
Overnight Supervision of Alzheimer’s Disease Patients
in Nursing Homes
System Development and Field Trial
Laura Montanini
1
, Laura Raffaeli
1
, Adelmo De Santis
1
, Antonio Del Campo
1
, Carlos Chiatti
2
,
Giorgio Rascioni
3
, Ennio Gambi
1
and Susanna Spinsante
1
1
Information Engineering Department, Universit
`
a Politecnica delle Marche, Ancona, Italy
2
Italian National Research Centre on Ageing (INRCA), Ancona, Italy
3
ArieLAB S.r.l., Ancona, Italy
Keywords:
Environmental Sensors, Unobtrusive Monitoring, Activity Detection, Alarm Notification, Behavioural
Analysis.
Abstract:
The number of patients affected by Alzheimer’s disease among the population is currently growing, while
the availability of resources for their assistance is decreasing. A solution for this problem is provided by
the use of Ambient Assisted Living technologies, with the objectives to prolong the independent living of
patients at home, to relieve assistance burden on caregivers, and to improve care effectiveness in nursing
homes. This paper describes an integrated system designed to support the work of nurses during the night, to
ensure comfort and safety of Alzheimer’s disease patients in nursing homes. The project started from a similar
solution designed for home use, suitably re-engineered for adoption in nursing homes. The system has been
designed according to nurses’ requirements and expectations, both by revising some existing functionalities,
and by developing new components. The results gained from an experimental trial are also presented and
discussed.
1 INTRODUCTION
Staff working in care and nursing homes typically ex-
periences a high workload, due to the need of carry-
ing out a lot of tasks in a relatively short period of
time. Usually, this happens because of budgetary re-
strictions on the amount of personnel recruited, with
respect to the number of patients cared after. In
fact, since 2010, due to the global economic cri-
sis, growth in public health spending came almost
to a halt across the OECD (Organisation for Eco-
nomic Cooperation and Development), with even re-
ductions in many countries. Since then, the spending
growth has been very slow, often in line with over-
all economic growth (Organization for Economic Co-
operation and Development, 2015). Despite the cur-
rent trend of moving long-term care out of institu-
tions into patients’ home premises, the role of nurs-
ing homes remains relevant, especially for those pa-
tients affected by chronic diseases, like dementia or
Alzheimer’s disease (AD), who cannot be assisted at
home. Information and Communication Technolo-
gies (ICT) should be exploited to improve the work-
ing conditions of the care staff, and to improve the
quality of care. Experiences showed that the impact
of technology on underlying clinical work processes
should be carefully evaluated and analysed. Possible
blocks in the execution of routine procedures due to
the adoption of technology tend to distract staff from
care issues, and can result in new errors. Typically,
in reaction to this condition, nurses develop problem-
solving behaviours that involve bypassing new tech-
nology, or adapting work process so as to minimize
disruption in operational procedures (Bowens et al.,
2010; Lowry et al., 2015; Huston, 2013).
Several ICT-based solutions have been proposed
to facilitate home-caring of people affected by de-
mentia or AD during the night hours. In fact, night-
time activity is a common occurrence in persons with
dementia, which increases the risk for injury and unat-
tended home exits, and impairs the sleep patterns of
caregivers (Lee et al., 2014; Kim et al., 2014). Tech-
nology has been applied to develop tools that alert
caregivers of suspicious nighttime activity, to help
Montanini, L., Raffaeli, L., Santis, A., Campo, A., Chiatti, C., Rascioni, G., Gambi, E. and Spinsante, S.
Overnight Supervision of Alzheimer’s Disease Patients in Nursing Homes - System Development and Field Trial.
In Proceedings of the International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2016), pages 15-25
ISBN: 978-989-758-180-9
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
15

prevent injuries and unattended exits (Occhiuzzi et al.,
2014; Mao et al., 2015; Vuong et al., 2013). Night-
time attendance of patients affected by dementia or
AD may be difficult to manage also in nursing homes,
especially because the number of nurses available is
reduced, with respect to daily hours. As a conse-
quence, it is of interest to evaluate the applicability
of technology for night monitoring of AD patients in
nursing homes, in order to assess the impact of tech-
nology on nurses’ work flows, and on the quality of
assistance provided to patients.
This paper describes an integrated system for the
monitoring of AD patients, realized by evolving and
updating an already existing product named UpTech
(Chiatti et al., 2013). The UpTech project focused
on AD patients and their family caregivers; it was
carried out as a multi-component randomized clini-
cal trial (RCT), integrating previous evidence on the
effectiveness of AD care strategies, in a comprehen-
sive design, to reduce the burden of family caregivers
of AD patients, and to maintain AD patients at home.
Indeed, often the relatives who take care of AD pa-
tients are subjected to high levels of stress, that could
also contribute to the onset of physical problems. The
positive outcomes of the UpTech experimental phase
(Pombo et al., 2015), providing the use of technolog-
ical devices as alternative or complementary form of
support, have suggested its application in a different
scenario, represented by the nursing homes. The aim
of the UpTech RSA project is to support and help as-
sistance of AD patients in nursing homes, during the
night hours, by means of a set of sensors located in
patient’s room, and suitable software applications to
detect dangerous events and raise alerts for the nurses.
When dealing with monitoring of people, this con-
dition is often seen as violating the privacy of the
user. Therefore, in order to satisfy the requirement
of providing an unobtrusive monitoring, only simple
environmental sensors have been employed in the Up-
Tech RSA solution, that are less intrusive and more
acceptable than other options, like wearable devices,
or video cameras. Wireless sensors have been chosen
and used: on one hand, this enables a simple installa-
tion, on the other hand, power consumption is a crit-
ical aspect, which has to be evaluated at the design
stage.
The paper is organized as follows: the context of
application of the proposed technology is discussed
in Section 2, whereas Section 3 is focused on design
and deployment issues. The field trial implementa-
tion is presented in Section 4, and the results gath-
ered from the practical use of the technology in a
real nursing home are discussed in Section 5, show-
ing how the data collected from sensors may be trans-
lated into useful information for understanding the
patients’ needs and requirements. Finally, Section 6
concludes the paper and suggests possible future de-
velopments.
2 CONTEXT
Dementia is becoming increasingly prevalent world-
wide and is today considered as one of the
most burdensome disease for the western societies.
Alzheimer’s Disease is the most common form of de-
generative dementia. Generally, the onset of the ill-
ness occurs in the pre-senile age, however it could be
even earlier. A person with dementia can live 20 years
or more after diagnosis, during which he/she experi-
ence a gradual change of the functional and clinical
profile. As consequence of the disease, a progres-
sive loss of cognitive capacity is occurring, eventually
leading to disability and to a severe deterioration of
quality of life. During the so-called “dementia jour-
ney”, the disease affects not only the patients but also
their informal (e.g. families) and formal (e.g. care
staff) caregivers, on whom the bulk of the care burden
falls (Chiatti et al., 2015).
Up-to-date, there is no cure for dementia thus
the attention to the symptomatic non-pharmacological
treatment for the patients and their caregivers has be-
come increasingly relevant, especially as the litera-
ture shows that these can be more effective that most
of available drugs (Spijker et al., 2008). Although
home remains the preferred place for care delivery,
a substantial number of patients need to access (per-
manently or temporarily) to residential care facilities,
when home care is no longer feasible. In the resi-
dential context, infrastructure and staffing levels are
not always adequate to manage residents with demen-
tia. Residential care services are indeed labour inten-
sive and the quality of care here depends largely on
the staffing level and characteristics (Kahanp
¨
a
¨
a et al.,
2016; Milte et al., 2016). As the ongoing financial
crisis is reducing the budget available for residential
care services, a detrimental effect on personnel stan-
dards might occur. This concrete risk of staff short-
comings might, in turn, lead to a substantial propor-
tion of avoidable hospitalisations, use of emergency
departments, icreased carers’ burden and stress, and
inappropriate use of chemical and physical restraints
(e.g. antipsychotics).
The literature suggests that education, training and
support of available staff, supervision, improvement
of job satisfaction could be effective measures to in-
crease quality of care in this care setting (Institute of
Medicine, 1986). In addition, technologies and other
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
16

environmental factors have been identified as the most
promising measures to improve working conditions
in the residential care setting, to reduce the care bur-
den and to improve the overall quality of care (Freed-
man, 2005; Ancker et al., 2015). The potentials of
new technologies have been tested to reduce the need
for constant monitoring of dementia patients, increase
their safety and wellbeing within the residential set-
ting. So far, however, few solutions have manage to
survive to the prototyping phase and have been con-
cretely exploited in the market.
3 DESIGN AND DEPLOYMENT
The system described in this paper represents an evo-
lution of a project named UpTech, aimed at improv-
ing the quality of life of both AD patients living at
home and their family caregivers. This project in-
volved nurses and social workers, who periodically
went to the patients’ houses, and the installation of
technological kits. Each kit consisted of a network of
wireless sensors installed in the house, for the moni-
toring of the patient. Data were processed by a central
control unit and, in case of danger, a notification was
sent to the caregiver. The new system, called UpTech
RSA, targets the nursing home environment and has
been devised primarily for the overnight monitoring
of patients, when there is a lack of personnel in the
building. Moreover, the main differences between the
two systems concern:
• number of users: in the nursing home, multiple
patients are monitored at the same time. Thus, the
central control unit is able to manage data coming
from more than one set of sensors;
• sensors: different types of sensors are employed,
due to the diversity of the physical environment;
• system architecture: the whole network can be
seen as a set of sub-networks, one for each room;
• alarm management: the monitoring system is an
aid for the nurses, the notifications are not sent to
the remote caregiver as in the previous system.
The project development stage conducted in the
Laboratory was aimed first at the improvement of the
previous UpTech kit, secondly at the design and im-
plementation of the modules required for the new sys-
tem. In particular, the radio transceivers firmware was
re-designed, to implement an efficient data acquisi-
tion and transmission procedure. At the same time,
particular attention was paid to the energy consump-
tion exhibited by the transmission nodes, by taking
into account the values of power absorption in the dif-
ferent operation phases, and implementing all the pos-
sible strategies for its reduction. As for the new com-
ponents, the following modules have been designed:
the structure of the database used to store the collected
information, and the applications necessary to imple-
ment the decision algorithms, in charge of making ac-
tions depending on particular values of the acquired
data.
The system requirements have been identified by
collecting nurses’ requests, thus the developed func-
tionalities are related to the usual daily care proce-
dures. Specifically, the set of sensors installed in each
room enables the following functionalities:
• door opening detection;
• window opening detection;
• “French-window” opening detection;
• presence in bed detection;
• presence in the bathroom detection.
The door opening detection is achieved using a mag-
netic sensor, wireless connected by Sub-GHz tech-
nology at a frequency of 868 MHz to a gateway, by
means of a properly designed electronic equipment.
Figure 1: Magnetic sensors for windows opening detection.
Figure 2: Self-calibrating mat sensor, for under-the-
mattress positioning.
Similarly, the detection of windows opening is
made through the same technology (see Figure 1).
The user’s presence in the bathroom is detected by a
self-powered Passive Infrared Sensor (PIR), which is
connected to the radio transmitter module. For ease
of installation, and to avoid damage to the fixtures
of the building, these sensors have been placed on
top of the entry doors of the bathrooms. A mat sen-
sor has been adopted to detect the user’s presence in
Overnight Supervision of Alzheimer’s Disease Patients in Nursing Homes - System Development and Field Trial
17

bed; it is available in two versions, with and without
self-calibration. The sensor without self-calibration is
placed over the mattress, under the sheets, while the
other one is placed under the mattress (Figure 2), and
therefore it appears more comfortable for the patients
and for the daily operations of bed maintenance. The
gateway represents a central node that forwards data
to a PC located at the nurses’ station. Then, the ap-
plication running on the PC filters the incoming in-
formation. Data related to events are saved in a local
database (DB), while those referred to the operating
status of the sensors are verified in order to monitor
the correct operation of the technology kits.
The electronic boards transmit an event to the cen-
tral server every time there is a status change, that is,
for example, activation/deactivation of the PIR sensor,
or opening/closing the door. Accordingly, the data
stored in the database contain the sensor information
(id, gateway address, name and type), the date and
time when the notified event occurred, and the status
of the sensor represented in binary format as follows:
• activation: state = 1;
• deactivation: state = 0.
In addition, the server assigns a unique id to each
DB row in order to implement a robust mechanism
for transmitting information to the mobile interface.
This allows the mobile device to identify one or more
missing events, and to request them back from the
server. In fact, a mobile Android application has been
developed, running on a tablet or smartphone, and so
easily portable. This allows the nursing staff to re-
ceive event notifications even when they are outside
the nurses’ station and cannot access the fixed desk-
top interface. Events data, properly processed, are
displayed through not only mobile, but also desktop
interfaces (Figures 3 and 4). In the first case, the
user can see a scrollable list of events identified by
the name of the sensor that generated it and the room
Figure 3: Mobile interface running on a smartphone.
Figure 4: Screenshot of the Desktop Interface, two sections
version.
name, as shown in Figure 3. Each event is tagged with
a colored circle: depending on the associated level of
alert, the circle may be green, yellow or red. In the
latter case, two versions are available:
• a two sections version: the interface is divided
into two parts. On the right there is a scrollable
list of the events acquired by the sensors, while
on the left the status of the sensors in each room
is shown. There is a top bar which becomes
coloured and flashing when an event occurs;
• a multi-user version: the main screen shows all
the rooms monitored. When an event occurs in
one room, the corresponding frame becomes col-
ored. By clicking on the box, it is possible to see
the details of sensors state.
Given the wireless transmission mode of the sen-
sor nodes and their battery supply, the monitoring
of the sensors state itself becomes very important.
Therefore, a procedure for the periodic sending of
alive messages has been implemented in the sensors.
They are constantly monitored by the central process-
ing system, that generates alarm messages in the case
of failure. Despite its importance, this procedure is
extremely critical, because sending alive messages
too frequently causes an increase in the batteries con-
sumption. Otherwise, the transmission of the alive
message at a lower frequency can give rise to long
time intervals in which the sensor is not active, but
the system is not informed about the failure. When
an alive message does not reach the local server at the
expected time, the latter notifies a malfunction of the
sensor node to the nurse, who can promptly find out
the problem and act accordingly.
4 FIELD TRIAL
4.1 Experimental Set-up
The system described in Section 3 is already avail-
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
18
able as a prototype. Following the initial develop-
ment phase in the Laboratory, aimed to better adapt
the technology to the emerged operational require-
ments, the prototype has been installed in the nursing
home “Villa Cozza” in Macerata (Italy). In this phase,
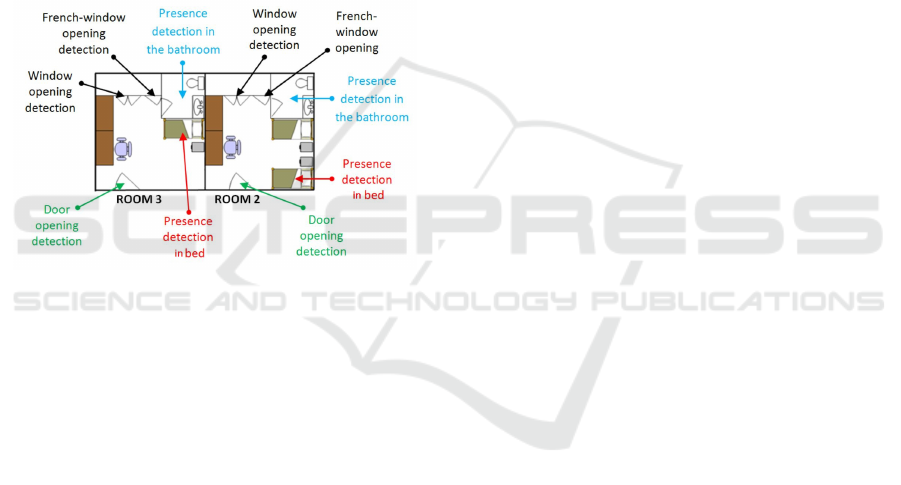
the supervision of two rooms (tagged as room 2 and
room 3) has been implemented, while the final ver-
sion of the system will be able to dynamically accept
a plurality of rooms, depending on the operating re-
quirements. Each room is equipped with a sensors kit
consisting of three magnetic sensors (one applied onto
the window, one onto the French window, and one
onto the room front door), a PIR sensor in the bath-
room, and a force sensor placed in the bed, as shown
in Figure 5. A single gateway device has been used to
manage wireless communications with the sensors in
the two rooms.
Figure 5: Floor plan of the two rooms equipped with the
UpTech RSA sensors in the nursing home “Villa Cozza”,
Macerata (Italy).
In room 2 two female patients are housed, only
one suffering from Alzheimer’s disease. Her bed has
been equipped with a force sensor. The other one is
not autonomous and can move only by a wheelchair;
consequently, the events generated by the different
sensors can be originated only by the movement of the
first patient. In room 3, instead, a single female pa-
tient is housed, also suffering from Alzheimer’s dis-
ease, but in this case she can not move autonomously.
As the system represents a support tool for improv-
ing the safety of patients, it can be well-compared to
an alarm system. Moreover, the type of sensors em-
ployed do not collect personal data of the two patients
involved. According to the national laws, in this case
the ethical approval is not required.
A critical issue encountered during the installa-
tion phase has been to enable the communication be-
tween the gateway, positioned in the corridor in front
of the two rooms, and the central server, located in
the nurses’ station on the upper floor. Such a problem
arises because the building where the nursing home
is located is not equipped with a communication in-
frastructure (e.g. a Local Area Network): there are
no network cables, or WiFi coverage. Moreover, the
nursing home is hosted in a historic building and, as
often happens in such cases, the walls are thick and
made of concrete, thus making wireless communica-
tions very difficult. Both a Power Line Communica-
tion (PLC) and a mixed wireless infrastructure (WiFi
and Hiperlan) have been experimented, finally select-
ing the wireless solution as the supporting commu-
nication architecture. In order to overcome obsta-
cles like metal doors and thick walls, that limit signal
propagation, multiple Access Points (APs) and links
have been setup.
4.2 Evaluation Survey
Some weeks after the installation a survey for the
evaluation of the system has been conducted over 18
nurses. Although some of them are not very familiar
with the technology, the results are highly positive. In
Table 1, some of the most significant questions and
results are listed. The 100% of respondents believes
the kit is easy to use and recommends it for the mon-
itoring of AD patients in nursing homes during the
night. All the nurses state the system has not been
a source of stress for them. In fact, its introduction
does not generate further work for the staff. They just
carried on the usual activities, but with an additional
monitoring tool. Only the 6% of nurses believes that
it was stressful for patients. Indeed, operators have re-
ceived some sporadic grumbles due to the discomfort
produced by one of the bed sensors. As mentioned
in Section 2, the bed force sensor without calibration
must be placed between mattress and sheet: this may
annoy the patient during sleep time, due to a differ-
ence in thickness. This leads us to conclude that the
sensor with calibration is preferable, as it has to be
placed under the mattress, and will be consequently
used in the subsequent installations. Apart from that,
patients have noticed any change.
Moreover, the nurses stated that, during the trial
period, there have been some dangerous episodes de-
tected by the kit, such as the opening of a window
during the night, and a patient’s fall out of the room.
In both cases the system detected the alarming situa-
tion and the staff was been able to intervene promptly.
Despite the positive opinions, some problems were
found, in particular due to the occurrence of false
alarms. They were caused primarily by failures in the
communication link, resulting in multiple sending of
alarm events.
Still considering nurses’ opinions, some ideas for
improving the system were identified. First, false
alarms must be avoided, as they can generate a feel-
Overnight Supervision of Alzheimer’s Disease Patients in Nursing Homes - System Development and Field Trial
19

Table 1: The opinion of the nurses about the experimental deployment of the UpTech RSA technology at the nursing home
“Villa Cozza”.
Question Yes No
Is the kit easy to use? 100% 0%
Do you think that the patients monitored have suffered a
stress?
6% 94%
Do you think that the kit has been a source of stress for
nurses?
0% 100%
Would you recommend the use of this kit in nursing
homes?
100% 0%
Question Positive Medium Negative
Overall opinion on the technological kit 89% 11% 0%
Question Yes Quite a lot No
Do you think that the kit can improve the assistance pro-
vided in nursing homes?
61% 39% 0%
ing of distrust by operators against the entire system.
Secondly, customizing different alarms for each user
would be preferable, since each patient has different
behavioural and health conditions. Finally, imple-
menting an even more friendly user interface would
encourage the adoption of the system by nurses unfa-
miliar with technology.
5 DATA ANALYSIS
5.1 Context Characterization
In addition to the real-time monitoring of patients,
it is possible to perform several types of analysis
on the data collected by UpTech RSA sensors over
time, such as obtaining information on the patient’s
habits and, as a consequence, detecting any changes
or unusual behaviours. In the following, some sample
graphs are shown, representing selected daily activi-
ties of the monitored patients, obtained thanks to the
events detected by the sensors. The analysis refers to
data collected from May to June, 2015, by the sensors
located in both the monitored rooms.
First of all, in order to give significance to the
analysed data, some information about the patients
and the daily activities conducted in the Alzheimer’s
ward are necessary. Table 2 represents a sort of daily
diary. Patients remain within the ward during the day:
they can stay together in the common areas, where
they also have lunch and dinner, and can go in/out of
the rooms whenever they want. The entry doors of
the rooms are generally closed during the night. They
are opened by the shift nurse who performs two in-
spection rounds per night, in order to verify that the
Table 2: Diary of daily activities.
Time Activity
7:30 Rooms cleaning
7:00 - 10:00 Patients get out of beds
Morning Patients stay in the common ar-
eas, can go in/out of the rooms
11:30-12:30 Lunch in the dining room
Afternoon Patients stay in the common ar-
eas, some of them have a rest
17:30-18:30 Dinner in the dining room
19:00-21:00 Patients go to bed
22:00 First nurses’ check round
3:00 Second nurses’ check round
patients are sleeping and do not need assistance.
In room 2 there are two patients: only one is mon-
itored through a bed sensor, because she suffers from
AD and often wakes up in the night and goes out of
the room. The other patient moves by wheelchair and
is not able to get off the bed on her own. The AD pa-
tient in room 3 has bed rails, so she can not get out of
the bed autonomously during the night.
Although the system is able to monitor the pa-
tients throughout the entire day, the interesting events
are those occurring during the night. In that pe-
riod, in fact, the user is left alone for most of the
time and thus the data acquired are more significant.
The graphical visualization of the analysis output pro-
vided in the following sub-section has the ability to
help the reader in recognizing and understanding a
large amount of data, and in easily identifying anoma-
lies and behavioural patterns that would not be obvi-
ous otherwise.
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
20

5.2 Data Representation and Analysis
The raw data collected by the sensors installed in the
rooms are often difficult to interpret. Therefore, in or-
der to carry out the data analysis, first of all it is nec-
essary to find a representation allowing to understand
them immediately. Lotfi et al. (Lotfi et al., 2012) af-
firm that, among the various representation methods
presented in the literature, the start-time/duration is
the most effective one for large data sets. The data
acquired from each sensor can be seen as a binary
signal, in which the value “1” is the activation and
the value “0” is the deactivation. Representing in-
formation according to a start-time/duration method
means converting the binary signal into two separate
sequences of real numbers corresponding to the start-
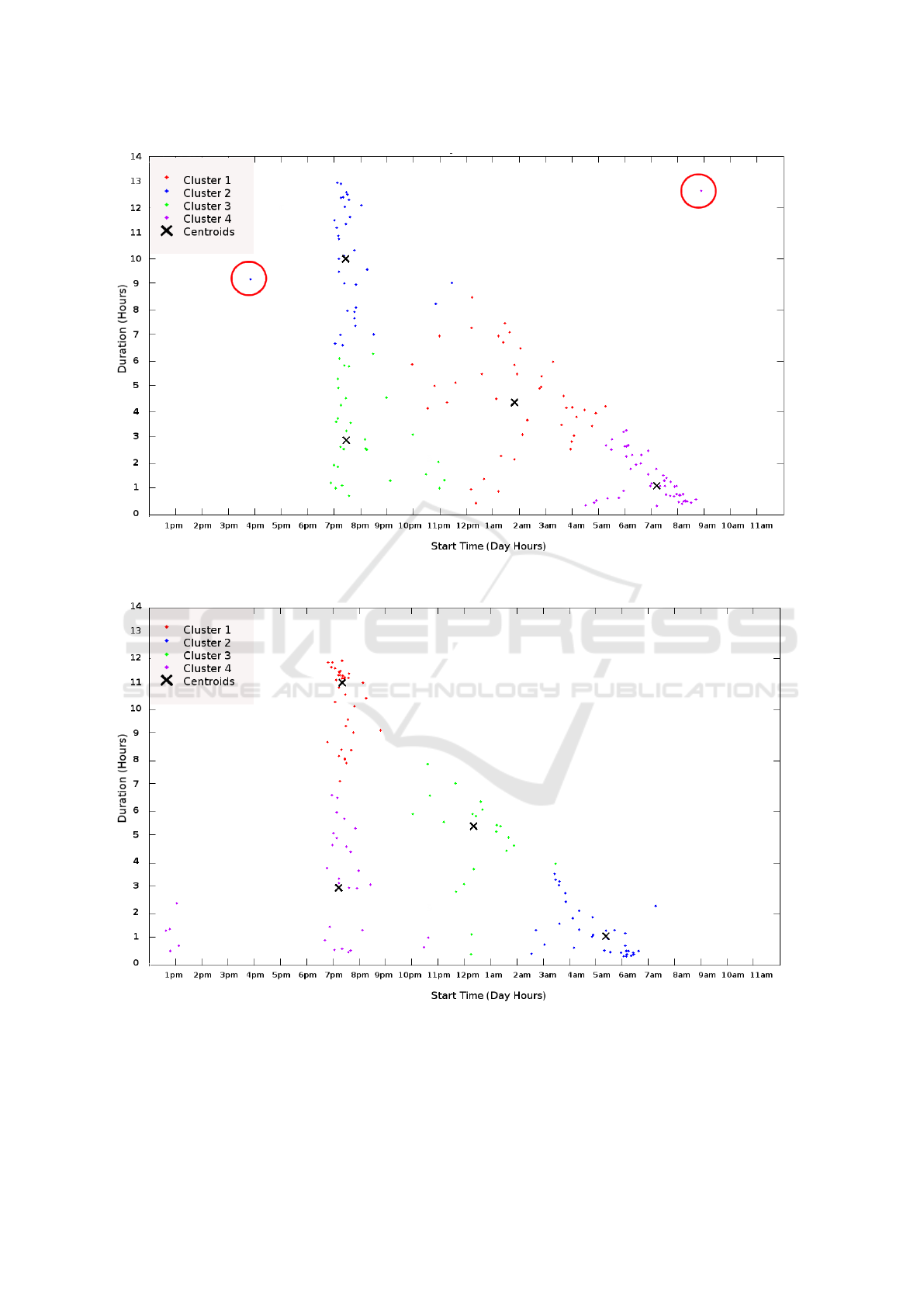
time and duration of each activity, respectively. Fig-
ure 6 shows the start-time/duration graphs of the ac-
tivity detected by the bed sensor, i.e. presumably
sleeping, for each room. Each point on the graph indi-
cates a “sleep” and is characterized by a start-time (on
the abscissa) and a duration (on the ordinate). All ac-
tivities lasting less than 10 minutes have been ignored
because they could indicate sensor activations and de-
activations due to involuntary movements of the sub-
ject while asleep.
Looking at the charts is easy to notice the triangu-
lar shape assumed by the set of points. This result was
expected because life in the nursing home is sched-
uled by the daily diary and, thus, the sleeping activ-
ities are bounded by specific and almost fixed time
constraints. Therefore, it seems plausible that patients
never go to bed before 6:30 PM, and the sleep dura-
tion is inversely proportional to the start-time. The
sparse distribution of points in the triangular-shape di-
agrams indicates that the monitored subject wakes up
several times during the night. In Figure 6 (b) a group
of points is located between 12:30 PM and 13:30 PM:
this suggests that sometimes the patient has a rest after
lunch. On the other hand, looking at Figure 6 (a), the
presence of two outliers (highlighted by red circles)
becomes immediately evident.
Analytically, a first detection of outliers is per-
formed using clustering techniques. In the present
case the K-means algorithm is applied (Nazerfard
et al., 2010), which allows condensing the data. Dif-
ferent techniques can be used to separate normal data
and outliers (Chandola et al., 2009). In this case, a
variation of the threshold filtering method have been
chosen: it consists in both comparing a specific fea-
ture of the points with a threshold and excluding the
outliers. Specifically, for each cluster identified, and
for each point in the cluster, the considered feature is
the euclidean distance between one point and the oth-
ers belonging to the same cluster. Such distances are
then compared against a threshold empirically cho-
sen: all points whose distance exceeds the threshold
are considered outliers. Moreover, to improve the
clustering effect, another iteration of the algorithm
is performed, by excluding the abnormalities found
from the dataset. Clustering is employed as a pre-
processing method, and it can be considered as the
basic level of data analysis. It does not provide a
definitive result, in fact its application to the dataset
has the only aim to help understanding data by means
of a graphical representation.
Another information that can be extrapolated by
combining the data obtained from the bed sensor with
those detected by other sensors, is the identification
of the action carried out after the user came out of
bed. This will enable the possibility to calculate the
occurrences of predefined patterns of activities, in-
stead of single ones. Such an analysis allows to iden-
tify potentially dangerous situations with respect to
behaviours commonly exhibited by the subject, and
not considered as alarms. Each point on the graphs
in Figure 7 indicates a “sleep” and is characterized
by a start-time (on the abscissa) and an end-time (on
the ordinate). As for the start-time/duration, the start-
time/end-time representation requires the conversion
of the binary signal in two separate sequences of real
numbers which in this case correspond to the start-
time and end-time of the activity. The type of activity
shown is still the sleeping, but, according to the ac-
tion carried out subsequently, the shape and colour of
the marker changes. In fact, the graphs show, for each
room, the actions executed within 4 minutes after the
patient got out of bed (end-time), i.e.:
• door opening (marked as a green circle);
• window opening (marked as a black square);
• presence in the bathroom (marked as a blue cross);
• no other activity (marked as a red cross).
This kind of representation has been chosen to em-
phasize, especially in Fig. 7 (b), that some of the
actions are performed only when the patient gets up
at certain times. For example, the patient in room 3
enters the bathroom within 4 minutes after waking up
only in the morning, i.e. only when nurses remove the
rail from the bed. The other activations and deactiva-
tions occurring during the night could indicate that the
subject has moved or was seated up on the bed, while
the openings of the door or window are probably due
to the presence of the medical staff.
Conversely, looking at Figure 7 (a), the observer
can notice the patient very often goes to the bathroom
or opens the door immediately after getting up. This
agrees with the reports of the nurses concerning the
Overnight Supervision of Alzheimer’s Disease Patients in Nursing Homes - System Development and Field Trial
21
(a) Room 2
(b) Room 3
Figure 6: Start-time/duration graphs of the “sleeping” activity detected from May to June 2015, respectively in (a) room 2,
and (b) room 3.
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
22
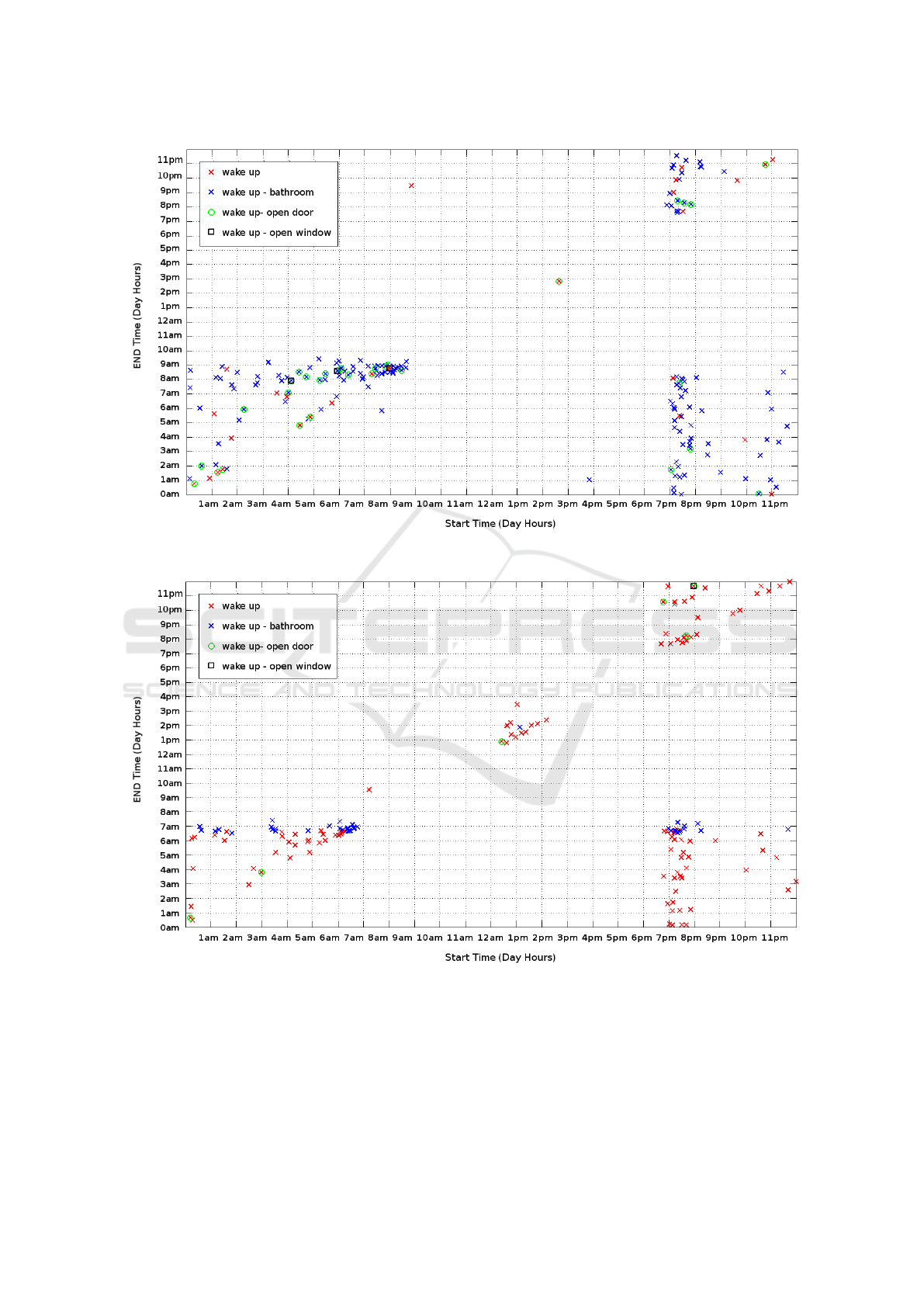
(a) Room 2
(b) Room 3
Figure 7: Start-time/end-time graphs representing the activities performed after waking up by the patients housed respectively
in (a) room 2, and (b) room 3, from May to June 2015.
fact that the monitored elder is very lively, and often
gets up during the night.
In Table 3, the percent occurrence rates of each
activity described above are given, limited to the night
hours.
The analysis described so far is just the very first
step to identify the user’s behavioural patterns and ab-
normal situations. Until now, we focused on the rep-
Overnight Supervision of Alzheimer’s Disease Patients in Nursing Homes - System Development and Field Trial
23

Table 3: Hit rate of the getting up action followed re-
spectively by the action of entering the bathroom, open-
ing/closing the door, or opening/closing the window, in the
time slot between 09:00 PM and 06:00 AM.
Event detected after
awakening
Room2 Room3
Presence in the bathroom 76% 15%
Door opening 14% 2%
Window opening 0% 0.2%
None 10% 82.8%
resentation and visualization of data, extracting some
preliminary information on the habits of two mon-
itored patients. Nevertheless, there is still a long
way to go. Although the detection of outliers can
be very useful in this context, however, it is neces-
sary to set up a predictive system able to identify in
advance any anomalous situation to help the nursing
home staff making the necessary arrangements. As
already hinted, one of the aspects emerged during dis-
cussion with nurses is the need of alarm personaliza-
tion. In fact, a situation may be potentially dangerous
for a user, while it may be harmless for another one.
This strongly depends on motor and cognitive skills of
each patient. Although this can be done manually by
nurses via graphical user interfaces, a significant con-
tribution comes from the analysis of patients’ habits.
One of the future developments is to extend the be-
havioural analysis in the long term, aimed at recog-
nizing unusual, and, therefore, potentially dangerous
situations and notifying them to the staff, in a com-
pletely automatic way.
6 CONCLUSION AND FUTURE
WORK
The issue addressed in this paper is the need to of-
fer assistance to a growing number of AD patients, by
providing solutions that can be applied both at their
homes, and in nursing homes. Different types of pa-
tients have their own specific requirements: this case
deals with AD, but it could be possible to adapt the
current solution to patients with different pathologies,
by changing the sensors selected and offering proper
services. The results obtained from the first exper-
imental installation of the monitoring system high-
lighted the effectiveness of the proposed solution to
support the nurses during the night supervision of pa-
tients. The effectiveness could grow even more by
extending the pool of monitored patients. Monitoring
all the patients leads to increase the convenience for
the nurses and, above all, the degree of safety of the
patients. For example, by monitoring the presence to
bed at night time for all the patients, it could be pos-
sible to detect any accidental fall or necessity to help.
Other advantages brought by the UpTech RSA pro-
posal are the introduction of innovative technologies
in the nursing home facility, the efficient use of hu-
man and technical resources, and the quality of care
improvement.
ACKNOWLEDGEMENTS
This work was partially funded through an Innova-
tion Voucher issued in the framework of the WIDER
project (Green Growing of SMEs: Innovation and De-
velopment in the Energy Sector in the Med Area), and
partially by the AAL 20141041 project “Home4Dem”
(HOMEbased ICT solutions FOR the independent liv-
ing of people with DEMentia and their caregivers),
co-founded by the Active and Assisted Living Joint
Platform.
REFERENCES
Ancker, J. S., Witteman, H. O., Hafeez, B., Provencher,
T., de Graaf, M. V., and Wei, E. (2015). The invisi-
ble work of personal health information management
among people with multiple chronic conditions: Qual-
itative interview study among patients and providers.
J Med Internet Res, 17(6):e137.
Bowens, F. M., Frye, P. A., and Jones, W. A. (2010).
Health information technology: integration of clini-
cal workflow into meaningful use of electronic health
records. Perspectives in health information manage-
ment / AHIMA, American Health Information Man-
agement Association, 7:1d.
Chandola, V., Banerjee, A., and Kumar, V. (2009).
Anomaly detection: A survey. ACM Comput. Surv.,
41(3):15:1–15:58.
Chiatti, C., Masera, F., Rimland, J., Cherubini, A.,
Scarpino, O., Spazzafumo, L., and Lattanzio, F.
(2013). The up-tech project, an intervention to sup-
port caregivers of alzheimer’s disease patients in italy:
study protocol for a randomized controlled trial. Tri-
als, 14(1).
Chiatti, C., Rimland, J. M., Bonfranceschi, F., Masera, F.,
Bustacchini, S., and Cassetta, L. (2015). The up-
tech project, an intervention to support caregivers of
alzheimer’s disease patients in italy: preliminary find-
ings on recruitment and caregiving burden in the base-
line population. Aging & mental health, 19(6):517–
525.
Freedman, V. A. (2005). Barriers to implementing tech-
nology in residential long-term care settings. Polisher
Research Institute.
Huston, C. (2013). The impact of emerging technology on
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
24

nursing care: Warp speed ahead. OJIN: The Online
Journal of Issues in Nursing, 18(2).
Institute of Medicine (1986). Improving the Quality of Care
in Nursing Homes. The National Academies Press,
Washington, DC.
Kahanp
¨
a
¨
a, A., Noro, A., Finne-Soveri, H., Lehto, J., and
Per
¨
al
¨
a, M.-L. (2016). Perceived and observed quality
of long-term care for residents - does functional abil-
ity account? International Journal of Older People
Nursing.
Kim, S.-S., Oh, K. M., and Richards, K. (2014). Sleep dis-
turbance, nocturnal agitation behaviors, and medical
comorbidity in older adults with dementia: Relation-
ship to reported caregiver burden. Research in Geron-
tological Nursing, 7(5):206–214.
Lee, D., Heo, S. H., Yoon, S.-S., Chang, D.-I., Lee, S.,
Rhee, H.-Y., Ku, B. D., and Park, K.-C. (2014). Sleep
disturbances and predictive factors in caregivers of pa-
tients with mild cognitive impairment and dementia. J
Clin Neurol, 10(4):304.
Lotfi, A., Langensiepen, C., Mahmoud, S., and Akhlagh-
inia, M. (2012). Smart homes for the elderly demen-
tia sufferers: identification and prediction of abnormal
behaviour. Journal of Ambient Intelligence and Hu-
manized Computing, 3(3):205–218.
Lowry, S. Z., Ramaiah, M., Patterson, E. S., Brick, D., Gib-
bons, M. C., and Paul, L. A. (2015). Integrating elec-
tronic health records into clinical workflow: An ap-
plication of human factors modeling methods to spe-
cialty care in ‘obstetrics and gynecology’ and ‘oph-
thalmology’. Technical report, National Institute of
Standards and Technology.
Mao, H.-F., Chang, L.-H., Yao, G., Chen, W.-Y., and
Huang, W.-N. W. (2015). Indicators of perceived use-
ful dementia care assistive technology: Caregivers’
perspectives. Geriatrics & Gerontology International,
15(8):1049–1057.
Milte, R., Shulver, W., Killington, M., Bradley, C., Rat-
cliffe, J., and Crotty, M. (2016). Quality in residen-
tial care from the perspective of people living with de-
mentia: The importance of personhood. Archives of
Gerontology and Geriatrics, 63:9–17.
Nazerfard, E., Rashidi, P., and Cook, D. (2010). Discover-
ing temporal features and relations of activity patterns.
In Data Mining Workshops (ICDMW), 2010 IEEE In-
ternational Conference on, pages 1069–1075.
Occhiuzzi, C., Vallese, C., Amendola, S., Manzari, S.,
and Marrocco, G. (2014). Night-care: A passive
{RFID} system for remote monitoring and control
of overnight living environment. Procedia Computer
Science, 32:190 – 197. The 5th International Confer-
ence on Ambient Systems, Networks and Technolo-
gies (ANT-2014), the 4th International Conference on
Sustainable Energy Information Technology (SEIT-
2014).
Organization for Economic Co-operation and Development
(2015). Focus on health spending: Oecd health statis-
tics 2015.
Pombo, N., Spinsante, S., Chiatti, C., Olivetti, P., Gambi,
E., and Garcia, N. (2015). Assistive technologies for
homecare: Outcomes from trial experiences. In ICT
Innovations 2015 Proceedings, Workshop ELEMENT
2015.
Spijker, A., Vernooij-Dassen, M., Vasse, E., Adang, E.,
Wollersheim, H., Grol, R., and Verhey, F. (2008).
Effectiveness of nonpharmacological interventions in
delaying the institutionalization of patients with de-
mentia: A meta-analysis. Journal of the American
Geriatrics Society, 56(6):1116–1128.
Vuong, N. K., Goh, S. G. A., Chan, S., and Lau, C. T.
(2013). A mobile-health application to detect wander-
ing patterns of elderly people in home environment.
In 2013 35th Annual International Conference of the
IEEE Engineering in Medicine and Biology Society
(EMBC), pages 6748–6751. Institute of Electrical &
Electronics Engineers (IEEE).
Overnight Supervision of Alzheimer’s Disease Patients in Nursing Homes - System Development and Field Trial
25
