
Oral Hairy Leukoplakia: A Predictor and Prognostic Factor of HIV
Infection
Yusuf Wibisono, Septiana Widyantari, Cita Rosita Sigit Prakoeswa
Department of Dermato-Venereology, Faculty of Medicine,Universitas Airlangga/Dr. Soetomo General Hospital Surabaya,
Indonesia
Keywords: Oral Hairy Leukoplakia, HIV, Acyclovir, ARV
Abstract: Introduction: Oral hairy leukoplakia (OHL), also known as benign hyperplasia of oral mucosa, is an
asymptomatic white corrugated plaque that is most commonly found on the lateral borders of the tongue.
This condition is caused by Epstein-Barr Virus (EBV). OHL is commonly found in immunocompromised
patient, with the prevalence around 20-25% among HIV patients and indicates decline of CD4 counts. Case:
A 29 year-old-male came to the Dermato-Venereology Outpatient Clinic of Dr. Soetomo General Hospital
Surabaya with complaint of persistent asymptomatic whitish color on lateral side of his tongue. From
history taking, the lesion was first appeared all over the tongue, and after consumption of antifungal
treatment, the lesion subsided and persisted only on lateral border of the tongue. There were history of
diarrhea, fever and cough for almost 1 month. He also has multiple sexual partners. From physical
examination, we found painless white demarcated plaque with corrugated appearance on the left lateral
border of the tongue. Further examination on HIV panels using three methods showed reactive result. Based
on history taking, clinical and laboratory findings, the patient was diagnosed with OHL and HIV. The
patient was treated with Acyclovir 800 mg, 5 times daily, and HAART (Duviral 2x1 tab + Neviral 1x1 tab).
After 2 weeks of treatment, the lesion disappeared. Conclusion: The appearance of OHL is commonly
associated with immunocompromised condition. The establishment of OHL has a diagnostic value for HIV
infection. Systemic antiviral therapy and prevention of recurrence using antiretroviral medication showed
satisfying result.
1 INTRODUCTION
Oral Hairy Leukoplakia (OHL) which also known as
benign epithelial hyperplasia of oral mucosa, is an
oral mucosal lesion associated with infection and
replication of the Epstein-Barr virus (EBV)
(Murtiastutik et al., 2008). The clinical presentation
of OHL is a painless, white proliferative oral
epithelial lesion that usually occured on the lateral
margins of the tongue.
This white patch is non-
removable, with wide variation in size, severity, and
surface characteristics.
OHL has been listed in the classification of oral
lesions as a Group I lesion strongly associated with
HIV infection (Classification and diagnostic criteria
for oral lesions in HIV infection, 1993; Uihlein et
al., 2011). It is also considered as a marker of poor
prognosis that frequently precedes the onset of
acquired immunodeficiency syndrome (Kreuter &
Wieland, 2011).
The lesion usually presents itself
when the CD4 cell counts fall below 0.3x10
9
/L
(Bravo et al., 2006).
However, OHL is also found in
other immunosuppressive non-HIV condition, such
as transplant recipients, in patients with
hematological malignancies, and in patients required
under systemic steroid treatment (Piperi et al.,
2010).
HIV is a lymphotropic human retrovirus, which
is predominantly transmitted through sexual contact.
HIV is also transmitted through exposure to infected
blood (i.e needles shared by injecting drug users)
and transmission from infected mother to her infant
during pregnancy, delivery or breastfeeding (Uihlein
et a., 2011). OHL has been associated with more
rapid progression to AIDS with HIV viral loads
exceeding 20.000 copies/ml, and with CD4+ counts
below 200/mm
8
or 0.3x10
9
/L (Bravo et al., 2006).
A case of OHL in 29-year-old patient who was later
diagnosed with HIV positive is reported. The
diagnosis was established by history taking, physical
Wibisono, Y., Widyantari, S. and Prakoeswa, C.
Oral Hairy Leukoplakia: A Predictor and Prognostic Factor of HIV Infection.
DOI: 10.5220/0008160805050509
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 505-509
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
505

examination, and later the establishment of HIV
diagnose. This report discusses the clinical
manifestation, diagnosis and treatment of this
condition.
2 CASE
A twenty-nine-year-old Javanese male came to the
Outpatient Clinic of Dermato-Venereology
Department at Dr. Soetomo General Hospital
Surabaya with the chief complaint whitish color all
over the tongue since 2 months before visitation. He
went to see doctor and was diagnosed with fungal
infection and then prescribed ketoconazole 1 x 200
mg daily for 4 weeks. The whitish color on the
middle part has gone, but parts on the borders still
persist. The patient tried to remove the whitish color
with tooth brush but there was no result.
The patient also complained of cough and fever
for more than 2 weeks. There was also complaint of
watery stool for 1 month and report of weight loss
and loss of appetite. There was history of sexual
relationship with multiple partners. History of sexual
transmitted disease was denied. Patient has
homosexuality preference.
The dermatological examination on his tongue
showed bilateral painless white well demarcated
plaque with corrugated appearance on the lateral
borders of the tongue. The lesion can not be scrub
off. Other physical examinations revealed normal
findings.
The patient was consulted to the UPIPI
outpatient clinic to have Voluntary Counseling and
Testing (VCT) for HIV, and was told to do Rapid
test and blood and urine examination. The HIV test
result for all three methods (Imunochromatography,
Imunodot, ELISA) were reactive.
The patient was then consulted to the internal
department, and was diagnosed with s HIV stage 3.
Complete blood count examination was conducted
and the result was within normal limit. The absolute
CD4 count was performed, and it was obtained that
the absolute CD4 count was 1 cells/uL and CD4
percentage was 0.05%, considered as a very low
CD4 count. The patient was also consulted to
pulmonology department, and based on chest x ray
and acid fast stain there was no abnormalities found,
so the assessment of tuberculosis can be excluded.
A cytopathology examination was performed by
scrapping of the lateral border of the tongue. From
the examination, there was squamous epithelial and
mononuclear inflammatory cells present. There was
no dysplasia cell founded. Based on those result, it
concluded that this condition caused by
microorganism infection, and not a malignancy
process.
Based on history taking, clinical findings and the
laboratory examination, the patient was then
diagnosed with Oral Hairy Leukoplakia and AIDS.
The diagnosis of AIDS in this patient was obtained
from the presence of OHL, reactive results of HIV
panel test, and the CD4 cell count below 200/μL.
The patient was then treated with acyclovir 800
mg, administered 5 times a day, along with the
administration of cotrimoxazole 1 times 960 mg as a
Cotrimoxazole Prevention Treatment 2 weeks before
starting the HAART. After 1 week of treatment, the
lesion on the lateral border had subsided, the therapy
was then continued for another week to make sure
the lesion has totally disappeared. Clinical
progression of the lesion
After outpatient clinic visit until the end of
February 2017, patient no longer came to Dermato-
venerology outpatient clinic. When we tried to
contact the patient, he said he already moved to
Papua for business affairs, and never come back to
Surabaya ever since.
3 DISCUSSION
Oral hairy leukoplakia is a specific lesion in HIV
infection caused by Epstein Barr virus, and has been
reported in over more than 28% patients and is a
sign of disease progression (Murtiastutik et al.,
2008)
OHL appear clinically as an asymptomatic,
white or grayish white, well demarcated plaque with
corrugated texture. The “hairy” surface vary in size
and typically occurs on the lateral tongue. The lesion
is painless and irremovable by blunt manipulation
(Triantos et al., 1997).
In our case, the patient complaint loss of appetite
regarding the lesion on his tongue. He was first
treated with ketoconazole 1 x 200 mg. After given
treatment for 4 weeks, the lesion subsided, but the
lesion on both lateral borders persist. No pain,
wound or swelling was reported.
EBV primarily transmitted through saliva as
infected cells are shed into the surface of the oral
mucosa. Primary infection activates the innate and
adaptive immune systems, and the virus remains
latent lifelong by living in circulatory B
lymphocytes, which serve as the cellular reservoir
(Walling et al., 2003).
Severe immunosuppressive
condition can lead into reactivation of EBV
replication in the oropharynx of EBV-seropositive
patients (Cruchley et al., 1989).
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
506
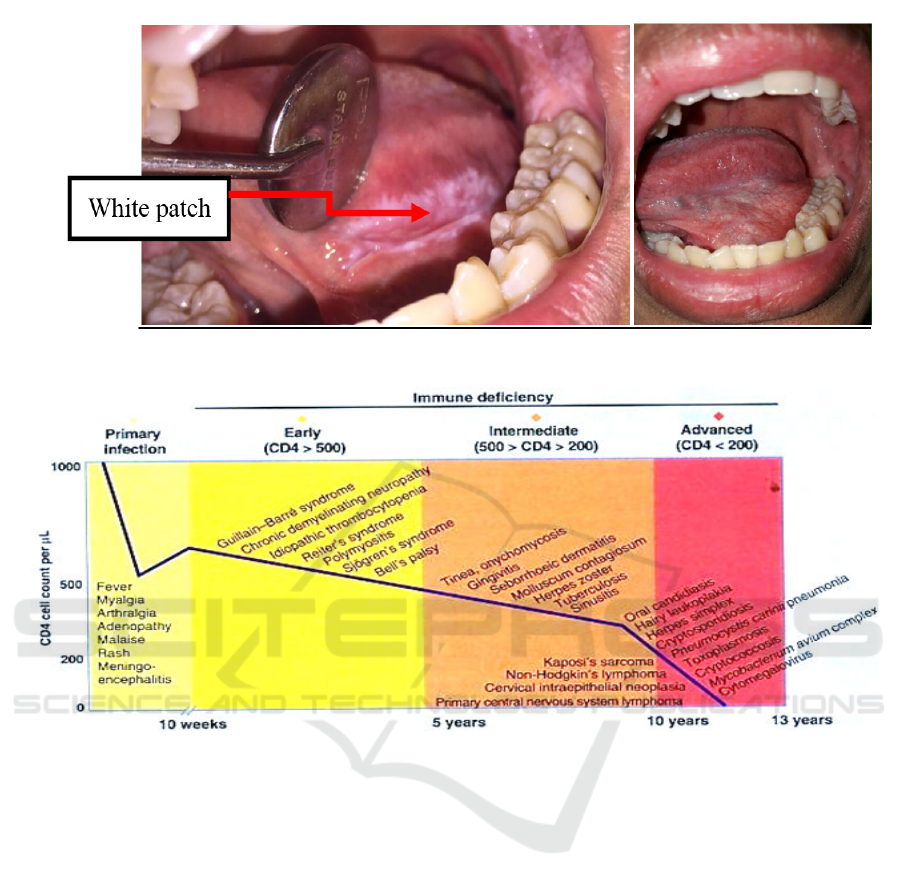
Figure 1: Patient’s clinical condition before (left) and after 2-weeks-treatment (right).
Figure 2: Opportunistic Infections Correlating with CD4+ Cell Count
11.
The lateral border of the tongue is the most
common location of OHL. The development of on
the tongue may be due to the accumulation of saliva
in the floor of the mouth (Piperi et al., 2010).
The
lateral border of the tongue is also an area which
prone to trauma, thus becomes a predilection area.
Another explanation is the decreased number of
Langerhans cells in OHL lesions compared with non
lesional oral mucosa. A comparative study of normal
mucosa revealed that the lowest density of
Langerhans cells was found on the lateral border of
the tongue and the sublingual region. Thus normal
epithelium of the lateral and ventral sides of the
tongue is more susceptible to EBV infection
(Cruchley et al., 1989).
In our patient, from physical examination we
found bilateral painless white well demarcated
plaque with corrugated appearance on the lateral
borders of the tongue, in accordance with the usual
location of OHL, which is on the lateral borders of
the tongue.
The importance of OHL as an indicator of
immunosuppressive condition was recognized soon
after it was first described in 1984 (Greenspan et al.,
1984). OHL has been listed in the classification of
oral lesions as a Group I lesion strongly associated
with HIV infection (Classification and diagnostic
criteria for oral lesions in HIV infection, 1993).
In this patient, after the initial diagnosis of OHL,
the patient was then referred to do VCT. The HIV
panel test result was reactive, which explain the
immunocompromised condition as predisposing
factor of OHL. OHL findings in patients with HIV
can also provide some predictive immunity
condition of how progressive the infection is, as it is
believed to have correlation with CD4 T cell counts.
The absolute CD4 count of the patient was 1
cells/uL (N = 410-1590 cells/uL) and CD4
percentage was 0.05% (N = 31-60%), which
Oral Hairy Leukoplakia: A Predictor and Prognostic Factor of HIV Infection
507

considered as a very low CD4 count.This is in
accordance with data provided in figure 2, where
OHL is correlated with CD4 T cell counts <200/μL.
According to WHO clinical staging of
HIV/AIDS for Adults and Adolescents, patient with
OHL is classified as HIV stage 3, (WHO, 2007)
but
CDC stated that when the number of CD4 cells falls
below 200 cells/mm, the patient is considered as
AIDS. (Greenspan et al., 1984). Diagnosis of AIDS
can also be established when one or more
opportunistic infection occured, regardless of the
CD4 count.
Therefore the patient was diagnosed
with OHL and AIDS.
In order to diagnosed patient with EBV infection,
further examination to obtain EBV in the lesion
needed. This can be done by performing
histopathology, exfoliative cytology, in situ
hybridization (ISH), or PCR examination. The most
common histopathological features of OHL include
hyperparakeratosis, epithelial hyperplasia, koilocyte-
like cells within the prickle cell layer and minimal or
complete absence of inflammatory cells in the
lamina propria. A band-like layer of cells with clear
cytoplasm (ground glass appearance) with basophilic
nuclear inclusions, ballooning of cytoplasm and
intracellular edema can also be seen in the upper
spinous layer (Davis et al., 2017).
In our patient, the result of cytopathology
examination does not specific for OHL. A study
revealed that only 50% of HIV patients with clinical
OHL had nuclear change (Reginald et al., 2017).
Suggestive clinical findings, the typical involvement
of lateral borders, the lack of response to
ketoconazole treatment and the patient’s HIV status
is sufficient to make the diagnosis.
The differential diagnosis of OHL include oral
candidiasis, lichen planus, tobacco-associated
leukoplakia, frictional keratosis, human papilloma
virus–induced oral intraepithelial neoplasia, and oral
squamous cell carcinoma (Radwan Ozcko &
Mendak, 2011). In most instances, OHL can be
diagnosed clinically and does not require a
confirmatory biopsy (Triantos et al., 1997).
OHL is a disease of minimal morbidity that does
not always require intervention. Therapy is indicated
when symptoms become troubling or when it is
associated with HIV infection. Treatments for OHL
when required consist of varying options. Usually
the institution of highly active antiretroviral therapy
(HAART) will reduced viral load and increased CD4
count which help decreasing prevalence of OHL
significantly. Other therapeutic options including
systemic antiviral agents such as acyclovir and
valacyclovir, topical podophyllin, topical retinoids,
cryotherapy and surgical excision (Triantos et al.,
1997; Uihlein et al., 2011).
In our case, the patient was administered
acyclovir 800 mg oral 5 times daily, which is
corresponding with guidelines in the literature, for 2
weeks.After the 1
st
week, the lesion on the lateral
borders had subsided, the therapy was then
continued for another week to make sure the lesion
has totally disappeared. The institution of HAART
could also prevent the recurrence of OHL in this
patient.
4 CONCLUSION
Oral hairy leukoplakia is a predictor and prognostic
factor of HIV infection. It cannot be occured in
immunocompetent patient so immunocompromised
condition which can be caused by HIV must be ruled
out before considering other immunocompromised
etiologies. Oral manifestations are the earliest and
most important indicators of HIV infection. OHL is
often misdiagnosed and thus proper treatment is
delayed.
In early diagnosis of OHL, health care provider
must be cautious for and perform further
examination to establish the diagnosis of HIV
infection. Institution of HAART on HIV-related
OHL patient significantly decline the prevalence of
OHL. Other treatments such as systemic antiviral
accelerate the resolution process. The ability to
recognize early OHL manifestation in patient with
HIV is key to providing optimal and appropriate
care, administer early medical intervention and thus
prolonging patient’s life and improve their quality of
life.
REFERENCES
Bravo, I.M., Correnti, M., Escalona, L., Perrone, M.,
Brito, A., Tovar, V., Rivera, H., 2006. Prevalence of
oral lesions in HIV patients related to CD4 cell count
and viral load in a Venezuelan population. Medicina
oral, patología oral y cirugía bucal 11, E33-9.
Classification and diagnostic criteria for oral lesions in
HIV infection: EC‐Clearinghouse on Oral Problems
Relatedto HIV Infection and WHO Collaborating
Centre on Oral Manifestations of the
Immunodeficiency Virus, 1993. . Journal of Oral
Pathology & Medicine 22, 289–291.
doi:10.1111/j.1600-0714.1993.tb01074.x
Cruchley, A.T., Williams, D.M., Farthing, P.M., Lesch,
C.A., Squier, C.A., 1989. Regional variation in
Langerhans cell distribution and density in normal
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
508

human oral mucosa determined using monoclonal
antibodies against CD1, HLADR, HLADQ and
HLADP. Journal of Oral Pathology & Medicine:
Official Publication of the International Association of
Oral Pathologists and the American Academy of Oral
Pathology 18, 510–516.
Davis, G., Perks, A., Liyanage, P., Staines, K., 2017. Oral
hairy leukoplakia arising in a patient with hairy cell
leukaemia: The first reported case. BMJ Case Reports
2017. doi:10.1136/bcr-2016-218663
Graeme, J.S., Irvine, S.S., Scott, M., Kelleher, A.D.,
Marriott, D.J.E., McKnight, I., Pethebridge, A.M.,
Wodak, A., Ziegler, J. 1997. Editors. Strategies of
care in managing HIV. In Managing HIV. Sydney:
Australasian Medical Publishing Company Limited.
Greenspan, D., Greenspan, J.S., Conant, M., Petersen, V.,
Silverman, S. Jr., De Souza, Y. 1984. Oral “hairy”
leukoplakia in male homosexuals: evidence of
association with both papillomavirus and a herpes-
group virus. Lancet 2:831-4.
Kreuter, A., Wieland, U., 2011. Oral hairy leukoplakia: A
clinical indicator of immunosuppression. CMAJ 183,
932. doi:10.1503/cmaj.100841
Murtiastutik, D. 2008. Kelainan kulit pada pasien
HIV/AIDS. Dalam: Barakbah, J., Lumintang, H.,
Martodihardjo, S., editor. Infeksi Menular Seksual.
Surabaya. AUP : 258-59.
Piperi, E., Omlie, J., Koutlas, I.G., Pambuccian, S., 2010.
Oral hairy leukoplakia in HIV-negative patients:
Report of 10 cases. International Journal of Surgical
Pathology 18, 177–183.
doi:10.1177/1066896908327865
Radwan-Ozcko, M., Mendak, M. 2011. Differential
diagnosis of oral leukoplakia and lichen planus – on
the basis of literature and own observations. J Stoma;
64, 5-6: 355-370
Reginald, A., Sivapathasundharam, B., 2010. Oral hairy
leukoplakia: An exfoliative cytology study.
Contemporary clinical dentistry 1, 10–3.
doi:10.4103/0976-237X.62512
Triantos, D., Porter, S.R., Scully, C., Teo, C.G., 1997.
Oral hairy leukoplakia: clinicopathologic features,
pathogenesis, diagnosis, and clinical significance.
Clinical infectious diseases : an official publication of
the Infectious Diseases Society of America 25, 1392–6.
doi:10.1086/516131
Uihlein, L.C., Saavedra, A.P., Johnson, R.A. Cutaneous
manifestations of human immunodeficiency virus
disease. 2011. In: Goldsmith, L.A., Katz, S.I.,
Gilchrest, B.A., Paller, A.S., Leffell, D.J., (eds).
Fitzpatrick’s Dermatology in General Medicine. 8
th
ed. New York : Mc Graw Hill . p.2439-2455
Walling, D.M., Flaitz, C.M., Nichols, C.M., 2003.
Epstein-Barr virus replication in oral hairy
leukoplakia: response, persistence, and resistance to
treatment with valacyclovir. The Journal of infectious
diseases 188, 883–90. doi:10.1086/378072
World Health Organization. 2007. WHO Case Definitions
of HIV for Surveillance and Revised Clinical Staging
and Immunological Classification of HIV-Related
Disease in Adults and Children; 15-16
Oral Hairy Leukoplakia: A Predictor and Prognostic Factor of HIV Infection
509
