
Uremic Pruritus Characteristics in Hemodialysis Patients with
Chronic Kidney Disease in Relation to Blood Urea Levels and Dialysis
Adequacy at Jakarta Pelabuhan Hospital, Indonesia
Maria Clarissa Wiraputranto
1
, Oktatika Pratiwi Agustinus
2
, Tamarachiara Kuntjoro
3
, Heryanto
Syamsuddin
4
1
Halimun Medical Centre Hospital, Halimun Raya St. No.9, Jakarta, Indonesia
2
Port Medical Centre Hospital, Enggano St. No.10, Jakarta, Indonesia
3
Kembangan Community Health Centre, Kembangan Raya St. No.52, Jakarta, Indonesia
4
Division of Dermatovenereology, Jakarta Pelabuhan Hospital, Kramat Jaya St., Jakarta,Indonesia
Keywords: uremic pruritus, chronic kidney disease, hemodialysis, blood urea level, dialysis adequacy
Abstract: Background and objective: Uremic pruritus is one of the distressing symptoms encountered in patients
with chronic kidney disease. It compromises overall quality of life. Factors associated with the severity of
pruritus remains unclear. This study aims to describe and analyze the relationship of blood urea level and
dialysis adequacy to uremic pruritus. Methods: We conducted a cross-sectional study for 3 months at
Jakarta Pelabuhan Hospital, Indonesia. The intensity of uremic pruritus was measured using both visual
analog scale (VAS) and numerical rating scale (NRS). Results: Of the 75 patients completed the study, 30
(40%) had pruritus. There was no significant correlation between uremic pruritus and blood urea level as
well as dialysis adequacy (p>0.05). Conclusion: Our study suggests that blood urea level and dialysis
adequacy do not play a role in pruritus in hemodialysis patients with chronic kidney disease.
1 INTRODUCTION
Uremic pruritus is one of the most frequent
complications found in hemodialysis patients with
chronic kidney disease. The itch of uremic pruritus,
whether localized or disseminated, is debilitating for
the majority of patients. This intractable symptom
could lead to affect patients’ quality of life (Ko et al.,
2013). Fifty to ninety percent of hemodialysis
patients with chronic kidney disease are afflicted with
pruritus (Aⱪca & Taşci, 2014; Al Shafei & Nour,
2016). There are multifactorial factors that could
cause uremic pruritus, in particular, blood urea levels.
Previous studies suggested that uremic pruritus is
significantly correlated with elevated levels of blood
urea (Al Shafei & Nour, 2016). On the contrary, an
effective dialysis has been shown to reduce the
severity of uremic pruritus (Ko et al., 2013).
To the best of our knowledge, there were no
studies in Indonesia reporting the prevalence of
uremic pruritus in hemodialysis patients with chronic
kidney disease as well as its correlation to blood urea
levels and dialysis adequacy. We hence sought to
describe the prevalence and clinical characteristics of
uremic pruritus in hemodialysis patients with chronic
kidney disease in Jakarta Pelabuhan Hospital,
Indonesia. Our research additionally investigates the
associations of blood urea levels and dialysis
adequacy with the severity of uremic pruritus
measured by means of visual analog scale (VAS) and
numerical rating scale (NRS).
2 METHODS
This was an analytical descriptive study of patients
with chronic kidney disease undergoing hemodialysis
treatment at Jakarta Pelabuhan Hospital
Hemodialysis Unit. We conducted a cross-sectional
research commencing from September 27th, 2017
until December 27
th
, 2017. The inclusion criteria of
our study comprised of age above 18 years, no history
of mental health problems as well as consent to
participate. The study population was obtained using
a consecutive sampling technique and was excluded
if the patient did not give written consent.
68
Wiraputranto, M., Agustinus, O., Kuntjoro, T. and Syamsuddin, H.
Uremic Pruritus Characteristics in Hemodialysis Patients with Chronic Kidney Disease in Relation to Blood Urea Levels and Dialysis Adequacy at Jakarta Pelabuhan Hospital, Indonesia.
DOI: 10.5220/0008151000680072
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 68-72
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
During this 3-month period of study, a total of 76
patients were receiving hemodialysis treatment at the
hospital hemodialysis unit. However, one patient was
excluded because of the patient’s refusal. Thus, 75
patients were included in our final analysis. Subjects
received 3.0 – 5.0 hours of hemodialysis, one to three
times a week using bicarbonate dialysate and heparin
anticoagulant. In case of allergy, we switched heparin
to enoxaparin sodium or parnaparin. The diagnosis of
uremic pruritus was made if patients met one of the
following criteria: appearance of pruritus shortly
before the dialysis treatment or at any time of dialysis
without evidence of any other active causes of
pruritus; a minimum of 3 episodes of troubling
pruritus that appears a couple times in a day and lasts
at least a few minutes during a period of time less than
2 weeks; pruritus appears less frequently than
aforementioned criteria but in a regular pattern in a
period of 6 months (Keithi-Reddy et al., 2007).
We designed a comprehensive questionnaire to
evaluate the clinical characteristics of uremic pruritus
and to assess the dialysis adequacy. In regard to the
measurement of the pruritus severity, we used two
different validated tools, VAS and NRS (Phan et al.,
2012; Reich et al., 2016; Reich et al., 2012). Patients
were asked to point to the 10-cm horizontal line of
VAS that corresponded to the intensity of pruritus
where the starting point (0 cm) indicated no pruritus
and the last point (10 cm) demonstrated the worst
imaginable pruritus. We further asked patients to tell
verbally a NRS score that best reflected their
symptom severity where 0 was no pruritus and 10
represented intolerable pruritus. The laboratory
parameter, blood urea level, was measured before the
beginning of hemodialysis treatment. We applied the
Kt/V ratio (amount of dialysis delivered: K =
clearance of urea, t = time on dialysis, V = estimated
total body water) to measure the adequacy of dialysis;
Kt/V > 1.5 was considered as an effective dialysis (1).
Statistical analysis was performed using IBM SPSS
Statistics software version 23.0 where statistical
significance was defined by a probability level of p <
0.05 (95% confidence interval). Descriptive data
were expressed as a mean ± standard deviation and
percentage. Mann-Whitney-U and t-test were
performed to compare means between pruritic and
non-pruritic patients.
3 RESULT
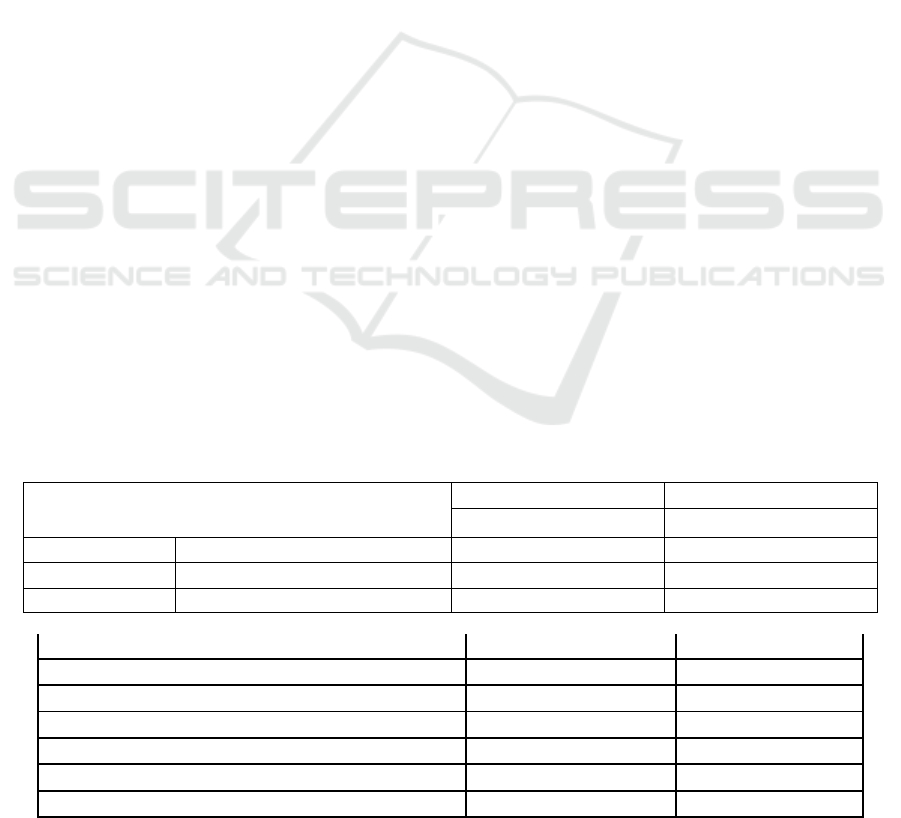
A total of 75 patients participated in this study.
Patients’ demographic and clinical characteristics, as
well as blood urea levels are summarized in Table 1.
The average age of the patients was 56 ± 12,6 years,
ranging from 33-87 years with 65% being males and
35% being females. In pruritic patients, there were 18
male patients (60%) and 12 female patients (40%).
Table 2 demonstrated the prevalence and uremic
pruritus characteristics. The most frequent pruritus
distributions were the localized areas (77%) consisted
of the back (32%), the head (17%), followed by other
areas including the chest, palm, arm, crotch, waist,
thigh, sole, back of hand, shoulder, stomach, and
elbow. There was no statistically significant
difference in the blood urea levels between pruritic
patients (n = 30, Md = 115.00) and non-pruritic
patients (n = 45, Md = 111.00) according to the
Mann-Whitney-U test (p = 0.669) . Applying the non-
dependent t-test, we found that the means of dialysis
adequacy in 30 patients with uremic pruritus and 45
patients without pruritus were not statistically
significantly different (p = 0.192).
Table 1. Demographic, clinical characteristics, and blood urea levels of the participants
Variables
Pruritic patients Non-pruritic
(n=30) patients (n=45)
Gender Male 18 (60%) 31 (69%)
Female 12 (40%) 14 (31%)
Age (years) 54 ± 13.0 57 ± 12.3
Etiology of chronic kidney disease
Hypertension (HTN) 11 (37%) 19 (42%)
Diabetes mellitus (DM) 5 (17%) 11 (24%)
Kidney stone - 3 (7%)
Polycystic kidney disease 1(3%) 1 (2%)
Idiopathic 3 (10%) 2 (5%)
Others 1 (3%) -
Uremic Pruritus Characteristics in Hemodialysis Patients with Chronic Kidney Disease in Relation to Blood Urea Levels and Dialysis
Adequacy at Jakarta Pelabuhan Hospital, Indonesia
69

Combined DM with HTN 8 (27%) 7 (16%)
HTN with others 1 (3%) 1 (2%)
HTN with kidney stone - 1 (2%)
Polycystic kidney disease
- -
with others
Duration of
hemodialysis ≤ 3 months 7 (23%) 22 (49%)
>3 months 23 (77%) 23 (51%)
Dialysis adequacy
(Kt/V) 2.3 ± 0.9 2.0 ± 1.1
Dialyzer
membrane Polysulfone 21 (70%) 22 (49%)
Polyarylethersulfone 9 (30%) 23 (51%)
Hemodialysis
acces Continuous 21 (70%) 21 (47%)
Temporary 9 (30%) 24 (53%)
Blood urea levels
112.8 ± 34.5 125.5 ± 58.6
Abbreviation: n: Number of patients, K: clerarance of urea; t: time on dialysis; V; estimated total water
Table 2. Uremic pruritus characteristic in patients with pruritus
Variables Statistics
Uremic pruritus diagnosis
criteria
Apperance of pruritus shortly before the dialysis treatment
or at any time of dialysis without evidence of any other
active causes of pruritus
11 (37%)
A minimum of 3 episodes of troubling pruritus that appears
a couple times in a day and lasts at least a few minutes during
a period of time less than 2 weeks
15 (50%)
Pruritus appears less frequently than aforementioned
criteria but in a regular pattern in a period of 6 months
4 (13%)
Distribution
Generalized
7 (23%)
Localized
23 (77%)
Numerical Rating Scale (NRS) 4,5 ± 2.3
Visual Analog Scale (VAS) 4 ± 2.1
Abbreviation: n: Number of patients
4 DISCUSSION
Uremic pruritus remains a frequent and intractable
symptom encountered in hemodialysis patients with
chronic kidney disease (Ko et al., 2013; Kilic &
Tasci, 2014, Shirazian et al., 2017). There is
inconclusive evidence in terms of the
pathophysiology of this entity. In our study, we found
that there were 40% patients with chronic kidney
disease experiencing uremic pruritus. From this 30
pruritic patients, 18 were males and 12 were females.
From this 30 pruritic patients, 18 were males and 12
were females. The majority of patients who reported
pruritus were those who had already undergone
hemodialysis treatment for more than 3 months
(77%).
Fifteen percent of pruritic patients met the second
diagnosis criteria of uremic pruritus which was a
minimum of 3 episodes of troubling pruritus that
appears a couple times in a day and lasts at least a few
minutes during a period of time less than 2 weeks.
Unlike our study, most of previous studies did not
analyze the prevalence of uremic pruritus specifically
based on the diagnosis criteria of uremic pruritus
according to its time of onset and episode frequency.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
70

Narita et al reported that blood urea level was
statistically correlated with pruritus severity.
According to Ko et al’s study, dialysis adequacy 1.5
had a significant effect in decreasing the severity of
pruritus. On the other hand, we found a difference in
blood urea levels between pruritic and non-pruritic
groups but it was not statistically significant p > 0.05
(0.669). Our study also showed that there was no
statistical difference regarding dialysis adequacy
(Kt/V) between the two groups (p > 0.05). These
findings could be affected by the small number of
participants in our study.
There were 23 pruritic patients (50%) from a total
of 46 patients who had received hemodialysis
treatment for > 3 months. For 29 other patients who
had undergone hemodialysis for ≤ 3 months, 7 of
them (24%) had pruritus. Until now, the relationship
of dialysis vintage with uremic pruritus was
controversial. Some studies suggested that 3-month
hemodialysis therapy would result in decreased
intensity of pruritus while others reported that a
minimum of 12-month hemodialysis would show
beneficial effect. The most common used pruritus
assessment tools are VAS and NRS attributed to its
high discriminative sensitivity. According to the
study from Reich et al, evaluation with NRS would
result in higher pruritus intensity compared with
VAS. There was only a slight difference of 0.1 – 0.6
points between VAS and NRS assessment but this
was not statistically significant (Reich et al., 2012;
Reich et al., 2016). In our study, the pruritus intensity
in the 30 patients with pruritus was 4 ± 2.1 and 4.5 ±
2.3 for VAS and NRS scores, respectively. With
regard to the distribution of the pruritus, we found
that 77% of the patients had localized pruritic areas
on the back, head, chest and extremities. Our findings
were consistent with data regarding the high variety
of the uremic pruritus distribution with the most
commonly involved areas were back, stomach, hand
and head.
5 CONCLUSION
Taken together, our study demonstrates that there is
no statistically significant correlation between uremic
pruritus and blood urea level or dialysis adequacy.
However, there are some limitations of this study.
First, a small number of participants were involved.
Second, the data on VAS and NRS did not include the
baseline scores before the hemodialysis treatment
started. Therefore, we could not further analyze the
relationship of dialysis adequacy and reduction of
pruritus. Third, our study did not exclude participants
with confounding factors, for instance diabetic and
hepatitis patients. Further research with bigger
sample size and prospective design is necessary to
understand contributing factors in uremic pruritus
development.
ACKNOWLEDGMENT
We would like to express our sincere gratitude to all
the patients who signed the consent forms and
participated in the study. Our thanks are also extended
to Mrs. Dessy Emastari as the Director, M. Syaiful
Huda E., MD as the Chief, and all the staffs of
hemodialysis unit at Jakarta Pelabuhan Hospital for
their continuous help and support
.
REFERENCES
Aⱪca, N.K., & Taşci, S., 2014. An important problem
among hemodialysis patients: uremic pruritus and
affecting factors. Turkish Nephrology Dialysis
Transplantation, 23(3), pp. 210 – 216.
Al Shafei, N. K., & Nour, A., 2016. Observations on the
Association of Serum histamine, Interleukins and Other
Serum Biochemical Values with Severity of Pruritus in
Chronic Hemodialysis Patients. Journal Nanomedicine
Nanotechnology, 7(1).
Keithi-Reddy, S.R., Patel, T.V., Armstrong, A.W., Sigh,
A.K., 2007. Uremic pruritus. Kidney international, 72,
pp. 373-377.
Kilic, A.N, & Tasci, S., 2014. An Important Problem
Among Hemodialysis Patients: Uremic Pruritus.
Turkish Nephrology Dialysis Transplantation, 23(3),
210-216.
Ko, M. J., Wu, H. Y., Chen, H. Y., Chiu, Y. L., Hsu, S. P.,
Pai, M. F., Ju, Y.Y., Lai, C.F., Lu, H.M., Huang, S.H.,
Yang S.Y., Wen, S. Y., Chiu, H.C., and Jee, S.H., 2013.
Uremic pruritus, dialysis adequacy, and metabolic
profiles in hemodialysis patients: a prospective 5-year
cohort study. PLoS One, 8(8), pp. 71404.
Phan, N. Q., Blome, C., Fritz, F., Gerss, J., Reich, A., Ebata,
T., Augustin, M., Szepietowski, J.C., & Ständer, S.,
2012. Assessment of pruritus intensity: prospective
study on validity and reliability of the visual analogue
scale, numerical rating scale and verbal rating scale in
471 patients with chronic pruritus. Acta dermato-
venereologica, 92(5), pp. 502-507.
Reich, A., Heisig, M., Phan, N. Q., Taneda, K., Takamori,
K., Takeuchi, S., Furue, M., Blome, C., Augustin, M.,
Stander, S., & Szepietowski, J. C., 2012. Visual
analogue scale: evaluation of the instrument for the
assessment of pruritus. Acta dermato-
venereologica, 92(5), pp. 497-501.
Uremic Pruritus Characteristics in Hemodialysis Patients with Chronic Kidney Disease in Relation to Blood Urea Levels and Dialysis
Adequacy at Jakarta Pelabuhan Hospital, Indonesia
71

Reich, A., Riepe, C., Anastasiadou, Z., Mędrek, K.,
Augustin, M., Szepietowski, J. C., & Ständer, S., 2016.
Itch assessment with visual analogue scale and
numerical rating scale: determination of minimal
clinically important difference in chronic itch. Acta
dermato-venereologica, 96(7), pp.978-980.
Reich, A., Riepe, C., Anastasiadou, Z., Mędrek, K.,
Augustin, M., Szepietowski, J. C., & Ständer, S., 2016.
Itch assessment with visual analogue scale and
numerical rating scale: determination of minimal
clinically important difference in chronic itch. Acta
dermato-venereologica, 96(7), pp. 978-980.
Shirazian, S., Aina, O., Park, Y., Chowdhury, N., Leger, K.,
Hou, L., Miyawaki, N., & Mathur, V.S., 2017. Chronic
kidney disease-associated pruritus: impact on quality of
life and current management challenges. International
Journal of Nephrology and Renovascular Disease, 10,
pp. 11-26.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
72
