
Study of Psychoneuroimmunology in Atopic Dermatitis
Cita Rosita Sigit Prakoeswa
1*
, Bayu Bijaksana Rumondor
2
, Menul Ayu Umborowati
1
, Sylvia
Anggraeni
1
, Anang Endaryanto
3
1
Allergy Immunology Division, Dermatology Venereology Department, Faculty of Medicine, Universitas Airlangga - Dr.
Soetomo General Hospital, Surabaya, Indonesia.
2
Medical Student, Faculty of Medicine, Universitas Airlangga - Dr. Soetomo General Hospital, Surabaya, Indonesia.
3
Allergy Immunology Division, Child Health Department, Faculty of Medicine, Universitas Airlangga - Dr. Soetomo
General Hospital, Surabaya, Indonesia.
Keywords: psychoneuroimmunology, atopic dermatitis, stress, hypothalamus-pituitary-adrenal.
Abstract: Psychoneuroimmunology is an inter disciplinary field that specifically examines the biochemical cross talk
between brain, behavior and the immune system and between allergy immunology concept and
psychosocial factors. The increase of allergic manifestation may be associated with environmental factors
such as stress. A growing number of studies have suggested an altered hypothalamus-pituitary- adrenal
(HPA) axis function to stress in allergy. It is speculated that a dysfunctional HPA axis in response to stress
may facilitate and/or consolidate immunological aberrations and thus, may increase the risk for allergic
sensitization and exacerbation especially under stressful conditions. It has been established via clinical and
physiological means that psychological stress is a significant contributor to allergy course through its direct
and indirect effects on immune response, cutaneous neuropeptide expression, and skin barrier function.
1 INTRODUCTION
Psychoneuroimmunology is an interdisciplinary
field of study which focuses in the biochemical
interactions between the brain, social behavior and
the immune system (Suarez et al., 2012), especially
the correlation between immunologic disorders and
psychosocial factors (Chida et al., 2008; Nordlind,
2008). Hypersensitivity reactions are identified by
overabundant production of immunoglobulin E
(IgE), one of which is atopic dermatitis (AD)
(Buske-Kirschbaum, 2009).
Allergen presentation by dendritic cells initiates
the late phase response via activation of T-helper
(Th) cells which in turn secretes large amounts of
interleukin (IL)-4, IL-5 and IL-13. This reflects a
Th-2 dominant response which plays a big role in
allergic inflammations. IL-4 and IL-13 stimulates
the synthesis of IgE and also induces B cells to
switch from other Ig isotypes into IgE. This is
followed with an increase of Vascular Cells
Adhesion Molecule 1 (VCAM-1) expressions, and
the recruitment and invasion of eosinophils to
inflamed sites. IL-5 induces eosinophils to secrete
Eosinophyl Cationic Protein (ECO) which
contributes to the degradation of cells. The role of
immunologic dysfunction in the pathomechanism of
allergic diseases including AD has been proven in
several previous studies, however most of them
remained not well understood (Buske-Kirschbaum,
2009; Dave et al., 2011).
One popular hypothesis which potentially
explains the increased prevalence of AD is that its
immunopathology is affected by several factors i.e.:
lifestyle, nutritional status and intake, pollution and
also psychosocial stress.
This study aimed to discuss the role
psychoneuroimmunlogy in the pathogenesis of
allergy, including the potential impact of hyper or
hypo responsiveness of hypothalamus-pituitary-
adrenal (HPA) axis towards the onset and chronicity
of allergic diseases in dermatology, in this case,
atopic dermatitis. Other factors which contributes to
the dysfunction of HPA axis in allergy, including
stress management therapy which targets neuro-
immune systems for comprehensive allergic
management is also discussed in this study.
Prakoeswa, C., Rumondor, B., Umborowati, M., Anggraeni, S. and Endaryanto, A.
Study of Psychoneuroimmunology in Atopic Dermatitis.
DOI: 10.5220/0008160304850488
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 485-488
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
485
2 CASE
A 11-year-old female came to the dermatology and
venerology outpatient clinic in Dr. Soetomo teaching
hospital with clinically severe eczema along with
allergic history towards house dust mites, animal fur
and certain food. Laboratory results show a total IgE
value of 937 (Normal value: <100), with specific
IgE positivity towards eggs, poultry, shrimp, crabs,
house dust mites, and bird feather as well as cat and
dog fur. After a series of thorough anamnesis and
examinations, this patient was diagnosed with severe
atopic eczema, allergic rhinitis and chronic
intermittent cough. Comprehensive patient
management was done including skin care and
topical as well as oral corticosteroid for eczema,
symptomatic medication for allergic rhinitis, and
immunotherapy.
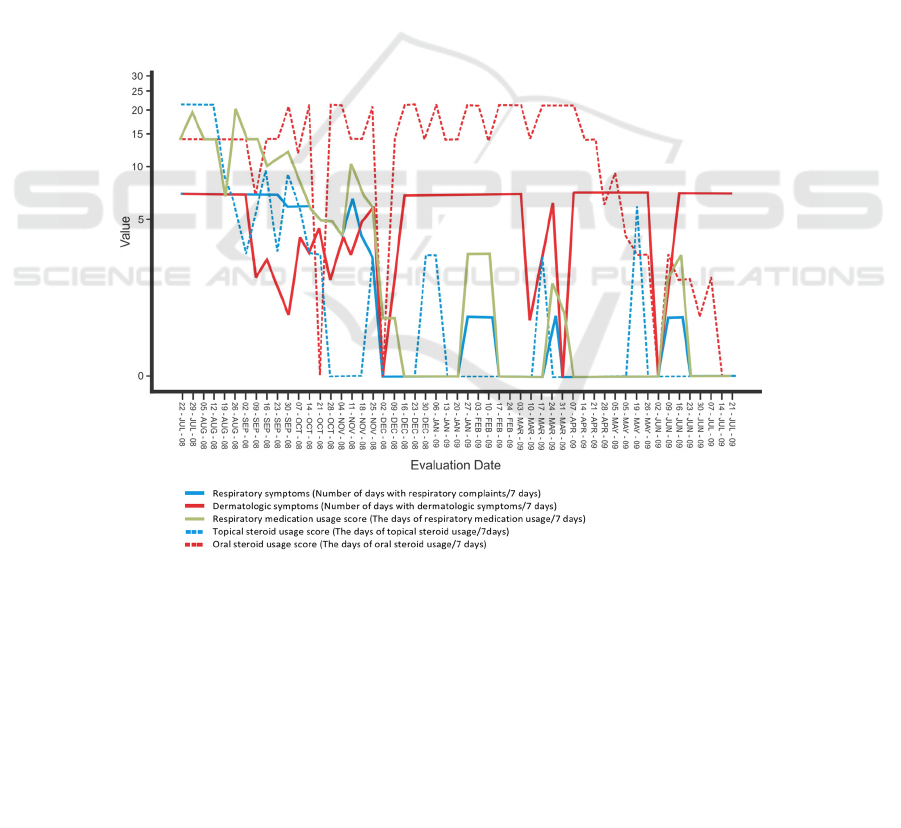
Patient went through these regiment for a year.
For the first few months, food elimination program
almost always fails where the patient fails to avoid
food which causes allergic reactions. The impact
could be directly seen along with worsening of
eczema. Clinical improvement of eczema eventually
was seen after 9 months of treatment due to the
patient's gradually increased compliance towards the
food elimination program.
Patient went through a series of immunotherapy
every week for the first 14 appointments, followed
by every 3 weeks for the next. Respiratory tract
conditions including sneezing, nose itching, show
clinical improvement after the 10th administration.
Another positive impact was that oral corticosteroid
was needed less frequently after 4th immunotherapy.
This researcher found an interesting fact that all the
clinical improvements regarding eczema and
respiratory tract complaints are somehow related to
the patients father's presence.
Figure 1: Graph demonstrating evaluated aspects of this patient's disease progression throughout the year,
illustrated by different lines. (Endaryanto, 2015).
3 DISCUSSION
In the earlier decades of life, atopy is characterised
by hyperresponsiveness of HPA axis to stress
(Buske-Kirschbaum, 2009; Ball et al., 2006). The
dysfunction of HPA axis mechanism in newborns
which eventually leads to allergy is yet well
understood. However, some studies have shown that
it is influenced by genetic factors and the prosess of
fetal programming. (De Weerth et al., 2005; Wüst et
al., 2006). During stress psychological, the increase
of endogenous cortisol which triggers dominant
response from th2 will further increase the risk of
allergic sensitisation and (accelerate) the onset of
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
486

allergies. Cortisole stimulates IL-4 which will later
induce the production of IgE and B-cells. (Barnes,
2001). During the course of time, hyperresponsive
HPA axis will switch to hyporesponsiveness. The
factors which causes this phenomenon is not fully
understood, but it is thought to be affected by
chronic inflammation which induces continuous
secretion of proinflammatory cytokines or by
(chronic/prolonged) stress due to the allergy itself or
due to social problems. In chronic allergy in
children, lack of cortisol adequate secretion response
in stressful conditions causes lack of inflammatory
response control such as the regulation of pro-
inflammatory cytokines, the adhesion of leucocytes
and the activation of eosinophils. Hence, in
children, stress also can be a risk factor of
exacerbation and chronic progression of allergies
due to its impact which causes HPA axis
dysfunction.
The central nervous system response to
phychologic stress (Suarez et al., 2012). The HPA
axis responses to phsychologic stress by increasing
the secretion of corticotropin releasing hormone
(CRH) and adrenocorticotropic hormone (ACTH)
(Glaser, 2005). which then triggers the secretion of
pituitary prolactin (PRL) which inhibits lymphocyte
proliferation induced by stress (Foitzik et al., 2009).
CRH and ATCH also stimulates norepinephrine
(NE) and the release of cortisol from adrenal cortex
which in turn stimulates and regulates other immune
responses while sending a negative feedback to the
hypothalamus and hypophysis. This is followed by
an increased release of serotonin (5HT) in the brain
stem as well as P-Substance (SP), gastrin-releasing
peptide (GRP) and calcitonin gene related peptide
(CGRP) in the dorsal ganglia (Norlind et al., 2008;
Roosterman et al., 2006; Slominski et al., 2005).
In the dermis, immune cells release cytokines,
chemokines and neuropeptides which modulates the
inflammatory responses, triggers the sensation of
pain and itchiness and also transmits sensory stimuli
through dorsal ganglia and spinal tract to spesific
areas in the central nervous system. Cutaneous mast
cells are known to be well related to SP, CGRP,
pituitary adenylate cyclase activating protein
(PACAP) and opioid releasing neurons; and is
responsive towards said neuromediators. As a
response to stress, cutaneous mast cells stimulate
several inflammatory mediators, hence inducing
local production of neurohormones and
neuropeptides (Suarez et al., 2007).
Prolonged psychological stress may damage the
natural barrier of the skin and increase levels of
endogenous glucocorticoid which will also attribute
to the alteration of homeostasis and integrity, also
microbial defense of the skin itself. These are mainly
caused by the inhibition of epidermal lipid synthesis
which is mediated by glucocorticoid. Therefore,
replacement of this epidermal lipid is a promising
therapy for people who has stress related allergic
skin disorder. However, no randomised trial study
comparing the efficacy of topical therapy for
patients with stress related atopic dermatitis and
patients with non-stress related atopic dermatitis
(Walker & Papadopuolos, 2005; Suarez et al., 2007;
Steinhoff & Steinhoff, 2009).
There’s a continuous pattern where psychologic
stress causes itch in atopic dermatitis, and the itch
will in turn further cause psychologic stress and this
will continue on. Hence, psychopharmacology will
be useful in breaking this chain. The correlation
which was found between anxiety score in AD
patients who experiences pruritus and NPY and
NGF explains that anxiety causes pruritus via
increase of expression of these neuropeptides.
Therefore stress management and reduction is an
necessary approach in treating pruritus in AD
patients.
Patient with stress related AD also experiences
an increase in serotonin-sensitive mast cells.
Serotonin agonists and SSRIs improves the skin
condition and reliefs the patient from pruritus
through a poorly understood mechanism. Anti-
pruritic effect of SSRI is thought to be due to a
certain mechanism in the central nervous system.
Tandosiprone Citrate (TC), an anxiolitic serotonin
agonist, may be used in stress managements which
are related to worsening AD conditions supported by
other studies using mice models. The administration
of bupropion may show clinical improvements
through its role as anti-inflammatory agents which
lowers TNF and as inhibitor of neurotransmitter
reuptake (Steinhoff & Steinhoff, 2009; Suarez et al.,
2012).
Itchiness caused by psychologic stress is also
thought to be related to substance P (SP). The
increase of psychological stress condition causes
elevated levels of plasma SP which is then related to
the worsening of AD. Adding oral olopatadine to the
regular topical regiment helps relief itchiness and SP
plasma levels. Therefore it is thought that
olopatadine has a potential use of controlling or
reducing the level of SP caused by stress, which is
beneficial towards reducing pruritus in AD. Mice
model studies show clinical improvement after
administration of NK1R antagonists. NK1 receptors
is known to be affiliated to SP, which makes it a
Study of Psychoneuroimmunology in Atopic Dermatitis
487

possible approach for pharmacological
inverventions.
SP levels tend to remain the same, even after
remission of AD, which suggests that SP-ergic
mechanisms does not play a big role in acute clinical
changes in AD (Suarez et al., 2012; Steinhoff &
Steinhoff, 2009). The central or peripheral
mechanisms related to pruritus management is still
poorly understood. Therefore further researches
regarding these matter, including the roles of
neuropeptides as pruritogenic substances in AD
should be done. The decision for
psychoneuroalergologic management approaches in
dermatology for cases such as AD should be
supported by enough clinical evidence. A meta-
analytic review regarding psychologic stress and
atopic dermatitis proves that there is a two way
relation. These findings should receive
comprehensive efforts involving psychologic
interventions in AD management standards.
4 CONCLUSION
The mechanism underlying psychoneuroalergology
in dermatology i.e. the correlation of allergy and
psychologic stress is not fully understood. However,
new perspectives and concepts have been unveiled
from the Psychoneuroimmunology point of view.
Clinically and physiologically, psychologic stress is
shown to have direct and indirect influence towards
immune response, expression of skin neuropeptide
and skin barrier function. Several researches have
shown huge potentials in identifying new therapeutic
approaches by modulating neuroimmune systems.
Hopefully this will further improve AD management
hence reducing chronicity and recurrence rates,
lowering the burden of the disease and improving
the patient's life quality.
REFERENCES
Chida, Y., Hamer, M., Steptoe, A., 2008. A bidirectional
relationship between psychosocial factors and atopic
disorders: a systematic review and meta-analysis.
Psychosomatic Medicine 70, 102–116.
doi:10.1097/PSY.0b013e31815c1b71
Dave, N.D., Xiang, L., Rehm, K.E., Marshall, G.D., 2011.
Stress and Allergic Diseases. Immunology and Allergy
Clinics of North America.
doi:10.1016/j.iac.2010.09.009
Endaryanto, A. 2015. Allergic March. in: Implikasi Klinis
Imunologi Alergi dalam Manajemen Anak Alergi.
Airlangga University Press: pp 15-40.
Foitzik, K., Langan, E.A., Paus, R., 2009. Prolactin and
the skin: A dermatological perspective on an ancient
pleiotropic peptide hormone. Journal of Investigative
Dermatology. doi:10.1038/jid.2008.348
Suárez, A.L., Feramisco, J.D., Koo, J., Steinhoff, M.,
2012. Psychoneuroimmunology of psychological
stress and atopic dermatitis: Pathophysiologic and
therapeutic updates. Acta Dermato-Venereologica.
doi:10.2340/00015555-1188
Nordlind, K., Azmitia, E.C., Slominski, A. 2008. The skin
as a mirror of the soul: exploring the possible role of
serotonin. Experimental Dermatology; 17: 301–311.
Steinhoff, A., Steinhoff, M., 2009. Neuroimmunology of
atopic dermatitis, in: Neuroimmunology of the Skin:
Basic Science to Clinical Practice. Springer Berlin
Heidelberg, pp. 197–207. doi:10.1007/978-3-540-
35989-0_18
Buske-Kirschbaum, A., 2009. Cortisol responses to stress
in allergic children: Interaction with the immune
response. Neuro Immuno Modulation.
doi:10.1159/000216190
Walker, C., Papadopoulos, L., 2005. Psychodermatology,
Psychodermatology. Cambridge University Press,
London Metropolitan University, United Kingdom.
doi:10.1017/CBO9780511544170.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
488
