
Nursing Documentation Improvement at Post-Acute Care Settings
Ryoma Seto
1
and Toshitaka Inoue
2,3
1
Division of Healthcare Informatics, Faculty of Healthcare, Tokyo Healthcare University, Tokyo, Japan
2
Dept. of Social Welfare Science, Faculty of Health and Social Welfare Science, Nishikyushu University, Saga, Japan
3
Seishinkai Inoue Hospital, Fukuoka, Japan
Keywords: Clinical Documentation Improvement, Electronic Health Records, Nursing Documentation, Patient Safety,
Vital Signs Documentation, Post-Acute Care Settings.
Abstract: Although nursing documentation is very important for patient safety, it forces nurses to spend increasing
amounts of their working time completing it. In this study, I evaluated the time lag between patient events to
completion of nursing documentation at two Post-Acute Care settings (called as “Care-Mixed Hospital” in
Japan, similar to nursing home). The mean time lag at Hospital A, which did not implement an automatic
documentation system (ADS) was 197.3 min [progress note regarding vital signs (VS), 208.2 min and the
others, 196.1 min. The mean time lag at Hospital B, which had implemented ADS, was 3.2 min (only
progress note regarding VS). ADS is effective in improving instantaneity on nursing documentation at post-
acute care settings.
1 INTRODUCTION
Nursing documentation is very important for
maintaining a good quality of nursing care.
Therefore, in previous studies, standardized
documentation forms were developed both in paper
and electronic formats (Romano, 1982). The
documentation framework (e.g., document form)
depends on the clinical situation and whether the
setting is clinical such as in an acute care facility or
community-based such as in a patient home. These
factors have an impact on how useful clinical data
can be collected (Curran, 1994). Therefore, nursing
documentation comprises various kinds of
documents that increase workload. Nursing
documentation is a significant proportion of the
workload that is associated with inpatient nursing care
(McCartney, 2013) (Asaro, 2003). It is unfortunate
that good documentation improves delivery of care
but creates a sub-optimal working environment for
clinical nurses at post-acute care settings.
To improve the situation, clinical document
improvement (CDI) was created. One of the most
popular CDI approaches involves the use of a
template. By using the template in the electric
medical record (EMR), nurses were able to reduce
their workload with respect to completing nursing
documentation (Richardson, 2015). The next CDI
approach used minimum data sets (MDSs). MDSs
comprised standardized data sets that can cover most
patients. In a previous study, MDS maintained the
quality of documentation and reduced the nurses’
workloads (Ranegger, 2015). Other CDI approaches
involve modifying the system design, which is time
consuming; therefore, early implementation is very
important (Read-Brown, 2013).
Moreover, secondary methods for nursing
documentation have rapidly spread. Needless to say,
nursing at post-acute care settings encompasses not
only the physical problems of the patient but also
psychosocial aspects. However, the patient’s
physiological symptoms are not easy to elucidate.
One study analyzed the patient’s physiological
requirements (Hill, 2015). Nursing documentation is
correlated with knowledge management. A study
analyzed the integration of narrative documents,
database storage, and connectivity with clinical
guidelines (Min, 2013). These challenges are
critically important to resolve; however, solutions
are only being trialed in a limited number of clinical
settings (e.g., university hospital and national
institutional hospital).
Nursing terminology comprises formal languages
and sub-languages (Mead, 1997). Nursing
terminology is complex. Furthermore, the quality of
nursing documentation may also be affected by
clinical governance regulations (Dehghan, 2013).
Therefore, CDI in nursing is a very long road.
Seto, R. and Inoue, T.
Nursing Documentation Improvement at Post-Acute Care Settings.
In Proceedings of the International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2016), pages 163-168
ISBN: 978-989-758-180-9
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
163

However, CDI in nursing is one of the hottest
topics. Collins (Collins, 2013) noted that nursing
documentation patterns had been linked to the
patient’s mortality. In particular, vital signs (VS)
documentation is important. If the quality of VS
documentation is poor (delayed or incorrect), quick
responses to the patients’ requirements will be
difficult.
Overall, this study aims to elucidate the
effectiveness of CDI in nursing using the automatic
documentation system (ADS) at post-acute care
settings.
2 METHODS
2.1 Research Objectives
This study was performed at two post-acute care
settings. Both settings were very similar. The
settings (called as “Care-Mixed Hospital” in Japan,
but called as “Nursing Home” in the United States
and Europe) have 100–199 beds (this range of bed
numbers in the hospital represents the median of all
hospitals in Japan), including community care unit
(plans and implements follow-up care after
discharge).
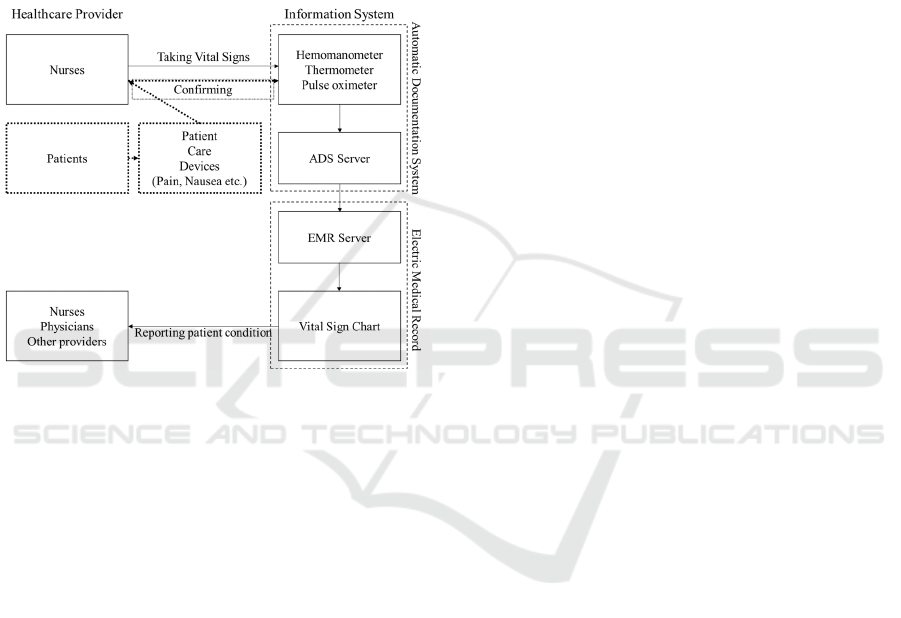
Hospital A implemented EMR but did not
implement ADS. Hospital B implemented both EMR
and ADS. ADS acts as a sub-system for the
automatic recording of VS, including body
temperature (BT), blood pressure (BP), and
pulse/SpO2, from an integrated VS recording
device, which includes a hemomanometer,
thermometer, and pulse oximeter. The devices flow
data to EMR (Fig. 1).
Figure 1: Relation with EMR and ADS.
2.2 Data Collection
The research period was 5–6 months from July 2015
to September 2015.
At Hospital A, all nursing progress records of
24,355 patient–days were extracted from EMR.
Hospital A was selected for the “focus charting
method” using one of the nursing documentation
forms (e.g., SOAP). The charting method comprised
data collection on patient status and condition,
actions (interventions) by the nurse or other
healthcare provider, and responses of the patient
(Lampe, 1985) (Table 1). All progress notes were
distinguished from VS documentation or other
documentation using the text-mining methods.
Table 1: Overview of Documentation at Hospital A.
Focus Data Action Response
Lines
(per patient–day)
3.9 3.7 1.6 0.5
Characters
(per patient–day)
18.6 124.8 29.6 10.6
At Hospital B, data records of VS of 21,268
patient–day were extracted from the ADS server. On
an average, BP was recorded at 1.2 times/patient–
day, BT was 1.6 times/patient– day, and pulse/SpO2
was 1.4 times/patients–day.
2.3 Data Analysis
At both Hospitals A and B, the time lag between
patient events, nurses taking VS, and documentation
reaching EMR was calculated from the EMR system
log and/or ADS server (Fig. 2). Because previous
studies noted that CDI must create a considerably
busy working situation for nurses (Lees, 2010), time
lag was separated by time zone.
Figure 2: Example of Time Lag of Nursing
Documentation.
2.4 Ethical Consideration
This study was performed under national ethical
guidelines for epidemiological studies. All data of
nursing documentation was anonymized.
At Hospitals A and B, this study was approved
under the protocol for each hospital (CEO and/or
Management Board approved).
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
164

3 RESULTS
3.1 Frequency of Taking Vital Signs by
Time Zone
The frequency of taking VS is shown by time zone
at each hospital (Fig. 3). Each hospital has three
peaks taking VS. The peaks at Hospital A occurred
at 6 AM (13.1%), 10 AM (21.5%), and 7 PM
(16.8%). The peaks at Hospital B were at 6 AM
(21.1%), 1 PM (12.1%), and 5 PM (12.2%). Taking
all of the documentation into account across all three
peak times at both the hospitals, 51.5% of all
documentation was completed at Hospital A and
45.4% was completed at Hospital B.
Figure 3: Frequency of Taking Vital Signs by Time Zone.
3.2 Time Lag between Taking VS and
Documentation
The time lag between taking VS and the nursing
documentation reaching EMR was 197.3 min at
Hospital A. VS documentation takes a significantly
longer time (p < 0.0001, Wilcoxon’s test) of 208.2
min to reach EMR than other documentations, which
only takes 196.1 min. The time lag at Hospital B
Figure 4: Time Lag between taking VS and ocumentation.
was just 3.2 min. The time lag by time zone is as
shown in Fig. 4.
The peak of time lag at Hospital A is shown at 6
AM (152.5 min), 10 AM (309.7 min), and 7 PM
(251.1 min); this peak is the same as the frequency
peak of taking VS. The peak of time lag at Hospital
B is shown at 2 AM (6.0 min) ; the peak differs from
the frequency peak of taking VS.
3.3 Content of Nursing Documentation
At Hospital A, all process records were analyzed;
which category does belong each lines of process
records. Of all process records, 2.6% were regarding
BP, 3.5% were regarding BT, 2.2% were SpO2,
1.9% were combined multiple source VS data (e.g.,
both BP and BT), and 89.8% were other parameters
(Fig. 5).
Figure 5: Contents of Nursing Documentation at Hospital
A.
For BP documentation, no peak of
documentation was observed. For BT documentation,
four peaks were observed at 6 AM (6.9% of all
documentation), 10 AM (3.9%), 4 PM (5.3%), and 6
PM (5.3%). For SpO2, two peaks were observed at
10 AM (3.2%) and 6 PM (2.8%).
4 DISCUSSION
4.1 Good Clinical Practice for
Collection of Vital Signs and
Accurate Completion of
Documentation
This study shows similar trends on taking VS at
Hospitals A and B because the frequency peak when
VS was taken at each hospital was the same. This
Nursing Documentation Improvement at Post-Acute Care Settings
165

trend may depend on the nurses’ working shifts: day,
8 AM–5 PM; evening, 4 PM–1 AM; and night, 0
AM–9 AM. Therefore, most nurses take VS as part
of their routine work schedule, i.e., twice during the
day and once in the evening and at night.
The importance of VS documentation has been
well discussed over the last 30 years (McCall, 1982).
In addition, precision in taking VS is very important
for maintaining the nursing quality of care. Missing
VS is a very serious omission; however, it occurs
from time to time (Grave, 2006). Therefore, to avoid
missing VS, we must discuss two issues (1) what is
the appropriate frequency for taking VS and (2) how
long does it take for this documentation to reach
EMR.
Issue (1) is not easy because the evidence for
proper frequency of taking VS is insufficient. In a
previous study, the frequency interval for measuring
VS was discussed at an emergency department (ED),
and BP documentation in ED was completed every
2.3 h for all patients (Miltner, 2014). Other studies
suggested that, complete VS documentation (BP, BT,
SpO2, and respirator rate) during every shift was
only completed for 17% of the recommended
intervals in 3 post-operative day (POD) and only for
5.6% in 7 POD (McGain, 2008).
In our study, VS was recorded every 4–9 h
during the day and 9–11 h during the night in
Hospitals A and B. This frequency of taking VS may
be sufficient, because the hospitals is post-acute care
settings.
Although Hospital A frequently measures VS,
the hospital has a huge risk of missing VS because
Hospital A has very long time lag (>3 h) between
taking VS and documentation reaching EMR.
Therefore, if a nurse at Hospital A takes VS in the
morning, other care staff will have VS of the patient
by afternoon. With respect to missing VS, it is
recommended not to clog the system with frequent
measuring of VS but to focus on improving the time
lag between measuring VS and documentation
reaching EMR at post-acute care settings.
4.2 Effectivity of Reducing Time Lag
using ADS
The solution for reducing missing VS has been
investigated in many studies. The basic approach is
to improve work flow on taking VS. In a previous
qualitative study, EMR was observed to be timelier
than paper-based documentation (Yeung, 2012). In
another study, user interface improvement on EMR
significantly reduced VS documentation but not
completely (Gerdtz, 2013). Whether VS
documentation is paper based or computerized and
PC based or tablet based, time lags will occur if
documentation is completed by people as opposed to
integrated data collection devices.
The second approach is role sharing. In a
previous study, routine observation and
documentation was performed by technicians (not
registered nurses) with tablet–PC (Wager, 2010).
Although effectiveness is limited, other benefits
could be considered because nurses at post-acute
care settings observe not only VS but other patient
parameters as well.
The third approach is integrating EMR and VS
recording devices. This approach was reported 10
years ago in the US, reducing nursing
documentation time (Arora, 2005). However, it is
very hard to use a VS monitor in all post-acute
patients. This policy of “automatic documentation”
is very realistic but an easier method is required in
the post-acute care setting as opposed to that
required for an ED.
In this study, it was found that ADS can reduce
time lag from 208.2 min to 3.2 min (98.5%). This
has a very clear and effective impact not only on
time lag but also on patient safety. Therefore, ADS
is strongly recommended to be implemented for
post-acute care settings as well as for EDs and acute
hospitals.
4.3 Maintaining Quality of Nursing
Documentation at Post-Acute Care
Settings
Reducing time lag is very important. Thus, we
should consider other types of documentation.
Our results demonstrated that the percentage of
VS documentation of all nursing documentation at
Hospital A was 10.2%. However, this rate varies
with time zone; nevertheless, the rate is part of the
routine workload schedule and is not affected by the
current patient conditions. Therefore, an ADS
system will not reduce the quality of documentation
on other aspects of patient care. Rather, currently,
many nurses cannot access patient information in a
timely manner because of the long time lag.
Although many nurses are forced to complete the
documentation, it may not be useful because it may
arrive in the system too late. This situation is known
as “death by data entry” and affects employees’
satisfaction (O’Brien, 2015).
VS are so fundamental that it should be
standardized. But other topics in post-acute care is
on progress in standardization. For example, in
oncology nursing at home, observation points were
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
166
well discussed and standardized. A database system
that can improve nursing documentation has been
reported (Turner, 2015). Because standardization in
nursing is rapidly progressing, if technology could
be improved to measure other parameters associated
with patient subjective symptoms (e.g., nausea and
pain), ADS for post-acute care settings could be
utilized for a broader range of nursing
documentation that is designed in part with the
nurses’ input to maintain the quality of
documentation (Fig. 6).
Figure 6: ADS Scheme of the Future (For Post-Acute Care
Settings).
5 CONCLUSIONS
Nursing documentation without ADS has a very
long lag of over 3 h between the collection of VS
and reaching EMR. The current frequency intervals
of collecting VS are sufficient in the acute and post-
acute hospitals. Moreover, >10% of progress notes
contained information on VS.
As a means to improve patient safety in elderly
care, ADS is very effective and implementing it is
recommended even for use in post-acute care
facilities such as “Care-Mixed Hospital”, nursing
home and skilled care facility.
ACKNOWLEDGEMENTS
This study was supported by a research grant of The
Health Care Science Institute, Japan.
REFERENCES
Romano C, McCormick KA, McNeely LD., 1982. Nursing
documentation: a model for a computerized data base.
ANS Adv Nurs Sci. Jan;4(2), pp.43-56.
Curran MA, Curran KE, Cody WK., 1994. Homeless
patients: designing a database for nursing
documentation. Proc Annu Symp Comput Appl Med
Care , pp.1017.
McCartney P., 2013, Evidence on electronic health record
documentation time. MCN Am J Matern Child Nurs.
;38(2 ), pp.121.
Asaro PV, Boxerman SB., 2008. Effects of computerized
provider order entry and nursing documentation on
workflow. Acad Emerg Med ;15(10), pp.908-15.
Richardson KJ, Sengstack P, Doucette JN, Hammond WE,
Schertz M, Thompson J, Johnson C. 2015. Evaluation
of Nursing Documentation Completion of Stroke
Patients in the Emergency Department: A Pre-Post
Analysis Using Flowsheet. Comput Inform Nurs,
Epub.
Ranegger R, Hackl WO, Ammenwerth E., 2015.
Implementation of the Austrian Nursing Minimum
Data Set (NMDS-AT): A Feasibility Study. BMC Med
Inform Decis Mak. ;15(1), pp.75.
Read-Brown S, Sanders DS, Brown AS, Yackel TR, Choi
D, Tu DC, Chiang MF., 2013. Time-motion analysis of
clinical nursing documentation during implementation
of an electronic operating room management system
for ophthalmic surgery. AMIA Annu Symp Proc;
pp.1195-204.
Hill H, Evans JM, Forbat L., 2015. Nurses respond to
patients' psychosocial needs by dealing, ducking,
diverting and deferring: an observational study of a
hospice ward. BMC Nurs. ;14: 60.
Min YH, Park HA, Chung E, Lee H., 2013.
Implementation of a next-generation electronic
nursing records system based on detailed clinical
models and integration of clinical practice guidelines.
Healthc Inform Res.;19(4), pp.301-6.
Mead CN, Henry SB. 1997, Documenting 'what nurses
do'--moving beyond coding and classification. Proc
AMIA Annu Fall Symp. pp.141-5.
Dehghan M, Dehghan D, Sheikhrabori A, Sadeghi M,
Jalalian M., 2013. Quality improvement in clinical
documentation: does clinical governance work? J
Multidiscip Healthc. ; 6, pp.441-450.
Collins SA, Cato K, Albers D, Scott K, Stetson PD,
Bakken S, Vawdrey DK., 2013. Relationship between
nursing documentation and patients’ mortality. Am J
Crit Care ;22(4), pp.306-313.
Lampe SS., 1985. Focus charting: streamlining
documentation. Nurs Manage ; 16(7), pp.43-46.
Lees L., 2010. Improving the quality of nursing
documentation on an acute medicine unit. Nurs Times
;106(37), .22-26.
McCall P, O'Sullivan PS., 1982. Vital sign documentation
and primary nursing in the emergency department.
Emerg Nurs.; 8(4):187-90.
Nursing Documentation Improvement at Post-Acute Care Settings
167

Grave J, Opatrny J, Gouin S., 2006. High rate of missing
vital signs data at triage in a paediatric emergency
department. Paediatr Child Health; 11(4), 211-215.
Miltner RS, Johnson KD, Deierhoi R., 2014. Exploring the
frequency of blood pressure documentation in
emergency departments. J Nurs Scholarsh ;46(2),98-
105.
McGain F, Cretikos MA, Jones D, Van Dyk S, Buist MD,
2008. Opdam H, Pellegrino V, Robertson MS, Bellomo
R. Documentation of clinical review and vital signs
after major surgery. Med J Aust.; 189(7), .380-383.
Yeung MS, Lapinsky SE, Granton JT, Doran DM,
Cafazzo JA., 2012. Examining nursing vital signs
documentation workflow: barriers and oortunities in
general internal medicine units. J Clin Nurs; 21(7-8),
975-82.
Gerdtz MF, Waite R, Vassiliou T, Garbutt B., 2013.
Prematunga R, Virtue E. Evaluation of a multifaceted
intervention on documentation of vital signs at triage:
a before-and-after study. Emerg Med Australas. 25(6),
580-587.
Wager KA, Schaffner MJ, Foulois B, Swanson Kazley A,
Parker C, Walo H., 2010. Comparison of the quality
and timeliness of vital signs data using three different
data-entry devices. Comput Inform Nurs ;28(4), 205-
212.
Arora M, Falsafi N, Al-Ibrahim M, Sawyer R, Siegel E,
Joshi A, Finkelstein J., 2005. Evaluation of CoViSTA–
an Automated Vital Sign Documentation System–in an
Inpatient Hospital Setting. AMIA Annu Symroc; 2005:
885.
O’Brien A, Weaver C, Settergren TT, Hook ML, Ivory
CH., 2015. EHR Documentation: The Hype and the
Hope for Improving Nursing Satisfaction and Quality
Outcomes. Nurs Adm Q.; 39(4), .333-339.
Turner A, Stephenson M., 2015. Documentation of
chemotherapy administration by nursing staff in
inpatient and outpatient oncology/hematology
settings: a best practice implementation project. JBI
Database System Rev Implement Rep.; 13(10), .316-
334.
ICT4AWE 2016 - 2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health
168
