
Assessment of Relative Technical Efficiency of Small Mental Health
Areas in Bizkaia (Basque Country, Spain)
Nerea Almeda
1
, Carlos García-Alonso
2
, José Alberto Salinas-Pérez
2
, Mencía R. Gutiérrez-Colosía
1
and Luis Salvador-Carulla
3
1
Universidad Loyola Andalucía, Department of Psychology, Seville, Spain
2
Universidad Loyola Andalucía, Department of Quantitative Methods, Seville, Spain
3
University of Sydney, Mental Health Policy Unit, Brain & Mind Research Institute, Sydney, Australia
Keywords: Relative Technical Efficiency, Monte-Carlo DEA, Simulation, Data Envelopment Analysis, Expert
Knowledge, Decision Support Systems, Operation Research in Health, Small Mental Health Areas.
Abstract: Mental disorders cause an enormous burden to society. Considering the current economic context, an efficient
use of scarce inputs, with an appropriate outcome production, is crucial. This situation defines a classical
Relative Technical Efficiency (RTE) problem. A well-known methodology to assess RTE is the Data
Envelopment Analysis, although it presents some limitations. These may be overcome through a hybrid
strategy that integrates Monte-Carlo simulation and artificial intelligence. This study aims to (1) design of a
Decision Support System for the assessment of RTE of Small Mental Health Areas based on DEA; and (2)
analyse 19 mental health areas of the Bizkaian Healthcare System (Spain) to classify them and to identify
potential management improvements. The results have showed higher global RTE in the output-oriented
orientation than in the input-oriented one. This suggests that a decision strategy based on improving the input
management, within the ranges of the expert-driven model of community healthcare, could be appropriate. A
future research line will focus our attention on the validation process through the analysis of micro-
management interventions and their potential impacts in the real system.
1 INTRODUCTION
The current high levels of mental disorders
prevalence cause an enormous burden to the society
and a devastating impact on health and economy
(WHO, 2003). The factors involved in the
development of these psychopathologies are not only
individual features; social, economic and political
determinants, such as national policies and
community support, have also a relevant influence in
the manifestation of the symptomatology (WHO,
2016).Unfortunately, in high-income countries, 35%-
50% of people who suffer mental disorders do not
receive any treatment; in middle and low-income
countries, this percentage increases till 76%-85%
(WHO, 2016).
To face this problem, the World Health
Organization (WHO) and United Nations (UN) are
carrying out specific macro-level strategies. Firstly,
the WHO designed a ‘Mental Health Action Plan
2013-2020’ (WHO, 2013), in which was emphasized
the importance of assessing the evidence and
developing a deeper research. In addition, this action
plan highlighted the provision of health and social
care from a community-based perspective. On the
other hand, the UN is also supporting the shifting of
mental health treatments from hospital to community-
based care (United Nations, 1991). The community-
based mental health care is focused on caring for
individuals with mental illness from institutional
environments to the community (Moran & Jacobs,
2013; Shen & Snowden, 2014). This paradigm of
intervention presents better outcomes and is more
cost-effective than institution-based care (Gutierrez‐
Recacha, Chisholm, Haro, Salvador‐Carulla &
Ayuso‐Mateos, 2006; WHO, 2005;). According to
this model, an increase in outpatient and day care
services and a decrease in inpatient services is
expected. Therefore, the integration of care and
treatment in general hospitals and primary care as
well as the collaboration between professionals and
informal care providers is fundamental.
In Spain, both the Mental Health Strategy of the
Spanish National Health System (Ministerio de
Almeda N., Garcà a-Alonso C., Alberto Salinas-PÃl’rez J., R. GutiÃl’rrez-Colosà a M. and Salvador-Carulla L.
Assessment of Relative Technical Efficiency of Small Mental Health Areas in Bizkaia (Basque Country, Spain).
DOI: 10.5220/0006195603770384
In Proceedings of the 6th International Conference on Operations Research and Enterprise Systems (ICORES 2017), pages 377-384
ISBN: 978-989-758-218-9
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
377

Sanidad, Política e Igualdad, 2011) and the ‘Strategy
for tackling the challenge of chronic illness in the
Basque Country’ (Gobierno Vasco, 2011) are now
being developed, among others, for handling
chronical diseases. The main goals of these strategies
and policies are the promotion of mental health, the
provision of care, the enhancement of the recovery
and the reduction of morbidity and disability.
Regarding economics issues, even though a
political responsiveness to burden of mental disorders
is consolidated, the amount of resources destined to
mental health care depends on the “health” of the
economy (Shen & Snowden, 2014). Public mental
health services are highly vulnerable to resources
constraints in compromising economic situations
(Shen & Snowden, 2014). In Spain (2010), according
to the Organization for Economic Cooperation and
Development (OECD), 9% of the Gross Domestic
Product (GPD) was destined to expenditures on
health (OECD, 2010). Mental disorders absorbed an
expense of 46 billion euros (Parés-Badel el al., 2014).
Taking into account the relevance their increasing
prevalence and the involved amount of public
resources, always scarce, an efficient mental health
care system is absolutely crucial in the present
economic situation.
Research and empirical evidences are decisive
elements for designing suitable mental health policies
and, in consequence, improving quality of care.
Identification and assessment of potential
improvements in the system can be used in designing
of new strategies for enhancing efficiency scores of
mental health services in real contexts. Policy
makers’ decisions are usually based on their clinic
experience and thus the decisional risk is pretty high
taking into account the high uncertainty level: inner
and systemic. In the current economic situation, risks
could be reduced using Decision Support Systems.
These tools can help decision makers to have a better
understanding of mental health services performance
in a real, dynamic and uncertain context. The lack of
previous information and empirical evidence about
the potential trade-offs (costs and outcomes) between
different policy options, severely affects the selection
of the most “suitable” decision in a specific
management situation: the “what could or should
happen if… problem”.
The maintenance of the essential balance between
the quality of public mental health services and their
financial sustainability is the next challenge. This not
necessary means that a mental health system should
maximize its outcomes while maintaining the amount
of the consumed resources or, sometimes even worst,
reducing them. The key question is the optimization
of the balance between inputs and outputs in a
complex, interrelated and dynamic system under
uncertainty. Sherman (1984) introduced Data
Envelopment Analysis (DEA) for assessing hospital
Relative Technical Efficiency (RTE). Nowadays,
there is a growing interest in the evaluation of RTE in
health systems (Färe, Grosskopf, Lundström & Roos,
2008; Hollingsworth, 2008; Hollingsworth & Parkin,
2001; Kaya & Cafrı, 2015; Pelone et al., 2012;), but
little is known about it in mental health (Torres-
Jiménez et al., 2015; Tyler, Ozcan & Wogen, 1995;).
Although DEA models have been successfully
applied in health, several relevant drawbacks of this
analysis have been identified in the literature
(Salvador-Carulla et al., 2007; Zhu, 2013): (i)
frequently decision makers have difficulties in
interpreting DEA results, (ii) DEA models are not
appropriate for analysing datasets with low number of
decision making units (observations) and high
number of inputs (usually resources) and outputs
(outcomes of the system), (iii) the management of the
inner uncertainty of the real systems is statistically
complicated (Monte-Carlo simulation) and very
computer demanding and, finally, (iv) real data values
(inputs and outputs) have to be interpreted according
to expert knowledge for avoiding biased results (this
process needs to formalise explicit knowledge in a
knowledge-base).
The main goals of the current research are: 1. The
design of a Decision Support System for the
assessment of RTE of Small Mental Health Areas
based on DEA; and 2. The analysis of 19 mental
health areas of the Bizkaia (Spain) Healthcare System
for identifying potential performance improvements.
2 METHODS
2.1 Inputs, Outputs and
Decision-making Units
Original data were collected from “Mental Health
Atlas of Bizkaia” (Pereira, Gutiérrez-Colosía &
Salinas-Pérez, 2013). In total, the dataset included 52
variables, 39 inputs and 13 outputs, which described
the Mental Health Care System in Bizkaia (Spain).
This system is structured in 19 Small Health Care
Areas that were identified as Decision Making Units
(DMU) (19×52 data matrix). The variables were
coded into main types of care (Table 1) according to
the DESDE-LTC codification system (Salvador-
Carulla et al., 2011) and each code was classified
based on the Basic-Mental Health Community Care
(B-MHCC) paradigm (Salvador-Carulla et al., 2007)
ICORES 2017 - 6th International Conference on Operations Research and Enterprise Systems
378

in the following variable groups: service availability,
amount of places or beds, amount of professionals
and service utilization. Variable values were
transformed into rates per 100,000 population. Health
planers and policymakers validated the variable
(inputs and outputs) set (Table 1).
In order to assess the RTE of the selected areas,
15 scenarios were designed. Each scenario is a set of
variables (a meaningful combination of inputs and
outputs), which describes a specific type of care or a
combination of them selected by experts in mental
health care (Table 2). Thus, these scenarios allow to
study different perspectives of the management and
evolution of the system. By integrating the proposed
scenarios, the Decision Support System offers both
the RTE for any area in each scenario as well as the
global RTE of the system.
Table 1: List of inputs/outputs analyzed for each group of
main types of care (DESDE-LTC) and scenario assigned.
Table 2: Description of the scenarios.
The variables in each scenario were selected by
applying two criterions:
1. Methodological: For developing highly
discriminating DEA models (Alirezaee, Howland &
VandePanne, 1998; Dyson et al., 2001; Staat, 2001;
Torres et al., 2015) the number of variables have to
be controlled (2×(I×O)≤DMU, being I the number of
inputs, O the number of outputs and DMU the original
number of observations, 19 in this case).
2. Technical: All of the scenarios have to be
meaningful for managers and policy makers.
According to this principle, results obtained are easy
to interpret and facilitate the identification of
potential improvements that can be used to design
new real interventions and policies.
For better understanding the inner uncertainty of
the system, each variable value was transformed in a
standard statistical distribution (symmetric triangular
T[minimum value, central estimator, maximum
value] in this case). Therefore, the original 19×52
data matrix was transformed in a 19×52 statistical
distributions matrix. The structure and parameters of
these statistical distributions were selected by a panel
of experts including managers and policy makers
(Torres et al., 2015).
2.2 The Monte Carlo DEA Model and
the Decision Support System (DSS)
A hybrid model was used to assess the RTE of the
small mental health care areas in Bizkaia. This model
integrates classical statistics, mathematical
programming and an approximation to artificial
intelligence. Regarding classical statistics, Monte-
Carlo simulation was used: (1) to incorporate
Assessment of Relative Technical Efficiency of Small Mental Health Areas in Bizkaia (Basque Country, Spain)
379

uncertainty in variable measuring by using statistical
distributions rather than the original variable values
(i.e. the original value 0.299 was transformed into
triangular distribution T[0.2691, 0.299, 0.3289] and
(2) to artificially multiply the number observations
(500 replications of each area and scenario) which
makes RTE analysis be more discriminant. In the
proposed model, the Monte-Carlo engine allows the
simulation of inputs and outputs and offers the
statistical distribution of the RTE for each area in
each scenario and, by extension, the corresponding
one for the global system (Torres-Jiménez et al.,
2015).
Once inputs and outputs values were produced by
the Monte-Carlo engine, they are mathematically
(linear monotone increasing/decreasing functions)
interpreted based on expert knowledge formalised in
a IF … THEN … rule-base (knowledge-base), an
embryo of a fuzzy inference engine (Torres-Jiménez
et al., 2015). The rule design was based on the B-
MHCC paradigm (Salvador-Carulla et al., 2007).
Finally, and using the transformed variable
values, the operational algebraic model was designed
and solved. The BCC-DEA model, variable returns to
scale, was selected because there is no evidence of a
constant returns to scale rigid behaviour (Salvador-
Carulla et al., 2007). Both input and output
orientations of the BCC-DEA model were used. Input
orientation refers to maintaining a stable level of
outputs, while trying to minimize the resources
utilized. Output orientation aims to maximize the
outcomes for a constant amount of inputs.
In conclusion, for each scenario and BCC-DEA
orientation, the Decision Support System analysed 20
times (or repetitions) a 19×25×V (being: 19 the
number of areas, 25 the number of simulations and V
the number of variables –inputs and outputs- in the
corresponding scenario) datasets. The number of
simulations and repetitions was controlled by the
Nakayama’s error (Torres-Jiménez et al., 2015) that
should always be lower than 2.5% over the RTE
average.
RTE for each area (19), scenario (15) and
orientation (2) has a probabilistic structure that can be
statistically studied. By aggregation, the global RTE
of the system can also be statistically determined and
studied.
3 RESULTS
The results of the analysis showed the statistical RTE
assessment of mental health services provision and
use in 19 Bizkaia’s small areas. 15 different technical
Figure 1: Box-plots of input-oriented relative technical
efficiency of mental health areas for each scenario.
Figure 2: Box-plots of output-oriented relative technical
efficiency of mental health areas for each scenario.
perspectives (scenarios) of the RTE problem were
taken into account in addition to the two BCC-DEA
orientations: input and output. The analysis of the
resulting RTE statistical distributions allowed to: (1)
rank the areas, and (2) identify and assess potential
improvements in key variables by using a
benchmarking process (the area that showed the best
RTE average and the bigger probability of being
efficient is considered the benchmark).
In DEA models, a RTE equal to 1 means that the
analysed DMU is efficient (when the sum of the
slacks is equal to 0) or weak efficient (when the sum
of the slacks is greater than 0). Values lower than 1
show different levels of inefficiency, the lower the
value the lower the efficiency. Figures 1 and 2 plot
the minimums, maximums, confidence intervals
(two-tailed t-Student, α=0.95 and 29 freedom
degrees), averages and outliers of the resulting ETR
ICORES 2017 - 6th International Conference on Operations Research and Enterprise Systems
380
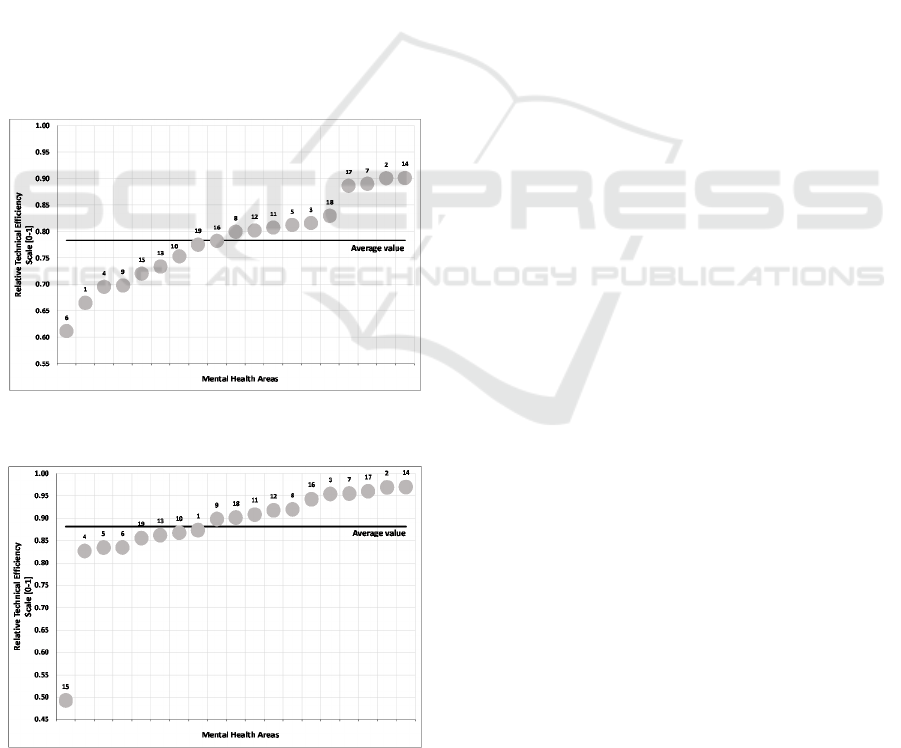
statistical distributions for each scenario (S#) in both
the input and output orientations.
The input orientation shows a less number of
outliers than the output one. The differences between
areas are greater in S1 and S6 to S15 in both
orientations, S2 to S5 have a relative homogeneous
behaviour.
The mental health areas 4, 6 and 11 appear in three
scenarios as outliers in the input-oriented model. On
the other hand, areas 6 and 15 are the most recurring
as outliers in the output-oriented model. Thus, the
area 6 can be considered as a RTE outlier. The area
15 is also an outlier in the most output-oriented
scenarios because of several missing data (highly
penalised in DEA models) because a private health
organization manages this area under contract
agreements with the public health system so its
information is not integrated.
The most efficient areas reach RTE average
values greater than 0.85 in most scenarios and in both
orientations. The worst RTE average values are lower
than 0.7 in the input orientation a 0.85 in the output
one (Figures 3 and 4).
Figure 3: Ranking of mental health areas for the input-
oriented model.
Figure 4. Ranking of mental health areas for the output-
oriented model.
The global input-oriented RTE average is 0.78
(Figure 3). Four areas have a RTE average values
greater than 0.85, while the lowest value is around
0.6. In the output-oriented model (Figure 4), results
are more homogenous and the RTE average is 0.88.
There are five areas above 0.95 and an outlier (area
15) close to 0.5 (due to its missing values).
4 DISCUSSION
4.1 The Monte Carlo DEA Model and
the Decision Support System (DSS)
The Monte-Carlo DEA model overcomes several
limitations of the traditional DEA models. Firstly, the
expert-based interpretation of input and output values
makes the result interpretation easier for decision
makers (Salvador-Carulla et al., 2007; Torres-
Jiménez et al., 2015) because it includes the specific
interrelations and particular characteristics of mental
health systems. For instance, the classical
assumption: “a situation which combines a low input
consumption with a high outcome production is
positive for the system performance” may not be
always correct or appropriate in mental health care
(Torres-Jiménez et al., 2015). Expert knowledge is
formalised in a rule-base by using the B-MHCC
paradigm (Salvador-Carulla et al., 2007), which
determines an appropriateness degree for each
variable value (“non-appropriate” values are
penalised in their mathematical transformation).
Secondly, the Monte-Carlo DEA model makes
RTE assessment more discriminant by the artificial
replication of the observation number. Datasets are
generated by the Monte-Carlo engine according to
variable values statistical distributions.
Finally, the uncertainty associated to data real
values is managed through the transformation of the
original variable values into standard statistical
distributions. The Monte-Carlo simulation engine
explores the variable values spectrum and offers a
RTE probabilistic view.
4.2 Strengths of the Study of the
Relative Technical Efficiency in
Bizkaia
Previous RTE studies have mainly assessed the
efficiency of complete systems (Kaya Samut & Cafrı,
2015); specific services, such as nursing homes
(Garavaglia, Lettieri, Agasisti & Lopez, 2011;
Kleinsorge & Karney, 1992), hospitals (Dash,
Assessment of Relative Technical Efficiency of Small Mental Health Areas in Bizkaia (Basque Country, Spain)
381

Vaishnavi, & Muraleedharan, 2010; Mogha, Yadav &
Singh, 2016) or primary care (Cordero et al., 2015;
Kirigia et al., 2011). However, they have not allowed
to know performance differences within the whole
health system. This research has studied different
RTE scenarios designed to describe the behaviour of
both the partial (i.e. residential care) or mixed (i.e.
day and outpatient care jointly) typologies based on
the B-MHCC paradigm. Thus, these scenarios
incorporate an integrative vision of mental health
care, including all the types of care (from a holistic
perspective) in which health and social care are
highlighted. This fact lets us to understand and assess
specific mental health care itineraries that patients
should follow in order to increase RTE and quality
care. Results include all the RTE statistical
distributions as well as the global RTE of the system.
This study has analysed the provision and
utilisation of mental health services in a real system
through an exhaustive data collection from the
Integrated Mental Health Atlas of Bizkaia (Pereira et
al., 2013; Salvador-Carulla et al., 2011). The use of a
standardized model for mental-health care
description and assessment was absolutely essential
because the name of the service was not enough for
describing its management structure and for making
comparisons. The Mental Health Atlas collected
information about the availability of specific types of
care, placement capacity, availability of workforce
and utilization indicators. The Monte-Carlo DEA
model integrates the uncertain information with an
operational model for assessing RTE and potential
managerial improvements.
4.3 Analysis of the Mental Health
System RTE in Bizkaia
Efficient mental health areas may be identified as
references for benchmarking. The assessed potential
improvements can guide management interventions
on the provision (inputs) and outcomes (outputs). On
one hand, the provision of mental health care in
inefficient areas could be adjusted to the values of the
efficient ones. On the other, interventions on the
service utilization could be direct such as the
optimization of facilities, placements and staff; or
indirect such as economic incentives, training
activities, policy design or good practices promotion.
The global RTE of the system is greater in the
output-oriented model than in the input-oriented one.
This suggests that a decisional strategy based on
optimizing the input amount, within the ranges
stablished by the B-MHCC paradigm, may be more
adequate for the Mental Health System of Bizkaia.
In the input-oriented analysis and in spite of the
existence of outliers, the scenarios where the RTE
scores are more homogenous are those that evaluated
the residential non-acute care and day hospitals (S2 to
S5 and, by extension, S13). This characteristic is the
result of the current and careful political planning.
Obviously, RTE scores can be improved in each
scenario by designing specific policies, especially on
the outlier areas.
In the output-oriented analysis (more
homogeneous), the most efficient scenarios are S11
and S12 (community mental health 1 and 2) and S4
(health-related day care). According to the results, S2
(non-acute residential and hospital care), S3
(residential care), S5 (non-health-related day care)
and s6 (outpatient care) could be main the targets in a
decisional environment based on the improvement of
the RTE. In this DEA orientation, the area number 15
has a relevant impact on the RTE scores because it
was a highly penalised due to the lack of information.
It is highly recommended to increase the day care
resources to be equal, at least, to medical ones. This
intervention should increase both the RTE and the
mental health care quality, in addition to an expected
decrease in the economic burden of the system. In this
sense, there are empirical evidences that show that
community-based care is more cost-effective than
institutional-based care (WHO, 2005).
The proposed DSS can assess the impact of an
almost infinite number of planning interventions.
This process can decrease the intrinsic managerial
risk associated to any real management decision. For
example, it can evaluate the effects on the system of
transferring some professionals from a mental health
area, or areas, to other/s: this implies changes in the
provision, utilization and outcome variables. This
analysis understands that any intervention in a
specific geographical area will probably have an
impact on the others because of the interrelations
between them.
4.4 Limitations
The analysis of RTE in specific mental health areas is
relevant and useful but insufficient to evaluate the
global situation of mental health care. The pathway of
care that should be followed by a specific user has to
be designed depending on his clinic status. In Spain,
the first point of contact in the health care system is
usually located in a primary care service or in a
hospital. From these units, the patient can be derived
to a secondary care service afterwards. All the
mentioned services have been include in this study.
Nevertheless, until the patient arrives to this
ICORES 2017 - 6th International Conference on Operations Research and Enterprise Systems
382

secondary level, he has followed an itinerary that
ought to be studied if RTE scores have to be
increased. To avoid an increase in the re-
hospitalization number, in the number of stays at the
hospitals, in the frequentation, the prevalence or even
in the incidence of mental disorders, a most efficient
care coordination and an integrative professional
practice have to be highlighted (Burns, Goldsmith, &
Sen, 2013; Cordero et al., 2015).
In conclusion, it should be necessary to include
primary care services in RTE assessment in order to
have a complete picture of the mental health system
under analysis.
5 CONCLUSIONS
In the decision making processes based on empirical
evidence, the intrinsic decisional risk decreases.
Therefore, it is fundamental to provide the decision
maker as much reliable information as possible to
understand the real situation (Gibert, García-Alonso
& Salvador-Carulla, 2010).
The Monte-Carlo DEA model has provided high-
level and empirical informed-evidence on the RTE
based on the provision and utilization of mental
health services in small geographical areas of the
Bizkaian Health System. Based on the results, it has
been possible to identify and analyse potential
improvements that can be transformed into decisional
interventions to be checked by modifying input or
output values (statistical distributions) in the DSS.
The obtained results may help decision makers to
prioritise them in an uncertain context dominated by
economic restrictions.
Future research will be focused on the validation
of the DSS analysing real decisional situations with
multiple feasible alternatives. Selected micro-
management interventions, those that imply a relative
small number of variables, based on policymaker
interests will be selected to assess potential
improvements and risks on the system management
prior their implementation, Following this process,
the decision making process is supported by empirical
evidence. This feature matches with the strategies
established in the Mental Health Action Plan 2013-
2020 (WHO, 2013).
ACKNOWLEDGEMENTS
This study is part of a bigger Project named “Atlas de
Salud Mental de Bizkaia” funded by the “Red de
Salud Mental de Bizkaia”. It has been carried out in
collaboration with “Osakidetza” and the
“Departamento de Sanidad y Consumo del Gobierno
Vasco”.
REFERENCES
Alirezaee, M.R., Howland, M. & Van de Panne, C., 1998.
Sampling size and efficiency bias in data envelopment
analysis. Journal of Applied Mathematics and Decision
Sciences, 2(1), pp.51-64.
Burns, L.R., Goldsmith, J.C. & Sen, A., 2013. Horizontal
and vertical integration of physicians: a tale of two tails.
Advances in health care management, 15, pp.39–117.
Cordero, J.M. et al., 2016. Technical efficiency assessment
of public primary care providers in the Basque Country
(Spain), 2010-2013. Gaceta Sanitaria, 30(2), pp.104–
109. Available at:
http://www.scopus.com/inward/record.url?eid=2-s2.0-
84959099383&partnerID=40&md5=3043220dd789be
1b3dd178769affd73c.
Dash, U., Vaishnavi, S.D. & Muraleedharan, V.R., 2010.
Technical Efficiency and Scale Efficiency of District
Hospitals: A Case Study. Journal of Health
Management, 12(3), pp.231–248. Available at:
http://www.scopus.com/inward/record.url?eid=2-s2.0-
77955896077&partnerID=tZOtx3y1 [Accessed March
14, 2016].
Dyson, R.G. et al., 2001. Pitfalls and protocols in {DEA}.
European Journal of Operational Research, 132(2),
pp.245–259. Available at:
http://www.sciencedirect.com/science/article/pii/S037
7221700001491.
Färe, R. et al., 2008. Evaluating health care efficiency.
Advances in health economics and health services
research, 18, pp.209–228. Available at:
https://www.scopus.com/inward/record.uri?eid=2-
s2.0-
58849144444&partnerID=40&md5=0156be57de9f25
4a68436a2db8b6d62f.
Garavaglia, G. et al., 2011. Efficiency and quality of care in
nursing homes: An Italian case study. Health Care
Management Science, 14(1), pp.22–35. Available at:
https://www.scopus.com/inward/record.uri?eid=2-
s2.0-
79551530621&partnerID=40&md5=eddb9c7279a145
d0f1c32c9181972ff9.
Gibert, K., Garcia-Alonso, C. & Salvador-Carulla, L., 2010.
Integrating clinicians, knowledge and data: expert-
based cooperative analysis in healthcare decision
support. Health research policy and systems / BioMed
Central, 8, p.28.
Gobierno Vasco. (2010). Estrategia para afrontar el reto de
la cronicidad en Euskadi, Bilbao, Eusko Jaurlaritza-
Gobierno Vasco.
Gutierrez-Recacha, P. et al., 2006. Cost-effectiveness of
different clinical interventions for reducing the burden
Assessment of Relative Technical Efficiency of Small Mental Health Areas in Bizkaia (Basque Country, Spain)
383

of schizophrenia in Spain. Acta psychiatrica
Scandinavica. Supplementum, (432), pp.29–38.
Hollingsworth, B., 2008. The measurement of efficiency
and productivity of health care delivery. Health
economics, 17(10), pp.1107–1128.
Hollingsworth, B. & Parkin, D., 2001. The efficiency of the
delivery of neonatal care in the UK. Journal of public
health medicine, 23(1), pp.47–50.
Kaya Samut, P. & Cafrı, R., 2015. Analysis of the
Efficiency Determinants of Health Systems in OECD
Countries by DEA and Panel Tobit. Social Indicators
Research. Available at:
https://www.scopus.com/inward/record.uri?eid=2-
s2.0-
84941367202&partnerID=40&md5=77b2c000e68c3d
32218b73040f075a46.
Kirigia, J.M. et al., 2011. Technical efficiency of primary
health units in Kailahun and Kenema districts of Sierra
Leone. International archives of medicine, 4, p.15.
Kleinsorge, I.K. & Karney, D.F., 1992. Management of
nursing homes using data envelopment analysis. Socio-
economic planning sciences, 26(1), pp.57–71.
Ministerio de Sanidad, Política e Igualdad (2011).
Estrategia en Salud Mental del Sistema Nacional de
Salud 2009-2013 [pdf] España. Avaliable at
http://www.aepcp.net/arc/SaludMental2009-2013.pdf
[Accessed 24 Oct. 2016]
Mogha, S.K., Yadav, S.P. & Singh, S.P., 2015. Slack based
measure of efficiencies of public sector hospitals in
Uttarakhand (India). Benchmarking: An International
Journal, 22(7), pp.1229–1246. Available at:
http://www.scopus.com/inward/record.url?eid=2-s2.0-
84942784709&partnerID=tZOtx3y1 [Accessed March
14, 2016].
Moran, V. & Jacobs, R., 2013. An international comparison
of efficiency of inpatient mental health care systems.
Health policy (Amsterdam, Netherlands), 112(1-2),
pp.88–99. Available at:
http://www.scopus.com/inward/record.url?eid=2-s2.0-
84885191198&partnerID=tZOtx3y1 [Accessed March
14, 2016].
[OECD] Organisation for Economic Co-operation and
Development. (2010). Health expenditures and
financing. [online] Available at:
https://stats.oecd.org/Index.aspx?DataSetCode=SHA
[Accessed 20 Oct. 2016]
[OECD] Organisation for Economic Co-operation and
Development. (2016). Mental Health and work.
[online] Available at:
https://www.oecd.org/els/emp/mental-health-and-
work.htm [Accessed 20 Oct. 2016]
Pares-Badell, O. et al., 2014. Cost of disorders of the brain
in Spain. PloS one, 9(8), p.e105471.
Pelone, F. et al., 2012. The measurement of relative
efficiency of general practice and the implications for
policy makers. Health policy (Amsterdam,
Netherlands), 107(2-3), pp.258–68. Available at:
http://www.scopus.com/inward/record.url?eid=2-s2.0-
84865970504&partnerID=tZOtx3y1 [Accessed March
14, 2016].
Pereira, C., Gutiérrez-Colosía, M. and Salinas-Perez, J.
(Eds.). (2013).
Mental Health Atlas of Bizkaia. Bilbao:
Osakidetza.
Salvador-Carulla, L., Dimitrov, H., Weber, G., McDaid, D.,
Venner, B., Šprah, L., ... and Johnson, S. (2011).
DESDE-LTC: Evaluation and Classification of
Services for Long Term Care in Europe. Spain: Psicost
and Caixa Catalunya.
Salvador-Carulla, L. et al., 2007. Use of an operational
model of community care to assess technical efficiency
and benchmarking of small mental health areas in
Spain. The journal of mental health policy and
economics, 10(2), pp.87–100.
Shen, G.C. & Snowden, L.R., 2014. Institutionalization of
deinstitutionalization: a cross-national analysis of
mental health system reform. International journal of
mental health systems, 8(1), p.47.
Sherman, H.D., 1984. Hospital efficiency measurement and
evaluation. Empirical test of a new technique. Medical
care, 22(10), pp.922–938.
Staat, M., 2001. The Effect of Sample Size on the Mean
Efficiency in DEA: Comment. Journal of Productivity
Analysis, 15(2), pp.129–137. Available at:
http://dx.doi.org/10.1023/A:1007826405826.
Torres-Jiménez, M. et al., 2015. Evaluation of system
efficiency using the Monte Carlo DEA: The case of
small health areas. European Journal of Operational
Research, 242(2), pp.525–535. Available at:
http://www.scopus.com/inward/record.url?eid=2-s2.0-
84920716285&partnerID=tZOtx3y1 [Accessed March
14, 2016].
Tyler, L.H., Ozcan, Y.A. & Wogen, S.E., 1995. Mental
health case management and technical efficiency.
Journal of medical systems, 19(5), pp.413–423.
United Nations. (1991). The protection of person with
mental illness and the improvements of mental health
care. [online] Available at
http://www.un.org/documents/ga/res/46/a46r119.htm
[Accessed 25 Oct. 2016].
World Health Organization. (2003). Investing in MENTAL
HEALTH [online] Available at
http://www.who.int/mental_health/en/investing_in_mn
h_final.pdf [Accessed 25 Oct. 2016].
World Health Organization. (2005). Mental health policy,
plans and programmes. Mental Health Policy and
Service Guidance Package. [online] Available at
http://www.who.int/mental_health/policy/services/esse
ntialpackage1v1/en/ [Accessed 25 Oct. 2016].
World Health Organization. (2013). Mental Health Action
Plan 2013 – 2020. [online] Available at
http://www.who.int/mental_health/publications/action
_plan/en/ [Accessed 25 Oct. 2016].
World Health Organization. (2016). Mental disorders.
[online] Available at
http://www.who.int/mediacentre/factsheets/fs396/en/
[Accessed 25 Oct. 2016].
Zhu, J., 2003. Imprecise data envelopment analysis
(IDEA): A review and improvement with an
application. European Journal of Operational
Research, 144(3), pp.513–529.
ICORES 2017 - 6th International Conference on Operations Research and Enterprise Systems
384
