
Interoperability Within E-Health Arena
Darko Gvozdanović
1
, Mario Kovač
2
, Hrvoje Mlinarić
2
, Leon Dragić
2
, Igor Piljić
2
,
Petar Franček
2
, Martin Žagar
2
and Vlado Sruk
2
1
Ericsson Nikola Tesla d.d. Krapinska 45, Zagreb, Croatia
2
Faculty of Electrical Enginnering and Computing, Unska 3, Zagreb, Croatia
darko.gvozdanovic@ericsson.com, mario.kovac@fer.hr; hrvoje.mlinaric@fer.hr; leon.dragic@fer.hr; igor.piljic@fer.hr;
petar.francek@fer.hr; martin.zagar@fer.hr; vlado.sruk@fer.hr
Keywords: Personal Healthcare Record, Continuity of Care Document CCD, Electronic Healthcare Record (EHR),
Electronic Medical Record (EMR), Interoperability, Information systems in healthcare
Abstract: Integrated care approach and the broader view on a patient’s care is something that today’s healthcare
systems thrive for. Medical information collected from many disparate sources, accessed by authorized
users through Electronic healthcare record (EHR) is enabling technology behind. This article gives
overview of different interoperability aspects related to data exchange and maps it to usual healthcare
business processes. It also comments HL7 CDA being one of today’s widely used standards for clinical
documents exchange. One concrete approach to Personal Healthcare Record (PHR) to EHR integration
using HL7 Continuity of Care Document (CCD) is described.
1 INTRODUCTION
The fact that ICT systems can bring a lot of benefits
to all stakeholders within healthcare system is well
known (Dobrev, 2009). However, successful
implementation and proper introduction of such ICT
systems in existing healthcare environment is long
and expensive process. Many countries can’t
increase efficiency in healthcare sector through ICT
system introduction. One of three main reasons for
this is lack of commonly defined and consistently
implemented standards (OECD 2010). Without
common standards, one of the biggest advantages
introduced by ICT systems in healthcare, which is
access to comprehensive and high quality patient
medical information in any time or place, remains
unsolvable puzzle. Due to the fact that medical data
originates from many disparate sources, efficient
sharing across organizations, administrative domains
or even countries is of utmost importance.
Interoperability of implemented ICT systems plays
vital role in achieving this goal.
Stroetmann et al. (2009) defined interoperability
in healthcare context “as the ability, facilitated by
ICT applications and systems: to exchange,
understand and act on citizens/patients and other
health-related information and knowledge; among
linguistically and culturally disparate health
professionals, patients and other actors and
organizations; within and across health system
jurisdictions in a collaborative manner.”
In order to meet these requirements, all
interoperability aspects, namely legal,
organizational, technical (eHealth Governance
Initiative, 2010) and semantic (EN13606
Association, 2015) must be addressed (Kovac,
2014). A real life interoperability issues are showed
in the example that follows.
Ana is a 22 years old female without any chronic
disease. On January 23rd she woke up and felt pain
in right side of abdomen. She decided to book an
appointment with Dr. Henry Levin, her general
physician through the patient portal.
On the date of the scheduled appointment Ana
went to the polyclinic to see Dr. Levin. Admission
81
GVOZDANOVIC D., Kovac M., Mlinaric H., DragiÄ
˘
G L., PiljiÄ
˘
G I., FranÄ ek P., Å¡agar M. and Sruk V.
Interoperability Within E-Health Arena.
DOI: 10.5220/0005889800810086
In Proceedings of the Fourth International Conference on Telecommunications and Remote Sensing (ICTRS 2015), pages 81-86
ISBN: 978-989-758-152-6
Copyright
c
2015 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

office staff (AO staff) checked if there were any
previous visits of Ana in the system using her
identity card. AO staff found general data about her
in the system (from her previous visits to the same
polyclinic.
Since Ana had set access right level for her
medical data to “ask patient consent each time”
through the patient portal, AO staff couldn’t access
medical data and asked Ana to provide consent. Ana
refused to provide a consent and signed the
document stating that only dr. Levin can access her
medical data.
Dr. Levin was logged in to his Hospital
Information System (HIS) and chose to review
Ana’s electronic medical record (EMR). He decided
to check her physical status immediately, opened a
new case in the system and invited Ana to step into
his office.
Even before physician saw the patient, number of
interoperability issues had emerged. The first one
was legal - who is the owner of medical information:
patient or the physician who generated it; how the
access rights are managed; can patient choose which
part of medical record will be accessible to medical
staff. The second issue is of organizational nature.
Healthcare institution might have one central
reception, one reception per clinic or completely
distributed one. Reception process might be
completely administrative where no medical
information is needed or it can include triage, taking
anamnesis and status in which case access to
previous medical information is mandatory.
Dr. Levin noted Ana’s anamnesis, physical status
and result of his observation in the system and
issued several requests for laboratory tests and
additional consultations from the surgeon and
gynecologist.
Unless Dr. Levin understands the data within
Ana’s electronic medical record (EMR) in the same
way that all those users who put information into
EMR have wanted, the whole concept of EMR is
missed. Having information in free text form is
definitely better than having nothing but medical
data stored in a structured format can be used for
automatic alerting on drug-drug interactions,
provision of drug-diagnose contraindications,
automatic suggestion of applicable clinical practice
guidelines (CPG), automatic reporting, reducing
administrative work etc. How clinical documents are
structured, what coding systems are used, whether
the same or different codes for the same notions are
used, are only part of semantic interoperability
aspect than needs to be taken care of.
Laboratory order was available through the
Laboratory Information System (LIS) at the same
moment Dr. Levin sent it through HIS.
Since completely new information system (LIS)
appeared in storyboard, technical interoperability
issue emerged. Legal aspect returned and became
even harder to address since laboratory personnel
actually did have Ana in their care but never met
her. Ana didn’t give consent to all personnel within
hospital to access her medical record so important
information that might affect laboratory results was
not available for laboratory staff. Since physician
and laboratory technician / biochemistry engineer
were of different specializations and were using
different applications, there must not be any
misunderstanding of what test were requested and
what results were sent back. Did all healthcare
professionals use same coding list or at least some
mapping engine (terminology server) existed?
The storyboard ends here since majority of
interoperability issue types within one healthcare
institution were already mentioned although only
three steps were exercised: admission, first
examination, and referral to laboratory/consultation.
In practice, stakeholders within same institution can
efficiently share data because they use the same
application or some proprietary integration is done if
multiple applications exist. But if Ana were urgently
referred to another hospital because of suspected
acute appendicitis she would be admitted to the
hospital with different internal processes, different
specialization and HIS from another vendor. These
two healthcare institutions were connected only
through national infrastructure if it existed. This
means that if integrated care is to be supported,
proprietary integration that is possible within one
institution has to be properly handled through
solving all the interoperability issues mentioned
above.
2 E-HEALTH BLOCKS
2.1 Electronic Medical Record
While introducing ICT into the healthcare
institutions, system Purchasers (not the users
themselves) often prioritize administrative over
medical processes. True value of information
systems / applications in healthcare provision
processes is proper management of medical
information. Therefore medical documentation
module should be the core of every application
within general practitioner and specialist practice
Fourth International Conference on Telecommunications and Remote Sensing
82

application or hospital information system. This core
component is called electronic medical record
(EMR). In simple terms, EMR is a digital version of
the paper charts in clinician offices, clinics, and
hospitals (Health information technology, 2015).
Market today witnesses thousands of EMR systems.
Unfortunately lack of standards led to the situation
where most of them are implemented on different
information models that are followed by the
completely different graphical user interfaces,
different ways how data entry is supported and
completely different application logic.
2.2 Electronic Healthcare Record
Today’s healthcare challenges are numerous and
there is myriad of ways how healthcare authorities
try to address them. One important tendency in
coping with these issues is shift towards so called
integrated care. The core of such an approach is
broader view on a patient’s care. This requires
boundaries among multiple EMR’s to vanish and
much more data about the patient made accessible
than it is collected in any single healthcare
provider’s office. The solution for this is electronic
healthcare record (EHR).
EHR contains information generated by all the
clinicians involved in a patient’s care process, with
all these clinicians having also access to it. EHR also
shares information with other health care providers,
such as laboratories and pharmacies. EHR should be
pervasive and follow patients – to the specialist, the
hospital, pharmacy, the nursing home, within or out
of the country (Health information technology,
2015). Secondary use of information stored in EHR,
namely education, research, public health needs etc.
is as equally important as its primary continuity of
care purpose.
2.3 Personal Healthcare Record
The implementation of different eHealth services
brings numerous benefits to the patients even when
they do not use the service directly. Example is any
service that saves time for the physician, allowing
him to spend more time with patients. Nevertheless,
final touch on the national eHealth system would be
direct patient empowerment where patient portals
and personal health records (PHR) play vital role.
Personal health records contain the same types of
information as EHR – diagnoses, medications,
immunizations, family medical histories, and
provider contact information, but are designed to be
set up, accessed, and managed by patients. Patients
can use PHR to maintain and manage their health
information in a private, secure, and confidential
environment. PHR can include information from a
variety of sources including clinicians, home
monitoring devices, and patients themselves (Health
information technology, 2015).
3 STANDARDIZATION
In order to efficiently use medical information
throughout healthcare system, it has to be stored and
exchanged in a standardized way. EMR, EHR and
PHR in their essence are about documenting
different facts. If document is intended for personal
use only, than words, grammar and rules are not so
important. But if document is intended for use by
other persons, all of this must be well defined and
collectively accepted. Otherwise, document will be
at least partly incomprehensible or what is even
worse wrongly understood. In the world of semantic
interoperability notion grammar refers to reference
model, words/dictionary are codes/coding system
and phrases/rules are clinical models, archetypes or
templates.
In that sense openEHR and HL7 Clinical
Document Architecture (CDA) are two of the most
promising standards for storing clinical information
and medical documents exchange respectively.
Integrating the Healthcare Enterprise (IHE) initiative
is the most prominent way to achieve out-of-the-box
interoperability at least in specific use cases.
3.1 HL7 CDA
The HL7 CDA is a document markup standard that
specifies the structure and semantics of "clinical
documents" for the purpose of exchange. A clinical
document is a documentation of clinical
observations and services, with the following
characteristics: persistence, stewardship, potential
for authentication, context, wholeness and human
readability. A CDA document is defined as a
complete information object that can include text,
images, sounds, and other multimedia content.
HL7 CDA standard proved to be too generic. In
order to refine it, content templates are introduced.
One of the most widely known content templates is
Continuity of Care Document (CCD). CCD is
specification on how to constraint HL7 CDA in
accordance with requirements set forward in
Standard Specification for Continuity of Care
Record (CCR). The CCR is a core data set of the
most relevant administrative, demographic, and
Interoperability Within E-Health Arena
83
clinical information facts about a patient's
healthcare, covering one or more healthcare
encounters (Health Level Seven International, 2007).
It provides a means for one healthcare practitioner,
system, or setting to aggregate all of the pertinent
data about a patient and forward it to another
practitioner, system, or setting to support the
continuity of care. The primary use case for the CCR
is to provide a snapshot in time containing the
pertinent clinical, demographic, and administrative
data for a specific patient.
Although templates obviously refine underlying
standards, one obvious weakness emerges – too
many different templates defined by different
organizations/vendors/health authorities. Even after
content is defined with content standard and refined
and constrained with standard templates,
overlapping terminologies issue remains. Very
representative example is HL7 CDA representation
of observation of 108 mg/dL glucose in the plasma
of a patient, which is measured in a laboratory
setting. There are more alternatives how to
exchange this fact within CCD document.
Alternative 1 is that plasma glucose
measurement procedure is exercised (SNOMED CT
code 119958019) and there was an observation of
blood glucose status (SNOMED CT code
405176005), with the actual observed value, which
is 108 mg/dL glucose. Alternative 2 is that
laboratory test procedure is exercised (SNOMED
CT code 15220000), and there was an observation of
glucose in serum or plasma (LOINC code 2345-7),
with the actual observed value, which is 108 mg/dL
glucose.
Although different coding systems and different
structure is used, the same medical information is
represented and communicated in both instances. So
in spite of the fact that communicating applications
are capable of using CCD template, interoperability
is achieved only partially. When different
terminology systems are used in the same structure,
it is necessary to semantically mediate them for
interoperation. Some of the repositories with
mapping information are Unified Medical Language
System (UMLS) and Metathesaurus and BioPortal.
There are examples of successful eHealth
systems that do not use international terminologies.
National information system in Croatia (CEZIH)
does not use nor SNOMED CT or LOINC. Local
coding systems are defined by professional
associations. Since there is national consensus about
coding lists used, interoperability on national level is
achieved and Croatian eHealth system is perceived
as one of the best in Europe.
4 INTEROPERABILITY
The practical approach to solving interoperability
problem is one of the goals of project “Information
and communication technology for generic and
energy-efficient communication solutions with
application in e-/m-health” (ICTGEN). In scope of
this project we will demonstrate integration of PHR
with EHR using HL7 Continuity of Care Document
(CCD). Simulation environment, consisting of PHR
and EHR, was created at Faculty of Electrical
Engineering and Computing. As an EHR system
openEMR solution based on openEHR reference
model is hosted and adapted to specific needs of the
ICTGEN project. Project partner, Ericsson Nikola
Tesla d.d. provided their own solution for PHR,
Ericsson Mobile Health (EMH).
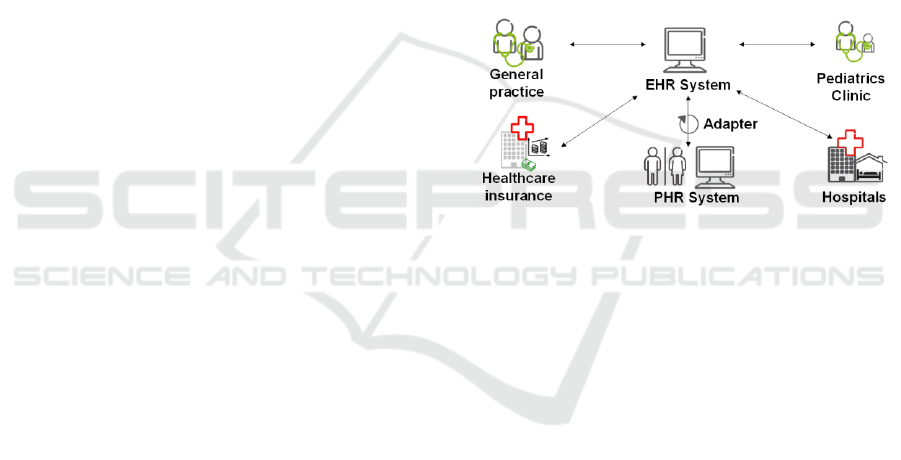
Figure 1: EHR-PHR integration within ICTGEN project.
EMH is one of the numerous PHR solutions
offered on the market and its focus is on managing
patient's record. Depending on the role, users can
access and manage their medical data. EMH
provides external access to specific data through
Medical Node (MN) API in custom format. Without
standardized format of data exchange, integration
with any other ICT solution requires system
modifications or additional integration components.
First step to solving this interoperability issue
was thorough analysis of exchanged medical data
format and HL7 Continuity of Care Document
(Health Level Seven International, 2007). The
analysis lead to classification of medical data into
matching categories which were mapped to
corresponding CCD elements in the next step. This
mapping model was implemented as an adapter
component connected to MN API. Since lot of data
from PHR is not suitable for EHR, only EHR to
PHR communication is implemented. After PHR
client is authenticated and authorized for data
access, adapter on PHR side receives data from EHR
Fourth International Conference on Telecommunications and Remote Sensing
84

formatted as CCD document. That allows multiple
PHR solutions capable of importing CCD to be
integrated with EHR. In this project, specific adapter
is built and information from CCD document is
extracted and stored within EMH database. In that
sense EMH is upgraded into interoperable PHR
solution capable of importing patient summaries in
CCD format presumed limited subset of medical
information is exchanged. Although this might seem
like unacceptable limitation it is in fact the only
realistic way to achieve interoperability. With more
than 600.000 concepts within SNOMED CT, it
would be illusion to build application that can
interpret any of these in the right context. Our
approach is to start small and expand adapter
making it capable to process more medical
information.
5 CONCLUSION
Retrieving all relevant information, utilizing other
experiences, exercising team work and looking on
things from different perspectives are all aspects of
providing high quality healthcare service.
Communication is foundation for all of this. The
necessary precondition however, is that sender and
receiver of information are capable of exchanging it
and understanding it in the same way. This is the
essence of interoperability. Healthcare, being one of
the most complex human domains, poses similarly
complex interoperability issues. It actually requires
from the participants speaking different complex
languages to use one common grammar, words from
the same dictionary, to use same phrases or to find
one translator that knows all the languages. Neither
of this is realistic, especially in short term. Therefore
different healthcare interoperability standards and
initiatives are introduced but for the time being
solution is far away. HL7 CDA without templates is
too generic to assure true interoperability. It only
allows that clinical documents can be exchanged
with appropriate amount of metadata. What’s within
these documents is not so important to this standard.
Templates and constraints narrow this uncertainty a
little bit. But even with CCD as one template, same
thing can still be expressed in more than one way
which makes it very hard for applications to
communicate among each other. Nevertheless,
ICTGEN project, confirmed that for well-defined
subsets, medical information can be efficiently
exchanged between different applications like EHR
and PHR.
But the main interoperability issue as we see it, is
the fact that healthcare professionals does not use
same dictionaries (or terminologies / coding list),
nor they use the same words (codes) for same
events. SNOMED CT as maybe the most
comprehensive terminology today is not available in
all languages. Mappings to other terminologies are
not available at all or are not complete. Process of
introducing terminology like SNOMED CT into
healthcare system of one country is very long and
expensive. Still it does not guarantee that same event
will be described with the same code by different
healthcare professionals. Until this is solved, no
structure, no clinical document definition, no
knowledge model (archetype) will bring true
interoperability.
The research leading to these results has received
funding from the project "Information and
communication technology for generic and energy-
efficient communication solutions with application
in e-/m-health (ICTGEN)" and co-financed by the
European Union from the European Regional
Development Fund and from project “Carewell”
funded by the European Commission within the ICT
Policy Support Programme of the Competitiveness
and Innovation Framework Programme (CIP).
REFERENCES
Chute, C.G., 2000. Clinical classification and terminology:
some history and current observations. J Am Med
Inform Assoc 7, 298–303.
Dobrev, A. and Jones, T. (2009) Report on The socio-
economic impact of interoperable electronic health
record (EHR) and ePrescribing systems in Europe and
beyond – Final study report. Retrieved from:
http://www.ehr-impact.eu/downloads/reports.html
eHealth Governance Initiative – eHGI (2012), Discussion
paper on semantic and technical interoperability
Retrieved from: http://ec.europa.eu/health/ehealth/
docs/ev_20121107_wd02_en.pdf
EN13606 Association, Semantic interoperability of health
information. Retrieved June 9, 2015 from:
http://www.en13606.org/the-ceniso-en13606-
standard/semantic-interoperability
Health information technology (health IT), Retrieved June
9, 2015 from: http://www.healthit.gov
Health Level Seven International (2007), HL7
Implementation Guide: CDA Release 2 – Continuity
of Care Document (CCD). Retrieved June 10, 2015
from: http://www.hl7.org/implement/standards/
product_brief.cfm?product_id=6
Kovac, M. 2014. E-Health Demystified: An E-
Government Showcase. Computer 47, 34–42.
doi:10.1109/MC.2014.282
Interoperability Within E-Health Arena
85

OECD, 2010. Improving Health Sector Efficiency.
Organisation for Economic Co-operation and
Development, Paris.
Stroetmann, V.N.; Kalra, D.; Lewalle, P.; Rodrigues, J.M.;
Stroetmann, K. A.; Surjan, G.; Ustun, B.; Virtanen,
M.; Zanstra, P. E (2009). Semantic Interoperability for
Better Health and Safer Healthcare: Research and
Development Roadmap for Europe: SemanticHEALTH
Report. Retrieved from:
http://www.empirica.com/publikationen/2009_en.htm
The Authoritative Dictionary of IEEE Standards Terms,
Seventh Edition, 2000. . IEEE Std 100-2000 -.
doi:10.1109/IEEESTD.2000.322230
Fourth International Conference on Telecommunications and Remote Sensing
86
