acute tetraplegic
patients. A BCI-FES therapy involved active
participation of patients, resulting in the combined
activation of efferent and afferent pathways while
FES therapy involved passive stimulation of muscles.
0 10 20 30 40 50
-4
-2
0
2
4
6
8
t/ms
Amplitude(micro volts)
Pre
Post
NEUROTECHNIX 2015 - International Congress on Neurotechnology, Electronics and Informatics
20

Previous BCI-FES rehabilitation studies on stroke
patients reported increased ERD, from electrode
located over the sensory-motor cortex, following a
therapy (Li et al. 2014, Mukaino et al. 2014). In a
subset of 4 patients included in this study we noticed
the same phenomena (Osuagwu and Vuckovic 2014).
However the novelty of the current study is that we
looked at scalp maps rather than at isolated
electrodes, which enabled us to notice the spatial
restoration of cortical activity. Before the therapy,
both groups had strong, parietal shift of cortical
activity during MA. Following the therapy, only BCI-
FES group, actively involved in the therapy, restored
centrally located cortical activity during MA. This
trend (parietal activity following injury, shifting
towards central region upon recovery) has been
previously reported in patients with spinal cord
injury, where restoration of cortical activity was
related to functional recovery (Green et al. 1998).
This results is in-line with fMRI single case study
(Mukaino et al. 2014) which showed initial diffuse
blood oxygenation level and lateralisation of this
activity following BCI-FES training.
SSEP was not used in BCI-FES studies in stroke
patients because they had injury to the brain. In SCI
patients however, this is a useful additional indicator
of recovery. In BCI-FES patients group, SSEP
following recovery showed re-appearance of N20
peak and reduced latency of the existing peaks.
Though this was primarily noticed in BCI-FES group,
due to the small number of patients, a statistical
comparison between groups was not performed. Curt
and Dietz (1999) showed a relation between the SSEP
of the lower limbs and the recovery of walking which
could be translated to recovery of the upper limbs.
Improvement in ROM was noticed in both groups.
In summary, while BCI-FES therapy results in a
better neurological recovery, the results of functional
recovery are inconclusive, partially due to the small
number of patients being available for the ROM test.
ROM is a functional assessment also used in studies
on stroke patients (Kim et al. 2015). Studies on stroke
patients additionally used Action Research Arm Test
(ARAT) and Fugl Meyer Assessment of Motor
Recovery to demonstrate better functional
improvements in patients receiving BCI-FES (Li et
al. 2014, Kim et al. 2015). SCI patients in the current
study had more severe motor deficit than stroke
patients and were not initially able to perform any of
these task; therefore individual muscle strength was
measured using MMT test. MMT is not a
straightforward measure as each muscle should be
observed individually, and unlike ARAT and FMA
test, results of individual assessments should not be
Figure 4: The range of motion during flexion and extension
of the right hand wrist before and after therapy for each
single patient in both groups.
summed up over the muscles. This made MMT
analysis complex, beyond the scope of this study.
A neurological recovery normally precedes a
functional recovery. Patients in this study received 20
therapy sessions and had the last assessment shortly
after the last therapy session. It is possible that FES
patients would reach the same level of neurological
recovery as BCI-FES patients but after a prolonged
period of time. Alternatively, BCI-FES group might
Brain-Computer Interface and Functional Electrical Stimulation for Neurorehabilitation of Hand in Sub-acute Tetraplegic Patients -
Functional and Neurological Outcomes
21
have shown long-term larger functional recovery than
FES group due to better neurological recovery. It
would be necessary to follow up patients for a
prolonged period of time (e.g. up to 6 months) to
establish whether those who showed better
neurological recovery would achieve better
functional recovery. Studies on the larger number of
patients are required to establish a clear correlation
between neurological recovery, as measured by the
cortical activity, and functional recovery.
Neurological recovery might potentially prevent
secondary consequences of SCI, such as spasticity
and central neuropathic pain (Pikov, 2002). These
complications are caused by disuse plasticity in the
spinal cord but reflect themselves in the cortical
activity (Wrigley et al. 2009, Vuckovic et al. 2014).
In our recent study, we trained 5 chronic paraplegic
patients with long-standing central neuropathic pain
to voluntary modulate their brain activity over the
sensory-motor cortex (neurofeedback), which
resulted in reduced pain and in some patients in self-
reported reduction of spasticity (Hassan et al. 2015).
In the current study we demonstrated the restoration
of the activity of the sensory-motor cortex as a result
of BCI-FES training. In a long term, this might
prevent secondary consequences of SCI. In the future,
it would be useful having BCI-FES studies with
follow up measures of spasticity and central
neuropathic pain.
5 CONCLUSIONS
The study indicates that BCI-FES therapy of the hand
in sub-acute incomplete tetraplegic patients provides
better neurological recovery than passive FES
therapy. Larger and longer studies are required to
compare functional outcomes of these two therapies
and explore the potential of preventing secondary
complications by early BCI-FES interventions.
ACKNOWLEDGEMENTS
This work has been partially funded by EPSRC PhD
scholarship EP/P505534/1. We would like to thank
Dr Purcell and Dr McLane for their help with
recruiting patients and to all patients for participating
in the study.
REFERENCES
Curt, A., Dietz, V. (1999) Electrophysiological recordings
in patients with spinal cord injury: significance for
predicting outcome. Spinal Cord, 37(3). p.157–165.
Daly, J.J., Cheng, R., Rogers, J., Litinas, K., Hrovat, K.,
Dohring, M. (2009) Feasibility of a new application of
noninvasive brain computer interface (BCI): a case
study of training for recovery of volitional motor
control after stroke. J Neurol Phys Ther, 33(3).p.203–211
Delorme, A., Makeig, S. (2004) EEGLAB: An open source
toolbox for analysis of single-trial EEG dynamics
including independent component analysis. J Neurosci
Meth, 134(1). p.9 – 21.
Fei, M., Kai-yu, T., Suk-tak, C., Wan-wa, W., Ka-him, L.,
Kwok-wing, T., Xiaorong, G., Shangkai, G. (2008)
BCI-FES training system design and implementation
for rehabilitation of stroke patients. In Proc IEEE Int
Joint Conf. Neur Net and World Cong Comp Int. p.
4103-4106.
Fukunaga, K. (1990) Introduction to statistical pattern
recognition. Academic Press, London.
Green, J., Sora, E., Bialy, Y., Ricamato, A., Thatcher, R.
(1998) Cortical sensorimotor reorganization after spinal
cord injury an electroencephalographic study.
Neurology, 50(4),p.1115–1121.
Gugino, V., Chabot, R.J. (1990) Somatosensory evoked
potentials. Int. Anesth. Clin. 28(3).p.154–164.
Hassan, M.A., Fraser, M., Conway, B.A., Allan, D.B.,
Vuckovic, A. (2015) The Mechanism of Neuro-
feedback Training for Treatment of Central
Neuropathic Pain in Paraplegia: A Pilot Study. BMC
Neurology. Accepted DOI:10.1186/s12883-015-0445-7.
Hebb, D. O. (1949) Organisation of behaviour. Wiley, New
York.
Holm, S. (1979) A simple sequentially rejective multiple
test procedure. Scand J Stat, 6(2).p.65–70.
Hyvarinen, A., Oja, E. (2000) Independent component
analysis: algorithms and applications. Neural Networks,
13(4).p.411 – 430.
Jurcak, V., Tsuzuki, D., Dan, I. (2007) 10/20, 10/10, and
10/5 systems revisited: Their validity as relative head-
surface-based positioning systems. NeuroImage,
34(4).p.1600 – 1611.
Kim, T., Kim, S., Lee, B. (2015) Effects of action
observational training plus bran-computer interface-
based functional electrical stimulation of paretic arm
motor recovery in patient with stroke: a randomised
controlled trial. [online] Occup Ther Int, Wiley Online
Library, [Epub ahead of print] DOI:10.1002/oti.1403.
Li,M., Liu, Y., Wu, Y., Liu, S., Jia J., and Zhang, L. (2014)
Neurophysiological substrates of stroke patients with
motor imagery-based brain-computer interface training.
Int J Neurosci, 124(6).p. 403–415.
Marino, R.J., Barros, T., Biering-Sorensen, F., Burns, S.P.,
Donovan, W.H., Graves, D.E., Haak, M., Hudson,
L.M., Priebe, M.M. (2003) ASIA Neurological
Standards Committee 2002. International standards for
neurological classification of spinal cord injury.
The
journal of spinal cord medicine. 26 Suppl 1.p. S50–6.
NEUROTECHNIX 2015 - International Congress on Neurotechnology, Electronics and Informatics
22
McGie, S.C., Zariffa, J., Popovic, M.R., and Nagai, M.K.
(2015) Short-term neuroplastic effects of brain-
controlled and muscle-controlled electrical stimulation.
Neuromodulation: 18(3).p.233-40.
Mukaino,M., Ono, T., Shindo, K., Fujiwara, T., Ota, T.,
Kimura, A., Liu, M., Ushiba, J. (2014) Efficacy of
brain-computer interface-driven neuromuscular
Electrical stimulation for chronic paresis after stroke. J
Rehab Med, 46(4).p. 378–382,
Osuagwu, A.B., Vuckovic, A. (2014) Feasibility of using
time domain parameters as online therapeutic BCI
features. [online] In Proc 6th Int Brain-Computer
Interface Conf, Graz, Austria. DOI:10.3217/978-3-
85125-378-8-58.
Pikov, A. (2002) Spinal Plasticity. In Horch, K.W., Dhillon,
G.S. (Eds) Neuroprosthetics, theory and practice.
World Scientific Publishing, Singapoore.
Pfurtscheller, G., Lopes da Silva, F.H. (1999) Event-related
EEG/MEG synchronization and desynchronization:
Basic principles. Clin Neurophisol. 110(11).p.1842–
1857.
Pfurtscheller, G., Müller, G.R., Pfurtscheller, J., Gerner,
H.J., Rupp, R. (2003) 'Thought'--control of functional
electrical stimulation to restore hand grasp in a patient
with tetraplegia. Neurosci Lett. 351(1).p.33-6.
Porter, S. (2013) Tidy's Physiotherapy. Churchill
Livingstone, Edinburgh.
Rupp, R. (2014) Challenges in clinical applications of brain
computer interfaces in individuals with spinal cord
injury.Front Neuroeng. 24.p.7:38.
Tam, W., Tong, K., Fei, M., Gao, S. (2011) A Minimal Set
of Electrodes for Motor Imagery BCI to Control an
Assistive Device in Chronic Stroke Subjects: A Multi-
Session Study. IEEE Trans Neural Syst Rehabil Eng.
19.p.617-627.
Tan, H.G., Shee, C.Y., Kong, K.H., Guan, C., Ang, W.T.
(2011) EEG controlled neuromuscular electrical
stimulation of the upper limb for stroke patients,” Front
Mech Eng, 6(1).p.71–81.
Vidaurre, C., Kraemer, N., Blankertz, B., Schloegl, A.
(2009) Time domain parameters as a feature for eeg-
based brain-computer interfaces. Neural Networks,
22(9).p.1313–1319.
Vidaurre, C., Sander, T.H., Schlögl, A. (2011) BioSig: the
free and open source software library for biomedical
signal processing. Comput Intell Neurosci.
2011.p.935364.
Vučković, A., Hasan, M.A., Fraser, M., Conway, B.A.,
Nasseroleslami, B., Allan, D.B. (2014) Dynamic
oscillatory signatures of central neuropathic pain in
spinal cord injury. J Pain. 15(6). p. 645-55.
Vuč
ković, A., Wallace, L., Allan, D.B. (2015) Hybrid
brain-computer interface and functional electrical
stimulation for sensorimotor training in participants
with tetraplegia: a proof-of-concept study. J Neurol
Phys Ther. 39(1).p.3-14.
Wrigley, P. J., Press, S.R., Gustin, S.M., Macefield, V.G.,
Gandevia, S. C., Cousins, M.J., Middleton, J.W.,
Henderson, L.A. (2009) Neuropathic pain and primary
somatosensory cortex reorganization following spinal
cord injury. Pain. 141.p.52-9.
Young, B. M
.
, Nigogosyan, Z
.
, Nair, V.A, Walton, L.M
.
,
Song, J., Tyler, M.E., Edwards, D.F., Caldera, K.,
Sattin, J.A, Williams, J.C., Prabhakaran, V. (2014)
Case report: post-stroke interventional BCI
rehabilitation in an individual with preexisting
sensorineural disability. Front Neuroeng. 24.p.7-18.
Brain-Computer Interface and Functional Electrical Stimulation for Neurorehabilitation of Hand in Sub-acute Tetraplegic Patients -
Functional and Neurological Outcomes
23
