
Maternal and Neonatal Risk Factors for Hypoglycemia in Preterm
Infants
Bugis Mardina Lubis
1
,
Beby Syofiani Hasibuan
1
1
Faculty of Medicine, Division of Neonatology Department of Child Health, Universitas Sumatera Utara,
Jl.. Dr. Mansyur, Haji Adam Malik General Hospital, Medan, Indonesia
Keywords: Maternal, Hypoglycemia, Preterm Infants, Birth Weight, Gestational Age
Abstract: Hypoglycemia is a common morbidity in preterm infants. It might cause transient and permanent disturbances
in brain structural and have impact on neurological development. The criteria for identifying preterm infants
who are at risk of hypoglycemia remain unclear. This study was conducted to determine incidence of
hypoglycemia in preterm infants and associated with maternal and neonatal risk factors. A cross-sectional
study on 50 consecutive preterm infants on hospitals in Medan, Indonesia from June to August 2018. Maternal
and neonatal risk factors were recorded. Blood glucose levels were obtained from venous blood sample and
were checked serial from the time of delivery within the first hour of life until discharged from hospital or 72
hours of age. Univariate and bivariate (Chi square and Fisher exact test) analysis were performed with 95%
CI and P value <0.05 were considered statistically significant. Out of 50 preterm infants, there were 13 infants
experienced hypoglycemia (26%). Preterm infants with birth weight <2500 gr and 32-<35 weeks of
gestational age were significantly increased the risk of developing hypoglycemia (p=0.010, PR=4.69;
p=0.021, PR= 3.11, respectively). There were significant associations between birth weight <2500 gr and
gestational age 32-<35 weeks with hypoglycemia.
1 INTRODUCTION
Prematurity is one of the highest causes of perinatal
death in addition to low birth weight (LBW) infants,
asphyxia or respiratory disorders. Neonatal mortality
rates in Asia due to prematurity amounted to 413,000
or 30% of total neonatal deaths in 2000-2003.Caring
premature infants is still a challenge. The biggest
challenge is how to reduce the risk of morbidity
which will reduce neurological disorders and long-
term growth and development disorders so that these
preterm infants can grow optimally (Howson, 2012).
One of the most common morbidity in premature
infants is hypoglycemia. The immaturity of the
glucose formation system, inadequate energy storage,
and hyperinsulinism conditions can affect the
occurrence of hypoglycemia, even severe and
recurrent hypoglycemia in preterm infants (Zanardo,
1999).
Symptoms of hypoglycemia in neonates include
jitteriness, convulsions, hypotonia, coma, refusal to
feed, cyanosis, high pitched cry, hypothermia and
even asymptomatic in mostcases. Therefore detection
of hypoglycemia must always be confirmed
biochemically (Dhananjaya, 2011). Hypoglycemia
conditions have an effect on transient and permanent
disturbances in the brain structural and have an
impact on neurological development. (Goode, 2016).
Research on risk factors for hypoglycemia in
premature infants is still limited and shows
controversial results. The purpose of this study is to
determine incidence of hypoglycemia in preterm
infants and associated maternal and neonate risk
factors for hypoglycemia.
2 METHODS
This was a cross sectional study. We examined 50
moderate to late preterm labor infants with 32-36
weeks of gestational age through normal vaginal
delivery and section caesarean. Patients were
obtained consecutively. Minimum sample size
calculated using one population sample formula.
Stillbirth infants and severe congenital abnormalities
were excluded. This study conducted from June to
August 2018 in five hospitals, Adam Malik General
Hospital, Universitas Sumatera Utara Hospital, Stella
924
Lubis, B. and Hasibuan, B.
Maternal and Neonatal Risk Factors for Hypoglycemia in Preterm Infants.
DOI: 10.5220/0010101709240928
In Proceedings of the International Conference of Science, Technology, Engineering, Environmental and Ramification Researches (ICOSTEERR 2018) - Research in Industry 4.0, pages
924-928
ISBN: 978-989-758-449-7
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Maris Mother and Child Hospital, Sarah Hospital, and
Bunda Thamrin Hospital. All hospitals are located in
Medan, Indonesia.
Maternal characteristics such as maternal age,
weight, gravidity and parity, and delivery methods
were recorded as maternal risk factors. Neonate
characteristics such as gender, birthweight,
gestational age, one-minute Apgar score, five-minute
Apgar score were recorded as neonate risk factors.
Blood glucose levels were obtained from venous
blood sample and were checked serial from the time
of delivery within the first hour of life until
discharged from hospital or 72 hours of age. Blood
glucose levels of 40 mg/dL or lower were considered
as hypoglycemia. All patients gave informed consent.
This study was approved by the Institutional Review
Board of Universitas Sumatera Utara. Statistical data
composed of univariate and bivariate were analyzed
using SPSS version 22 (SPSS Inc., Chicago) with
95% confidence interval. The analysis was carried out
using chi square and fisher exact test. P value <0.05
were considered statistically significant.
3 RESULT
3.1 Baseline Maternal Characteristics
of Subjects
Mean of maternal age were 30.9 years with mean of
body weight were 69.3 kgs. A total of 96% gave birth
through cesarean delivery where 58% having medical
indications. There were 54% of premature
infantshadLBW.About66% were 35–37 weeks
ofgestational age. (Table1).
Table 1: Basic maternal characteristicofsubjects.
Characteristics n = 50
Maternal age, years, mean + SD
>31 years
<31 years
30.9 + 5.23
21 (42%)
29 (58%)
Maternal weight, kg, mean + SD
>69 kg
<69 kg
69.3 + 10.87
25 (50%)
25 (50%)
Maternal parity, times, median (min-
max)
>1
1 (0 – 2)
8 (16%)
42
(
84%
)
0
–
1
Delivery, n (%)
Vaginal delivery
Sectiocaesarean
2 (4%)
48 (96%)
Indication of preterm labor, n (%)
Medical indication
Spontaneous
29 (58%)
21 (42%)
Gender, n (%)
Male
Female
25 (50%)
25 (50%)
Birthweight, gram, mean+ SD
<2500
>2500
2,503.5 +
542.21
27 (54%)
23
(
46%
)
Gestational age, weeks, n (%)
32 – <35 weeks
35
–
<37 weeks
17 (34%)
33 (66%)
One-minute Apgar score, n (%)
<3
4-6
>7
1 (2%)
9 (18%)
40
(
80%
)
Five-minute Apgar score, n (%)
<3
4-6
>7
0 (0%)
1 (2%)
49
(
98%
)
n = total numberofsubjects
3.2 Association between Maternal and
Neonate Characteristics with
Hypoglycemia in Preterm Infants
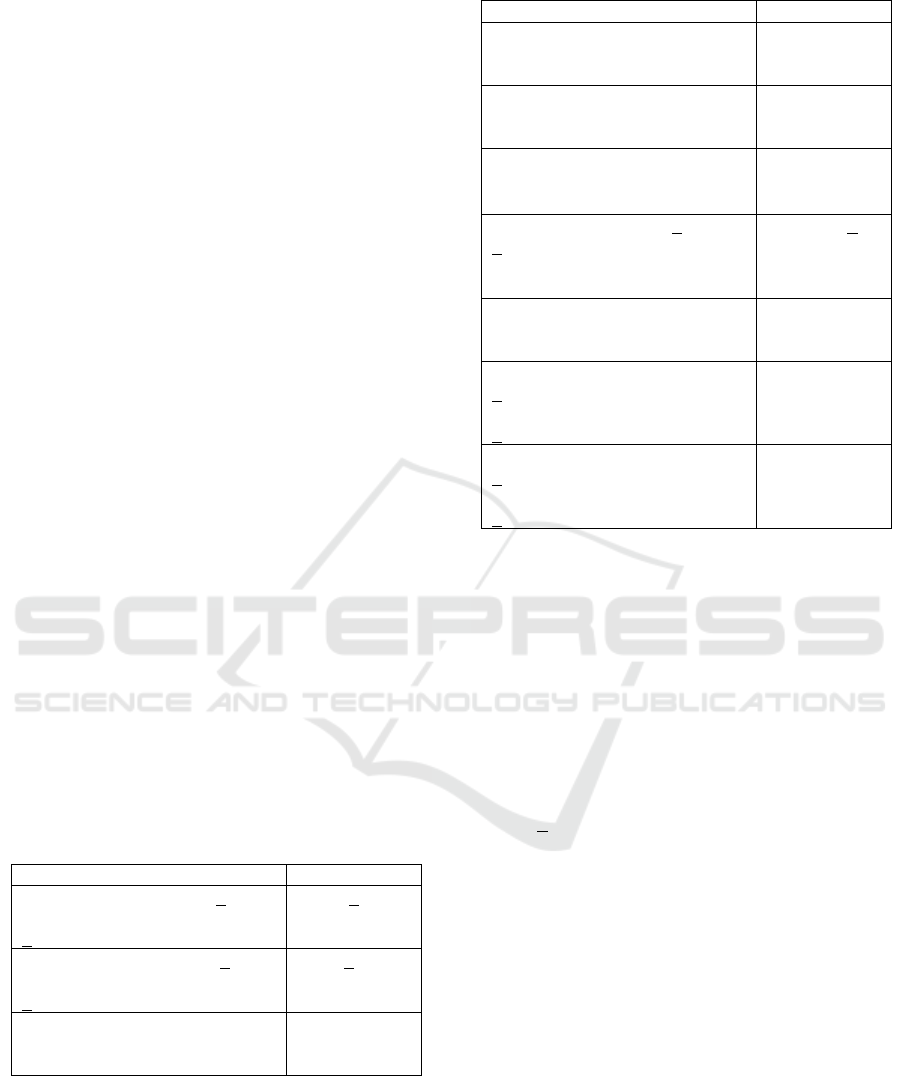
Out of 50 preterm infants, there were 13 infants who
had hypoglycemia (26%). Table 2 showed
association between maternal characteristics and
hypoglycemia in preterm infants. There were
significant association between birth weight and
prematurity with hypoglycemia. Infants with a birth
weight <2500 gr were increasedrisk of 4.69 times
experiencing hypoglycemia compared to birth
weight> 2500 gr (p=0.010). Infants with 32- <35
weeks of gestational age had 3.11 times higher risk to
had hypoglycemia than 35-<37 weeks (p=0.021).
There were no significant association between
maternal age, weight, gravidity, parity, indication of
preterm labor, gender, 1-minute and 5-minute Apgar
score with hypoglycemia in preterm infants.
Maternal and Neonatal Risk Factors for Hypoglycemia in Preterm Infants
925

Table 2: Association Between Maternal and NeonatalCharacteristics with Hypoglycemia in Preterm Infants
*p<0.05
4 DISCUSSION
Hypoglycemia is common in neonates. The lowest
blood glucose level in 2 hours of life which is
generally due to physiological rather than pathological
factors (Sperling, 2012; Mitanchez, 2007; Aggarwal,
2010). Previous studies reported prevalence of
hypoglycemia varied in neonates, approximately15.1-
29.1% (Lodhi, 2006; Dashti, 2007; Osiet, 2003;
Dalgic, 2002). The prevalence of hypoglycemia is
significantly higher in preterm infants. Singh. showed
the prevalence of hypoglycemia in preterm infants and
term infants were 19.05% vs 14.42%
(Singh, 2014).
This recentstudy found theprevalence of
hypoglycemia in preterm infantswas 26%. This
prevalence difference is due to differences in the
definition of hypoglycemia, inclusion criteria, sample
size, and detection method of hypoglycemia.There
were significant association between LBW
andprematuritywith hypoglycemia. Infants with a
birth weight <2500 gr were significantly increased
risk of 4.69 times experiencing hypoglycemia
compared to birth weight> 2500 gr. Infantswith 32 –
<35 weeksofgestationalage were significantly
increased risk of 3.11 times experiencing
hypoglycemia compared to 35 – <37 weeks
ofgestational age. This result is in line with previous
studies (Singh, 2014; Rasmussen, 2007).
Variable
Hypoglycemia Total
n (%)
p
PR
(95% CI)
Yes
n
(
%
)
No
n
(
%
)
Maternal age
0.097
2.21 (0.84-
5.81)
>31 years 8 (38.1) 13 (61.9) 21 (100)
<31 years 5 (17.2) 24 (82.8) 29 (100)
Maternal wei
g
ht
0.747
0.86 (0.34-
2.19)
>69 k
g
6
(
24
)
19
(
76
)
25
(
100
)
<69 kg 7 (28) 18 (72) 25 (100)
Maternal gravidity
>2
1
–
2
2 (15.4)
11
(
29.7
)
11 (84.6)
26
(
70.3
)
13 (100)
37
(
100
)
0.469
0.52 (0.13-
2.03
)
Maternal parity
>1
0
–
1
0 (0%)
13
(
31
)
8 (100)
29
(
69
)
8 (100)
42
(
100
)
0.093
1.45 (1.18-
1.77
)
Indication of preterm
labo
r
0.340
1.63
(0.58 – 4.59)
Medical 9 (31) 20 (69) 29 (100)
Spontaneous 4 (19) 17 (81) 21 (100)
Gender
Male
Female
6 (24)
7
(
28
)
19 (76)
18
(
72
)
25 (100)
25
(
100
)
0.747
0.86
(
0.34-2.19
)
Birthweight
<2,500 gr
>2,500
gr
11 (40.7%)
2
(
8.7%
)
16 (59.3)
21
(
91.3
)
27 (100)
23
(
100
)
0.010*
4.69
(
1.16-19
)
Gestational age
32 – <35 weeks
35 – <37 weeks
8 (47.1)
5 (15.2)
9 (52.9)
28 (84.8)
17 (100)
33 (100)
0.021*
3.11
(1.2-8.05)
One-minute Apgar score
<7
>7
4 (40)
9 (22.5)
6 (60)
31 (77.5)
10 (100)
40 (100)
0.420
1.78
(0.69-4.61)
Five-minute Apgar score
1,000
1.36
(1.15-1.61)
<7 0
(
0
)
1
(
100
)
1
(
100
)
>7 13 (26.5) 36 (73.5) 49 (100)
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
926

In the first week of life, premature infants are at
risk of developing glucose homeostasis. Premature
and LBW infantsare prone to hypoglycemia because
their small reserves and immature metabolic
pathways. After birth, the transplacental glucose
supply is interrupted, while vital organs require
continuous glucose supply to meet nutritional needs.
Simultaneously glycogenic hormones (e.g. glucagon,
catecholamines, glucocorticoids) increase, partially
suppressing insulin secretion. In preterm and LBW
infants prone to hypoglycemia because of these
adaptive changes and premature metabolic pathways.
Premature infants become prone to hypoglycemia due
to the limited glycogen and fat stores, lack of ability
to generate glucose through the gluconeogenesis
pathway, have a high metabolic demand due to
relatively higher brain size, and have a poorly
developed counter-regulatory mechanisms to prevent
hypoglycemia
(Ramzan, 2017; Bromiker, 2017; Sharma, 2017). The
American Academy of Pediatrics (AAP) recommends
hypoglycemia screening in high-risk populations
including premature infants (Adamkin, 2011).
Neonatal patients with hypoglycemia are mostly
asymptomatic. Hypoglycemic neonates were
asymptomatic due to increased utilization of
alternative substrates, such as lactate, in combination
with intracerebral storage of glycogen. All neonates
with hypoglycemia should receive careful
surveillance including glucose monitoring and therapy
because of possible adverse long-term effects (Dashti,
2007; Jain, 2008).
This study showsthatthere were no significant
association between maternal age, weight, gravidity,
parity, indication of preterm labor, gender, 1-minute
and 5-minute Apgar score with hypoglycemia in
preterm infants. Neonates from diabetic mothers,
including type 1 diabetes, type 2, and gestational
diabetes, have a high risk of developing hypoglycemia
due to the relative fetal hyperinsulinism resulting in a
feedback mechanism for the balance of high glucose
levels induced by maternal diabetes (Stanescu, 2014).
There was only 1 diabetic mother in this study where
her infant had hypoglycemia. The limitation of this
study is that infant of diabetic mother was not
analyzed as a risk factor for hypoglycemia in preterm
infants because there was only 1 case of diabetic
mother in this study and breastfeeding in the delivery
room could not be anticipated even though the amount
are expected to be almost negligible (Dollberg, 2001).
5 CONCLUSIONS
Infants with birth weight <2500 grand 32-<35 week
sofgestation a lage were significantly increased risk
to had hypoglycemia.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge that the present
research is supported by Ministry of Research and
Technology and Higher Education Republic of
Indonesia. The support is under the research grant
TALENTA USU of Year 2018 Contract Number
300/UN5.2.3.1/PPM/KP-TALENTA USU/2018.
REFERENCES
Adamkin, D., 2011.ClinicalReport- Postnatalglucose
homeostasis in late-pretermand term infants.Pediatrics.
127:575-9.
Aggarwal, R., Sankar, M., Agarwal, R., Deorari, A., Paul,
V., 2010.Hypoglycemia in thenewborn.J Pediatr.
109:114-26.
Bromiker, R., Perry, A., Kasirer, Y., Einav, S., Klinger,
G.,Levy-Khademi, F., 2017. Early neonatal
hypoglycemia:incidence of and risk factors.J Matern
Fetal Neonatal Med. 26:1-7.
Dalgic, N., Ergenekon, E., Soysal, S., Koc, E., Atalay,
Y.,Gucuyener, K., 2002.Transient neonatal
hypoglycemia – long term effects on neuro
developmental out come. J Pediatr Endocrinol
Metab.15:19-24.
Dashti, N., Einollahi, N.,Abbasi, S., 2007. Neonatal
hypoglycemia: prevalence and clinical manifestations
in Tehran Children’s Hospital. Park J Med Sci.
23:340-3.
Dhananjaya, C., Kiran, B., 2011. Clinical profile of
hypoglycemia in newborn babies in a rural hospital
setting. Int J Biol Med Res. 2:1110-4.
Dollberg, S., Lahav, S.,Mimouni, F., 2001. A comparis on
of intakes of breast-fedand bottle-fed infants during
the first two daysof life. J Am Coll Nutr. 20:209-11.
Goode, R., Rettiganti, M., Li, J., Lyle, R., Whiteside-
Mansell, L., Barrett, K., Casey, P., 2016.
Developmental outcomes of preterm infants with
neonatal hypoglycemia developmental outcomes of
preterm infants with neonatal hypoglycemia.
Pediatrics. 138:e20161424.
Howson, C., Kiney, M., Lawn, J., 2012. Born to soon: the
global action report on preterm birth, WHO.
Jain, A., Aggarwal, R., Jeevasanker, M., Agarwal, R.,
Deorari, A., Paul, V., 2008.Hypoglycemia in
thenewborn.Indian J Pediatr. 75:63-7.
Lodhi, M., Shah, N., Shabir, G., 2006. Risk factors
associated with neonatal hypoglycemia. Prof Med J.
16:687-90.
Mitanchez, D., 2007. Glucoseregulation in preterm new
born infants.HormRes. 68:265-71.
Osiet, F.,Berkley, J., Ross, A., Sanderson, F., Mohammed,
S., Newton, C., 2003. Abnormal blood glucose
Maternal and Neonatal Risk Factors for Hypoglycemia in Preterm Infants
927

concentrations on admission to a rural Kenyan district
hospital: prevalence and outcome.Arch Dis
Child.88:621-5.
Ramzan, M., Razzaq, A., Kiyani, A., 2017. Hypoglycemia
in small for gestational age neonates based on
gestational age, gender, birth weight, and mode of
delivery. Pak Armed Forces Med J. 67:397-400.
Rasmussen, A.,Wehberg, S., Fenger-Groen, J., Christesen,
H., 2007.Retro spective evaluationof a National
guideline to prevent neonatal hypoglycemia. Pediatr
Neonatol. 58:398-405.
Sharma, A., Davis, A.,Shekhawat, P., 2017.
Hypoglycemia in the pretermneonate:
etiopathogenesis, diagnosis, Management, and long
term outcomes.Transl Pediatr. 6:335-48.
Singh, Y., Devi, T.,Gangte, D., Devi, T.,Singh, N.,Singh,
M., 2014.Hypoglycemia in newborn in Manipur.J
MedSoc. 28:108-11.
Sperling, M., 2012.Hypoglycemia. In Kliegman R M,
Behrman R E, Jensen H B and Stanton B F (editors).
Nelson text book of pediatrics, Elsevier Inc.
Philadelphia, 19th edition. p.517-31.
Stanescu, A., Stoicescu, S., 2014. Neonatal hypoglycemia
screening in newborns from diabetic mothers -
arguments and controversies. J Med Life. 7:51–2.
Zanardo, V., Cagda, S., Golin, R., Trevisanuto, D.,
Marzari, F., Rizzo, L., 1999. Risk factors of
hypoglycemia in premature infants. Fetal DiagnTher.
14:63-7.
ICOSTEERR 2018 - International Conference of Science, Technology, Engineering, Environmental and Ramification Researches
928
