
Differences of Minimum Erythema Dose (MED) in Fitzpatrick IV
Skin Type Adults and Elderly with an Exposure of Narrowband
Ultraviolet B (NB-UVB)
Arini Astasari Widodo
1
, Tjut Nurul Alam Jacoeb
1
, Aria Kekalih
2
, Endi Novianto
1
1
Dermato-venereology Department, Faculty of Medicine, Universitas Indonesia/Dr. Cipto Mangukusumo National General
Hospital, Jakarta
2
Community Medicine Department, Faculty of Medicine, Universitas Indonesia
Keywords: Minimal Erythema Dose, Fitzpatrick Skin Type IV, Narrowband Ultraviolet B, elderly
Abstract: The skin of the elderly is different compared to that of an adult due to aging, where such changes could
influence the skin's response to ultraviolet exposure, including erythemal response. This difference could lead
to MED change, which in turn affects the effectiveness of treatment modalities for skin diseases. This study
aims to determine the difference between average MED in the elderly and adults with Fitzpatrick IV skin
type, as well as the difference between 24 hours-MED and 48 hours-MED. MED calculations were based on
skin erythemal responses relative to six different exposure doses of NB-UVB in elderly people aged over 60
years and adults aged 18-45 years. The irradiation is done with a Waldmann UV109 lamp with dosages
starting from 300, 500, 700, 900, 1100, and 1300 mJ/cm
2
. Responses were examined at 24 hours and 48 hours
post-irradiation by three different assessors. In the adult group, the mean of 24 hours-MED was 554 ± 182
mJ/cm
2
and 48 hours-MED was increased to 606 ± 167 mJ/cm
2
. In the elderly group, the mean of 24 hours-
MED was 702 ± 340 mJ/cm
2
and 48 hours-MED was increased to 836 ± 341 mJ/cm
2
. The 24 hours-MED in
the elderly group is higher compared to that of the adult group; however, the difference is not statistically
significant (p=0.158). There is a statistically significant difference between 24 hours-MED and 48 hours-
MED was found (<0.001) in the elderly group. The mean of 24 hours-MED in elderly and adults in this study
could be applied clinically.
1 INTRODUCTION
Elderly is defined as a person who has reached the age
of 60 (sixty) years old or above, while adult age is
defined as 18-45 years old and 45-59 years old is
defined as pre-geriatrics age (Peraturan Menteri
Kesehatan Republik Indonesia, 2016). According to a
report detailing visits to the Geriatric Division of
Dermatovenereology Department of Dr. Cipto
Mangunkusumo General Hospital, psoriasis vulgaris
and atopic dermatitis are included in the top 10
diagnoses (Legiawati et al., 2016), and these diseases
frequently require phototherapy modalities, including
phototherapy using NB-UVB.
The assessment of initial dose for phototherapy
may be approximated based on skin types or on MED
irradiation test (Taylor and Stern, 1991). MED refers
to a radiation dose used to produce just perceptible
erythema (JPE) or the minimum energy required to
produce a pink erythema response with clearly-
defined border (Cafardi et al., 2012; Morrison W,
2005).
The skin of the elderly is different compared to
that of an adult due to aging. These changes may
affect the skin’s response to ultraviolet light exposure
(Gilchrest et al, 1982), and may include changes in
inflammatory response and its mediators, changes in
the immune system (immunosenescense), changes in
the morphology of keratinocytes, and changes in the
size of blood vessels. These may lead to a reduced
erythema response triggered by UV exposure
(Raschke and Elsner, 2010). Changes in erythema
response due to aging is expected to affect MED in
the elderly group.
Studies on MEDs in the elderly yield varying
results. This may be due to difference of light source
and measurement in differing phases, resulting in the
difficulties to conclude the erythematous effect of
NB-UVB exposure in the elderly (Thomas and
Bergoend, 1977).
Studies on MED in the elderly with
Widodo, A., Jacoeb, T., Kekalih, A. and Novianto, E.
Differences of Minimum Erythema Dose (MED) in Fitzpatrick IV Skin Type Adults and Elderly with an Exposure of Narrowband Ultraviolet B (NB-UVB).
DOI: 10.5220/0008151100730077
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 73-77
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
73

the most frequent skin types in Indonesian population
has never been conducted and it is deemed necessary
to study the MED with the exposure of NB-UVB in
the elderly, compared to adult population with the
same skin type (Fitzpatrick IV and V being the most
frequent in Indonesians) (Bernadette et al., 2002).
This study aims to determine the difference of
MED in adults and elderly with Fitzpatrick IV skin
type, to determine the average MED for Fitzpatrick
IV skin type for both adults and elderly, and to
determine the difference of 24 hours- and 48-hour-
MEDs in the elderly.
2 METHODS
This study is a clinical trial that compares the MED
of adults and the elderly. The subject of the study are
geriatric residents of Tresna Werdha Nursing Home
(Cilandak, South Jakarta, Indonesia) with Fitzpatrick
IV skin type who consented to participate in the
study, as well as Nursing Home workers aging 18-45
years old with no history of diseases affected by UV
lights or causing photosensitivity. Thirty-eight
subjects from the adult group and 36 subjects from
the elderly group was exposed with narrowband
ultraviolet light on their backs using Waldmann
UV109 lamp on the opened window with dosages
starting from 300, 500, 700, 900, 1100, and 1300
mJ/cm
2
. This study has been approved by the Health
Research Ethical Committee of the Faculty of
Medicine, Universitas Indonesia.
Responses were examined at 24 hours and 48
hours post-irradiation by 3 individuals, namely the
principal investigators and 2 dermatovenereologist
with ICC approaching 1.00 (0.98).
Data analyses were conducted in two phases, i.e.
descriptive phase and inferential phase. The
descriptive phase was performed to compare MED of
adults and elderly population using Mann-Whitney
due to abnormal distribution. A Wilcoxon test was
conducted to compare the 24 hours- and 48 hours-
MED in both adults and elderly. All analyses were
performed using SPSS program version 20.
3 RESULTS
Of 36 elderly subjects, 17 (47.2%) were male, and 19
(52.9%) were female. In the adult group, 14 (42.4%)
were male, and 19 (57.6%) were female. There is no
significant difference in the number of male between
the adult and elderly groups. Although the percentage
of female is higher in both groups, this is not
significant; thus, both groups can be considered
homogenous in terms of gender. Based on the data
from 69 subjects included in the analysis, other than
gender, there are no significant difference in terms of
ethnicity and level of dependency.
In the adult population, the median of 24 hours-
and 48 hours-MED are 500 mJ/cm
2
(300 – 900
mJ/cm
2
) and 700 mJ/cm
2
(300 – 900 mJ/cm
2
),
respectively; while the mean 24 hours-MED and 48-
hours MED are 554 ± 182 mJ/cm
2
and 606 ± 167
mJ/cm
2
, respectively. The 24 hours-MED in the
elderly group is higher compared to that of the adult
group; however, the difference is not statistically
significant (p=0.158). Table 1 presents the
comparison of 24 hours- and 48 hours-MED in the
adult and elderly groups. Figure 1 presents the
distribution of 24 hours- and 48 hours-MED in both
adults and elderly.
In terms of the 24 hours-MED, we failed to reject
null hypothesis despite the fact that our sample size
indicates adequate power.
Table 1. Comparison of 24 hours- and 48 hours-MED in the adult and elderly groups
Variable Adult Elderly p
24 hours-MED
(mJ/cm
2
)
Median (min – max)
Mean
500 (300-900)
554 182
550 (300-1300)
702 340
0.158
48 hours-MED
(mJ/cm
2
)
Median (min – max)
Mean
700 (300-900)
606 167
700 (400-1300)
836 341
0.026
*Due to the abnormal distribution of MED data in this study, a non-parametric test, i.e. Mann-Whitney Test was
used in data analysis.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
74
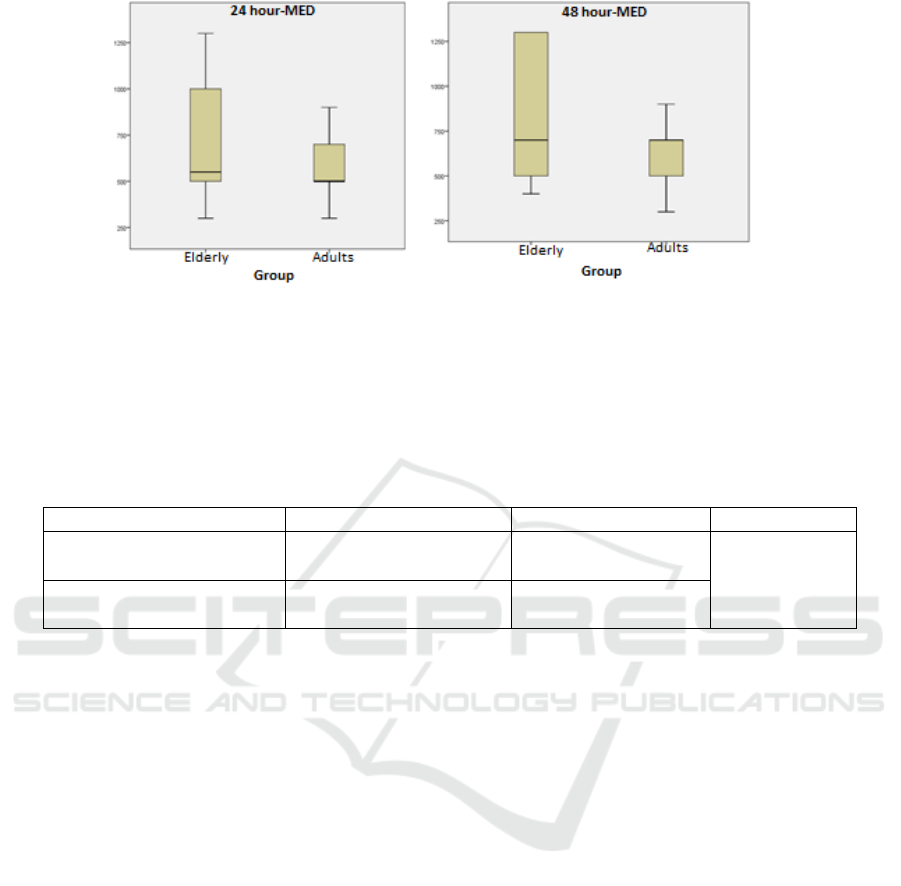
Figure 1. Distribution of 24 hours- and 48 hours-MED in the adult and elderly groups
In the elderly group, the median of 24 hours-MED
and 48 hours-MED are 550 (300 – 1300) mJ/cm
2
and
700 (400 – 1300) mJ/cm
2
, respectively; while the
mean 24 hours-MED and 48 hours-MED are 702
340 mJ/cm
2
and 836 341 mJ/cm
2
, respectively.
Based on the Wilcoxon test, there is a statistically
significant difference between 24 hours- and 48
hours-MED in the elderly group (p <0.001). Table 2
presents the comparison of median 24 hours- and 48
hours-MED in the elderly group.
Table 2. Comparison of median 24 hours- and 48 hours-MED in the elderly groups
Variable Elderly p
24 hours-MED (mJ/cm
2
)
Median (min-max)
Mean
550 (300-1300)
702 340
<0.001
48 hours-MED (mJ/cm
2
)
Median (min-max)
Mean
700 (400-1300)
836 341
* Due to the abnormal distribution of MED data in this study, Wilcoxon Test was used in data analysis
4 DISCUSSION
This study found a higher percentage of female
compared to male in both groups. However, the
difference is not significant; thus, both groups can be
considered homogenous in terms of gender. This is
likely due to the fact that there is more female elderly
compared to male in the location where the study was
conducted. This is also consistent with the female to
male elderly ratio in Indonesia, which is 9:8, and with
the higher life expectancy for female elderly
compared to male elderly (Pusat Data dan Informasi
Kementerian Kesehatan Republik Indonesia, 2016).
This study found a difference in 24 hours-MED
between adult and elderly groups. However, this
difference is not statistically significant (p=0.158).
Some literatures have found that the erythema
response in the elderly differs from that of adult
population (Gilchrest at al., 1982; Gloor and
Scherotzke, 2002; Guerrera, 1989).
This is due to various factors, including
differences in anatomical and physiological aspects,
vascular response, immune response, and so on.
Previous studies also found varying results. Cox
found that in the 24 hours after irradiation, no
statistically significant difference was observed in the
mean MED of adult group compared to elderly.
However, this study used different UVB source,
leading to difficulties in comparing the dosages
received by subjects. The study also included subjects
with Fitzpatrick I-V skin types (Cox et al., 1989).
Amblard performed an analysis of 2 quantitative
variable, namely age and MED, and found a good
correlation (r=0.78, P<0.001) in 303 patients aged 5-
89 years old. The study found that the MED lowers
with the increase of age. However, the study was
conducted on patients with lighter skin, which may
confound the result. Differ to the current study,
Amblard exposed their subjects to UVB using
different light source and measure the erythema
response using different methods as well. These
differences may contribute to the different results
yielded by that study and the current study (Amblard
et al., 1982).
Gloor conducted a study on 20 subjects aged 20-
40 years old and 20 subjects aged 70 and above with
Fitzpatrick I – IV skin types, where the MED was
Differences of Minimum Erythema Dose (MED) in Fitzpatrick IV Skin Type Adults and Elderly with an Exposure of Narrowband
Ultraviolet B (NB-UVB)
75

measured 48 hours after irradiation using narrowband
UVB. The study found no statistically significant
difference in 48 hours-MED between both groups
(Gloor and Scherotzke, 2002). All differences in
erythema response in the elderly descibed above
explains the finding of higher MED in the elderly
group compared to the adult group. However,
considering that the difference of 24 hour-MED is not
statistically significant, one can interpret that in
practice, the initial dose of phototherapy does not
need to be different between adults and the elderly.
Despite previous literatures showing various
evidences that the biological and physiological
erythema response are different in adults and in the
elderly, this alone does not affect the MED for NB-
UVB which may be useful to determine the initial
dose of phototherapy.
This study is also the first to compare the MED
between adults and elderly population in Indonesia,
where the majority of skin type is Fitzpatrick IV.
Even with the same skin type, considering the wide
range of minimum and maximum value as presented
in Table 2, determining initial dose for phototherapy
based on skin type might not always lead to a uniform
result; therefore, it is more recommended to use MED
as a reference for initial dose for phototherapy.
When a comparison is made between 24 hours-
and 48 hours-MED in the elderly, we found a
statistically significant difference with a p value of
<0.001). This indicates that significant erythematous
changes occur over time in the elderly. From this
finding, it can be interpreted that exposure to NB-
UVB with a mean radiation dose of 836 341 mJ/cm
2
will result in an erythema with a higher intensity than
MED definition at 24 hours, and result in clinical
features of erythema consistent with the definition of
MED at 48 hours.
In clinical application, the lowest dose to produce
a pink erythema response with clearly-defined border
should be used in determining MED. Based on the
findings of the current study, the lowest dose for
MED is obtained at 24 hours; therefore, 24 hours-
MED should be used in determining the initial dose
for phototherapy.
This study is the first study that compares 24
hours- and 48-hour MED in the elderly. Gloor were
the first to observe the 48 hours-MED in the elderly.
This observation was conducted in the 48th hour
following irradiation due to a theory stating that
erythema response in the elderly is expected to be
delayed, as confirmed in the findings of a previous
study (Gloor and Scherotzke, 2002; Guerrera, 1989).
Gloor’s study did not compare the 24 hours- and 48-
hour MED; however, despite finding that there are no
significant difference in terms of 48-hour MED
between adults and elderly populations, they found a
higher erythema intensity in the elderly population at
48 hours after irradiation.
Considering that this study is performed on
subjects with Fitzpatrick IV skin type, it is also
important to remember that the photoprotection effect
of melanin might also be a contributing factor to the
differences between the current study and previous
studies conducted on subjects with lighter skin. It
remains possible that the findings of this study are due
to the photoprotection effect of melanin, which is a
stronger determinant factor compared to age. In
darker skin, erythema resulting from UVB exposure
will subside after 1-3 days, while in individuals with
lighter skin, the response may persist for 1-2 weeks
(Weichenthal and Schwarz T., 2005).
5 CONCLUSION
The mean 24 hours-MED in the adult group with
Fitzpatrick IV skin type is 554 ± 182 mJ/cm
2
and the
mean 24 hours-MED in the elderly group with
Fitzpatrick IV skin type is 702 340 mJ/cm
2
. The 24
hours-MED of the elderly group is higher compared
to that of the adult group; however, this difference is
not statistically significant. There is significant
difference between 24 hours-MED and 48 hours-
MED in the elderly group with Fitzpatrick IV skin
type. The mean of 24 hours-MED in elderly and
adults in this study could be applied clinically.
REFERENCES
Amblard, P., Beani, J., Gautron, R., Reymond, J.,
Doyon, B., 1982. Statistical study of individual
variations in sunburn sensitivity in 303 volunteers
without photodermatosis. Archives of
Dermatological Research 274, 195–206.
doi:10.1007/BF00403722
Bernadette I, Daili S, Soedharmono S., 2002. Dosis
eritema minimal (DEM) regio infraskapula dan
regio gluteal dengan penyinaran Narrowband
UVB pada individu normal tipe kulit IV dan V.
Media Dermato-venereologica Indones.
Cafardi J, Pollack B, Elmets C. Phototherapy. In:
Goldsmith L, Katz S, Gilchrest B, Paller A,
Leffell D, Wolff K, editors., 2012. Fitzpatricks
Dermatology in General Medicine. McGraw Hill
Companies., 8th Editio., pp. 2841–50.
Cox, N.H., Farr, P.M., Diffey, B.L., 1989. A
Comparison of the Dose-Response Relationship
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
76

for Psoralen-UVA Erythema and UVB Erythema.
Archives of Dermatology 125, 1653–1657.
doi:10.1001/archderm.1989.01670240053012
Gilchrest, B.A., Stoff, J.S., Soter, N.A., 1982.
Chronologic aging alters the response to
ultraviolet-induced inflammation in human skin.
Journal of Investigative Dermatology 79, 11–15.
doi:10.1111/1523-1747.ep12510417
Gloor, M., Scherotzke, A., 2002. Age dependence of
ultraviolet light-induced erythema following
narrow-band UVB exposure. Photodermatology
Photoimmunology and Photomedicine 18, 121–
126. doi:10.1034/j.1600-0781.2002.00756.x
Guerrera M., 1989. Age and skin response to
ultraviolet radiation. J Cutan Aging Cosmet
Dermatol 1, pp. 135–44.
Legiawati L, Yusharyahya S, Sularsito S, Margaretha
S., 2016. The incidence of dermatologic disease at
dermatology clinic, department of
dermatovenereology university of indonesia,
ciptomangunkusumo hospital in 2008-2013. In:
22nd Regional Confrence of Dermatology (Asian-
Australasian). Raffles City Convention Centre,
Singapore.
Morrison W, 2005. Phototherapy and
photochemotherapy of skin disease. Boca Raton:
Taylor and Francis Group.
Peraturan Menteri Kesehatan Republik Indonesia,
2016. Rencana Aksi Nasional Lanjut Usia Tahun
2016-2019, 25.
Pusat Data dan Informasi Kementerian Kesehatan
Republik Indonesia. Situasi Lanjut Usia (Lansia)
di Indonesia., 2016. Jakarta: Kementerian
Kesehatan Republik Indonesia.
Raschke C, Elsner P. Skin aging: A brief summary of
characteristic changes. In: Farage M, Miller K,
Maibach H, editors., 2010. Textbook of Aging
Skin. Verlag Berlin Heidelberg: Springer., pp. 37–
47.
Taylor, C.R., Stern, R.S., 1991. Magnitude and
Duration of UV-B—Induced Tolerance. Archives
of Dermatology 127, 673–677.
doi:10.1001/archderm.1991.01680040081007
Thomas P, Bergoend H., 1977. Principles and
techniquess de l’exploration photobiologique.
Ann Dermatol Venereol 104., pp. 513–24.
Weichenthal M, Schwarz T., 2005. Phototherapy:
how does UV work?. Photodermatol
Photoimmunol Photomed 21, pp. 260–6.
Differences of Minimum Erythema Dose (MED) in Fitzpatrick IV Skin Type Adults and Elderly with an Exposure of Narrowband
Ultraviolet B (NB-UVB)
77
