
Information Technology for Medical Appropriateness Through
Support Algorithms and Recovery of Patients’ Clinical History
Enrico Serracca, Marco Brambilla, Tito Poli and Elena Martinelli
Informative Service Corporate, University Hospital of PARMA (PR), Parma, Italy
Keywords: Medical Appropriateness, Information Technology, E-Health, Data Mining.
Abstract: In the health sector, the current intention of the Ministry of Health and of the Italian Government is to
decrease healthcare squandering, to invest in research and to support the NHS. In this context the theme of
appropriateness of treatment is essential; in fact the Health Ministry is committed to establish guidelines for
the appropriateness of prescription, indicating the "conditions of provision" and "indications of
appropriateness". A number of key actors however complain that this approach, along with others (e.g.
multifaceted educational programs, electronic systems of frequency filtering, such as limiting the number of
available tests to the requesting physicians) lead to uncertain and often ineffective results. This work
highlights how the adoption and use of Information Technology (IT) in clinical settings is contributing to
the optimization of NHS resources and to the governance of the healthcare delivery activities, in particular
for the management and control of appropriateness of care. As an example, the adoption of a computerized
alerting system by the University Hospital of Parma has brought out significant results. System integration
through standard protocols such as HL7, fully normalized data repositories that univocally identify patients,
diagnosis and health service provided are crucial in the healthcare context.
1 INTRODUCTION
In recent years the Italian NHS has undergone
budget cuts of more than 30 billion, with negative
effects on research, on generational turnover of
healthcare personnel, on investments in technologies
and on the number of hospital beds. In fact, due to
the reduction of more than 9000 hospital beds
between year 2011 and 2012, the Italian NHS
accounts for 3.5 beds per 1000 inhabitants,
significantly less than Japan (14 beds/1000
inhabitants), Germany (8,2 beds /1000 inhabitants),
or Austria (7.6 beds/1000 inhabitants) .
This factor has led hospitals to adopt a business
profile, in which productivity and production costs
are key.
It is now a widespread practice to outsource or
concentrate services to rationalize resources and
improve efficiency. Furthermore the Italian
Government plans to reduce squandering through
additional healthcare budget cuts, estimated up to 10
billion euro, to be invested in research, in healthcare
efficiency improvements or in taxation reduction.
In this regard, the intention is to implement the
concept of medical appropriateness, by defining the
guidelines for "conditions of deliverability " and
"indications of appropriateness". Currently (August
2015) the first draft of the Decree concerning
appropriateness of prescriptions foresees constraints
on 180 health services in 7 main areas:
- Dentistry, Genetics, CT and MRI, dialysis,
nuclear medicine, laboratory tests and allergology.
Health services that go beyond the deliverability
constraints indicated by the caring physician will be
charged to the patient.
Is this approach appropriate to improve the
quality of healthcare?
Many physicians argue that you cannot make
cuts to health care indefinitely, nor can further
reduce the tools for the collection of a good
anamnesis, or to shorten the duration of a surgery. In
addition several literature studies show that,
educational programs, automatic filtering of
prescriptions and generalized budget cuts lead to
mixed results, and are hardly ever productive.
Technological development and Information
Technology, although increasingly expensive, have
on the other hand greatly improved healthcare
delivery efficiency and have allowed a more precise
definition and monitoring of appropriateness of care,
426
Serracca, E., Brambilla, M., Poli, T. and Martinelli, E.
Information Technology for Medical Appropriateness Through Support Algorithms and Recovery of Patients’ Clinical History.
DOI: 10.5220/0005816504260431
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 5: HEALTHINF, pages 426-431
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

through the use of models and algorithms. Proofs
abound that these algorithms allow to reduce costs,
by highlighting "unnecessary" health services in
advance.
In addition, the computerization of the health
area, the definition of standard protocols such as
HL7, has allowed the hospital information systems
to communicate more easily, thus promoting-clinical
data sharing. The purpose of this publication is to
highlight and demonstrate the benefits achieved in
health care by investing in Information Technology.
2 MEDICAL APPROPRIATENESS
AND INFORMATION
TECHNOLOGY
In medicine there is no mathematical definition of
appropriateness. The most accredited definition of
appropriateness among healthcare authorities is "the
measure of how a care delivery system and services
are adapted and effective to the clinical needs of
patients in accordance with current knowledge and
best clinical practices".
The achieved health benefits must definitely
outweigh the risks for the patient's health. In this
context, we can distinguish two opposite cases:
- "inappropriate" tests that, besides raising anxiety
in patients and consuming resources, could
generate false positives and lead to additional
diagnostic exams or even to inadequate therapy;
- "insufficient" tests, i.e. not performed diagnostic
exams that would be needed for a correct
diagnosis.
To address the first issue algorithms have been
developed to support clinicians on diagnostic
prescriptions appropriateness, in particular in the
area of laboratory tests and diagnostic imaging. Few
studies address the second issue.
In general we can distinguish three types of
appropriateness:
- Clinical appropriateness: it refers to the
efficiency criteria adopted in the diagnostic-
therapeutic process and in the request of
laboratory tests.
- Prescription appropriateness: more effective
clinical approach for the diagnosis (e.g.
investigation diagnostic) and treatment (e.g.
pharmacological) of diseases.
- Organizational appropriateness: fair and efficient
administration of the available resources in
relation to the clinical case to be treated.
Prescription appropriateness is perhaps the most
debated topic at present, for its legal and economic
implications. See for example the allegations and
wages reductions to family physicians due to
"improper" prescriptions. In this sense the
government proposes to adopt the above mentioned
''terms of deliverability" and to define clear
guidelines, no compliance to which could result in
administrative and/or pecuniary sanctions for the
clinician, or even the revocation of the employment
relationship.
Information Technology provides computer tools
that suggest to clinicians the most “appropriate”
therapy, improve the clinical approach and decision-
making for the use of medications and treatment of
diseases. We refer for instance to "therapeutic
algorithms" developed by AIFA (the Italian Drug
Agency) in collaboration with experts in the field
(University of Padua, the Italian association for the
study of the liver, an Italian association of
diabetology and the association of medical
diabetologists).
One such algorithm concerns the management of
triple therapy for hepatitis C (HCV algorithm). Born
from mathematical models that consider many
multiscale parameters, this algorithm is a "guide" in
the use of Direct-acting antiviral (Daa) drugs, later
replaced by second generation Daa. Access to these
new therapies foresees treatment of patients based
clinical urgency criteria.
A second algorithm concerns the treatment and
therapy of type 2 diabetes mellitus.
The "Diabetes" algorithm foresees three steps:
1. Identification of the glycemic index.
2. Therapy definition (no contraindications).
3. Therapy definition in presence of
contraindications or intolerance to metformin.
Two additional algorithms for the management of
arterial hypertension and osteoporosis are also
foreseen.
The clinical and organizational appropriateness
are closely linked. Recently the usage of laboratory
resources and the demand for laboratory exams has
significantly increased. According to data from
British Government, an estimated 70% of clinical
diagnosis depend on laboratory data. The main
reasons are ageing of population and related increase
in chronic conditions.
Given the limited resources of current NHS
system the Ministry of Health is considering the
option to produce a list of diseases and of related
supported diagnostic and therapeutic prescriptions,
outside which patients should pay out of pocket.
Information Technology for Medical Appropriateness Through Support Algorithms and Recovery of Patients’ Clinical History
427

Thus to comply with clinical appropriateness, lab
technicians and clinicians will both need to provide
more and more specific and sensitive tests and also
achieve a greater clinical competence in the
evaluation of the benefits brought by lab tests to
address each patient's disease.
IT offers supporting algorithms also for this
"educational/diagnostic" process.
The University Hospital of Parma has developed
a computerized alerting tool based on re-testing
intervals, linked to the order entry system, that
generates pop-up alerts when 15 pre-defined
laboratory tests violate the criteria of
appropriateness.
The criteria are violated when biological
plausibility is not respected or tests are repeated
before the defined minimum intervals:
- C-reactive protein (CRP, repeat <24 hours);
- Glycated hemoglobin (repeat < 2 months);
- Beta-human chorionic gonadotropin (HCG beta;
incompatible with age < 9 and > 60 years);
- Prostatic specific antigen (PSA; incompatible
with PSA reflex and female gender; repetition <3
months);
- Thyroid stimulating hormone (TSH,
incompatible with the TSH reflection; repetition
<6 weeks);
- Protein Electrophoresis (repeat <7 days);
- Total cholesterol, high density lipoprotein
cholesterol (HDL-C) and low density
lipoproteins (LDL-C) (repeat <2 months);
- Brain natriuretic peptide (BNP; repetition <24
hours);
- Procalcitonin (PCT; repetition <24 hours);
- Ferritin (repeat <1 week);
- Vitamin B and folic acid (repeat <1 year);
- Immunoglobulin and albuminuria (repeat <3
months).
765 (22%) out of a total of 3539 requests generated
by the departments of geriatrics of the hospital,
between October 2014 and March 2015, have
infringed the preset criteria and generated the alert
pop-up. After the alarm, 591 requests were canceled
(17% of the total and 77% of the alerted tests)
allowing the hospital to save € 3387 in six months.
Once applied to the whole hospital, the system will
"educate" doctors to the correct and effective use of
laboratory tests, freeing up resources to treat those
who need it most, besides generating significant cost
savings.
3 INTEGRATION AND DATA
RECOVERY
The computerization and integration between the
different Hospital Information System (HIS)
components is essential in order to achieve effective
results for medical appropriateness.. The use of an
integrated virtual patient record available from any
healthcare delivery location, appears a good solution
to allow the dematerialization of documents and
easy circulation and exchange of clinical
information.,.
To this aim the model IHE (Integrating the
Healthcare Enterprise) for the integration of health
information systems was developed. This model
uses communication standards like HL7 and
DICOM.
HL7 is now at version 3.0 and allows
applications of the systems (HIS, LIS, RIS etc..) to
interact based on events such as ADT (admission,
discharge, transfer), ORM (request for examination),
MDM (transmission of documents or medical
reports) etc.
These messages include a header (MSH),
followed by the description of the event (EVN), the
patient demographic data (PID) and information
about administered visits or healthcare services.
IHE has therefore a standard structure and allows
easy communication between different health
facilities without expensive interventions on the
existing hardware and software.
A transmission system for the exchange of
messages is also needed to ensure interoperability
between the information systems. . The meaning
attributed to messages must to be shared by both the
sender and the receiver; an application that converts
the intermediate information exchanged in a format
common to all the health information realities is
therefore required (for example from XML -> HL7).
Therefore in a logic-oriented EHR it is crucial to
use middleware that ensures a common
understanding of the messages and sharing the rules.
Several such middleware systems are available,
e.g. Picasso, Spagic or JCAPS. An ideal solution for
integration between health information systems.is
also the open-source Mirth software, developed in
Java.
Mirth supports different formats (such as HL7,
queries from the database, EDI / X12, XML,
NCPDP, DICOM and Delimited Text) and protocols
(TCP / LLP, http, JDBC and FTP ).
It allows you to manage and manipulate HL7
messages according to the needs of listening
systems; it makes use of channels that can take two
HEALTHINF 2016 - 9th International Conference on Health Informatics
428
profiles:
- Router: manipulates messages using filters and
transformations according to the demands of the
target systems. Subsequently perform message
routing.
- Broadcast: the information is sent via broadcast
to all listening applications.
Mirth has therefore the advantage of managing the
flows of information systems using independent
channels. The latter will verify the conformity of
messages in order to make them understandable by
the listening systems.
Furthermore, as mentioned before, messages
don't need to be HL7 compliant; the Middleware is
quite versatile and can in theory be used in any
language for the exchange of information. It is the
channels, via Java libraries or JavaScript commands,
that will transform the message.
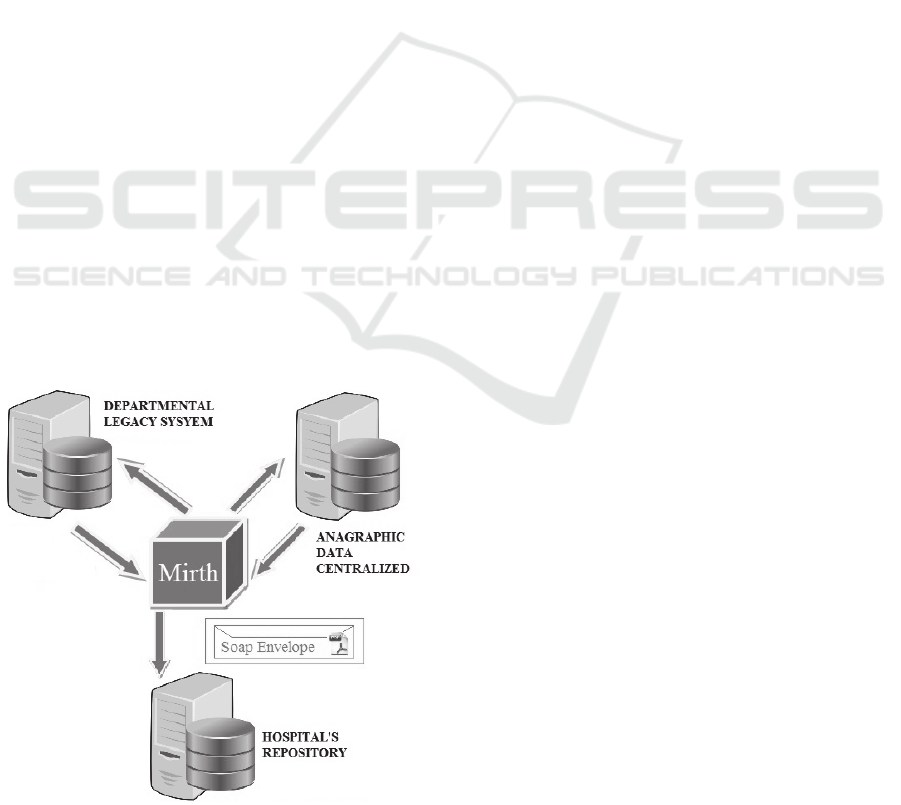
In the following we show an example of
integration for the archive of medical reports from a
hospital department of Parma to be sent and stored
into the hospital's repository.
In this case the exchange of messages is handled
by Mirth via two channels:
1. A channel dedicated to the extraction of patients'
data (via T-SQL query) from the department db,
required to generate medical reports in pdf
format.
2. Another channel used as a web service sender,
which associates the report created before (and
encrypted) to patients' data and then generates an
HL7 message. This message will be added to a
SOAP envelope and sent to the web service
listener of the Central Repository.
Figure 1: Integration Department-Repository.
The image shows that besides performing an
exchange of messages with the department, the
middleware also performs an alignment with the
anagraphic centralized db. In fact, the existence of
univocal anagraphic data is mandatory to achieve a
correct integration and to possess unique anagraphic
data. Often in hospital realities the patient's
anagraphic data coming from the wards, are
discordant with those of Central anagraphic system.
This happens because often patients arrive at
emergency units or directly in departments either
unconscious or without identification documents,
thus a correct patient's identification is not possible
at admission time. In other cases the operator
happens to make mistakes in patient's references
transcription.
This requires a process for the reunification of
personal data ("Patient's Demographic
Reconciliation"). A reference database of anagraphic
univocal data, MPI (master patient index), is
important not only to reconstruct patient's health
data and patient's anagraphic data, but also for all the
alignments with the accessories db of common use
(medical services, regional or national encodings,
general practitioners data).
The MPI anagraphic registry is therefore
essential in patient-centered architectures and the
patient's relative code idMPI is the unique identifier
from which all patient's clinical or administrative
events can be recovered.
However the concept of MPI is not sufficient to
solve the problems of integration between different
information systems. Frequent problems are caused
by:
1. Duplication: Mickey Mouse has two codes (for
example, 001 and 100) in the same building
Disneyland Clinic.
2. Overlapping codes: the same patient has multiple
codes in two or more structures (001 at the
Disneyland Clinic and 100 at the Disneyworld
Clinic).
3. Errors of transcription in individual hospital
departments: incomplete or misspelled names or
surnames, birth dates where the day and month
are reversed (e.g. 10/01/1900 → 01/10/1900).
Several algorithms have been developed to solve
these problems and prevent the occurrence of false
positives (the record is assigned to the wrong
patient) or false negatives (a patient has multiple
records) in a matching.
In a recent integration test between a legacy
information system of a department and the central
repository of Parma University Hospital a
Information Technology for Medical Appropriateness Through Support Algorithms and Recovery of Patients’ Clinical History
429

middleware (Mirth) was used that was interfaced
with the central demographic registry in order to
extract the MPI code of patients (not present among
the fields of the departmental system). In particular,
the matching algorithm used as keywords:
1. The date of birth of the patient
2. The patient's last name
3. The patient's name
They were the only fields in the legacy system of the
department that could guarantee the uniqueness of
the patient.
The algorithm is actually a step-by-step
procedure; from the first matching, mentioned
above, the MPI code for about 73% of patients was
recovered.
In the next step we made a matching targeted to
transcription errors. In particular, we used substrings
starting from the same search keys used earlier. To
ensure uniqueness in this case, in addition to the
surname, name and date of birth, the fields "address"
and "telephone number" (when they were present
and complete) were used. At the end of this process
the MPI code of more than 90% of patients was
recovered (67664 of 74971 initial patients ).
Through this system, so it was possible to store
medical reports and patient records of that
department in the central repository, without any
false positive or false negative.
4 CONCLUSIONS
Usually Hospital Information Systems are rather
fragmented and consist of isolated computerized
structures including heterogeneous hardware
equipment and software applications. Consequently
the concept of medical appropriateness cannot be
separated from the computerization of hospital
activities and from the integration of these different
health information systems.
The access to a central repository that provides
information from different departments (e.g.
laboratory, radiology, anatomy pathology etc.) can
facilitate patient's data retrieval and sharing. It can
allow a Medical Doctor to know the patient's
medical history, the clinical exams of performed by
different structures and provide proper diagnosis
with minimal requests for improper medical exams.
These information can also be used both as variables
by the algorithms supporting physicians on
evaluating the appropriateness of requests and also
to better investigate on exams (for example,
diagnostic images such as CT and MRI) through
operations such as chiaroscuro, zoom etc.
Obviously the use of middleware is essential to
"standardize" the exchange of data and reduce risk
factors related to the circulation of information
between the different legacy systems and the central
repository.
We have assessed how Mirth, in addition to
providing an open source solution, ensures the easy
and independent interoperability between
applications, providing transparency in the flow of
data and adapting to changes in hospital structures,
IT infrastructures and in clinical data.
Thanks to the use of anagraphic MPI, the
middleware can access a separate centralized
anagraphic registry (but related to the anagraphic
registry of the hospital) and can make available to
all the different hospital systems a number of
functions via the web for the management of
demographic data.
Moreover the idMPI, in addition to connecting
the patient ID with that related to any other access at
any hospital structures, adapts to different logics and
hospital settings and ensures adherence to the
requirements of the Italian Health System (uniquely
identifying the patient, avoiding homonyms and
unifying double anagraphic positions).
In summary, it is therefore essential to invest in
information technology, in order to improve the
management of health resources, to integrate the
multiple clinical information, in the optics to provide
an adequate health care to each patient
(personalized medicine) reducing improper requests,
as well as to obtain reliable information about
medical exams through a simple Web browser.
REFERENCES
Tamarin A., 2015. I tagli alla sanità sono ormai
inevitabili. Ma almeno si usino i costi standard.
www.quotidianosanita.it.
Fassari L., 2015. Appropriatezza prescrittiva. Cambiano
misure per 180 prestazioni. Tac, Rmn, test generici ed
esami di laboratorio. Ecco il documento.
www.quotidianosanita.it.
R J Lock., J Clin Pathol, 2004. Rational requesting or
rationing testing?
Lippi G., 2015. Effectiveness of a computerized alert
system based on re-testing intervals for limiting the
inappropriateness of laboratory test requests.
Verstappen WH, van der Weijden T, Sijbrandij J, Smeele
I, Hermsen J, Grimshaw J, et al. 2003. Effect of a
practice-based strategy on test ordering performance
of primary care physicians: a randomized trial.
Janssens PM, Wasser G. 2013. Managing laboratory test
ordering through test frequency filtering.
HEALTHINF 2016 - 9th International Conference on Health Informatics
430

Chu KH, Wagholikar AS, Greenslade JH, O'Dwyer JA,
Brown AF. 2013. Sustained reductions in emergency
department laboratory test orders: impact of a simple
intervention.
Perry Yastro., Arthur Davidson 2008. I The Role of Master
Patient Index (MPI) and Record Locator Services
(RLS) on the Implementation of HIEs for
Medicaid/SCHIP.AHRQ Medicaid-SCHIP TA
Webinar.
Information Technology for Medical Appropriateness Through Support Algorithms and Recovery of Patients’ Clinical History
431
