
Correlation between Psychological Distress with Level of
Methamphetamine Dependence in Male Chronic Methamphetamine
Users in the Rehabilitation Center of North Sumatra Province
Vita Camellia
1
, M. Surya Husada
1
, Fasihah Irfani
2
and Dudy Aldiansyah
3
1
Department of Psychiatry, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
2
Department of Neurology, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
3
Department of Obstetric and Gynecology, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
Keywords: Psychological Distress, Dependence Level, Chronic Amphetamine Users.
Abstract: The aim of this study was to find the correlation between psychological distress and level of
methamphetamine dependence in male chronic methamphetamine users. Drug users have fulfilled the
inclusion criteria, has been done detoxification, male, methamphetamine use disorder, not psychotic. The
exclusion criteria are those who have general medical illnesses based on the history of the disease, have a
history of previous head trauma and organic mental illnesses. Structured interviews with MINI ICD-10 to
determine subject is indeed a substance use disorder. To know the psychological distress, we determine it
with the Hospital Anxiety and Depression Scale (HADS), and to see the score level of dependence, we used
WHO ASSIST (The Alcohol, Smoking and Substance Involvement). The study found that out of 88 males
subjects with methamphetamine use disorder. The median of dependency level score is 30.5 (6-41), and mean
of HADS score is 15.67 (4.76). This study obtained Pearson correlation of psychological distress level scores
and dependency level scores with r = 0.242, p = 0.023. There is a significant weak correlation between
psychological distress level scores and dependency level scores.
1 INTRODUCTION
Methamphetamine dependence is a serious public
health problem in the world with medical, psychiatric,
cognitive, socioeconomic and legal consequences.
The use of amphetamine is ranked second after
cannabis as the most commonly used prohibited
substance worldwide. Globally it is estimated that
33.8 million people aged 15-64 years are
methamphetamine-dependent (Glasner-Edwards et
al., 2009; Karila et al., 2010; Marshall et al., 2011;
Opsal et al., 2013). In Indonesia, drug abuse among
students in 2018 from 13 provinces reached 2.29
million people and one of the community groups
prone to drug abuse are those who are in the 15-35
year range or millennial generation (PUSLITDATIN,
2019).
Glasner-Edwards et al., (2009) found that
symptoms of depressive pre-treatment had clinical
significance in the attachment to treatment and
became a chronic condition of depression, symptoms
and depressive syndrome at the end of treatment and
follow-up (in the next 30 days) showed the
association of Initial use of methamphetamine and
abstinence from methamphetamine with decreased
symptomatology of depression and major depressive
disorders associated with greater overall severity in
methamphetamine users.
Depression and anxiety often occur in
methamphetamine users, short-term abstinence can
improve depression and quality of life but do not
improve anxiety in methamphetamine abusers.
In chronic methamphetamine users, repeated and
sustained release of monoamine in central nervous
system (CNS) has a major role in the chronic
neurological influence of methamphetamine abusers.
Frequent use causes dopamine depletion in CNS and
damages the dopamine and serotonin terminals.
Damage to monoamine neurotransmission has
important effects on brain circuits and mood
regulation and also functions of self-control,
motivation, cognitive performance, and
psychological stress. These changes bring the user
unable to be happy without substances (anhedonia)
which makes it easier to cause severe depression.
322
Camellia, V., Husada, M., Irfani, F. and Aldiansyah, D.
Correlation between Psychological Distress with Level of Methamphetamine Dependence in Male Chronic Methamphetamine Users in the Rehabilitation Center of North Sumatra Province.
DOI: 10.5220/0010181100002775
In Proceedings of the 1st International MIPAnet Conference on Science and Mathematics (IMC-SciMath 2019), pages 322-325
ISBN: 978-989-758-556-2
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

During abstinence and release of substances, the
patient will experience different symptoms. These
symptoms are related to recurrence of substance use.
This study wants to find the correlation between
psychologic distress and the level of
methamphetamine dependence on chronic users, after
detoxification at a rehabilitation center in Northern
Sumatra, Indonesia.
2 METHODS
Subjects were chronic methamphetamine users who
underwent treatment in the rehabilitation of the
province of North Sumatra (research period May to
November 2019) who had fulfilled the inclusion and
exclusion criteria as research subjects.
Inclusion criteria:
Detoxification has finished;
Has used methamphetamine for more than a year;
Criteria for mental behavioral disorders due to
methamphetamine use are met;
The sample has a dependency level score based on
WHO ASSIST (The Alcohol, Smoking and
Substance Involvement
) > 4;
Willing to participate in research;
Minimum education in junior high.
Exclusion criteria:
Has a history of previous medical ailments;
Have been treated by a psychiatrist before;
Has an organic mental disorder;
Have psychotic symptoms.
2.1 Procedure
A total of 88 males subjects will have a urine drug test
to ensure that the subject has abstained and completed
detoxification then a structured interview with MINI
(The Mini International Neuropsychiatric Interview)
according to ICD-10 to establish a diagnosis of
mental behavioral disorders due to substance use.
Hospital Anxiety and Depression Scale (HADS) to
see the problems of depression symptoms and their
anxiety or psychological distress with the sum score
on each depression or anxiety scale having a range of
0-21 and Ozalp said that the total score ≥ 17 is optimal
for identifying affective psychopathology cases
(Ozalp et al., 2008; Zigmond & Snaith, 1983). To see
the level of dependency, the WHO ASSIST
questionnaire was used. it is made for use by all
cultures and can be used in different cultures. To
screen tobacco, alcohol, cannabis/cocaine,
amphetamine and sedative/hypnotic/ benzodiazepine
stimulants, hallucinogens, inhalants, opioids, and
other substances (WHO, 2010).
WHO ASSIST determine the risk score of each
substance used to discuss appropriate interventions
with substance users. WHO ASSIST consists of eight
questionnaire items which were carried out within 5
minutes. WHO ASSIST gets information about
substance users throughout the life and related to
problems throughout the last three months and values:
0 (never); not using the last three months;
1 (one or two times); up to twice in the last three
months;
2 (every month); an average of 1-3 times per
month for three months;
3 (every week); 1-4 times every week;
4 (every day); 5-7 times per week or almost every
day.
History of substances used, types of substances,
and the degree of dependence measure with WHO
ASISST can determine the type of intervention used.
If the WHO ASSIST score 0-3, it does not require
intervention, a score of 4-26 requires a brief
intervention and a score of more than 27 require more
intensive treatment, and to see the demographic
characteristics and background of the environment
and family factors, a questionnaire will be used which
will be filled out by the subjects.
2.2 Statistical Analysis
The data is analyzed whether the distribution is
normal or not with the normality test, if it is not
normally distributed then a non-parametric test is
performed to see the correlation between the level of
psychological distress and the level of dependence
that is the Pearson correlation test. It is meaningful if
p < 0.05, using SPSS.
3 RESULTS
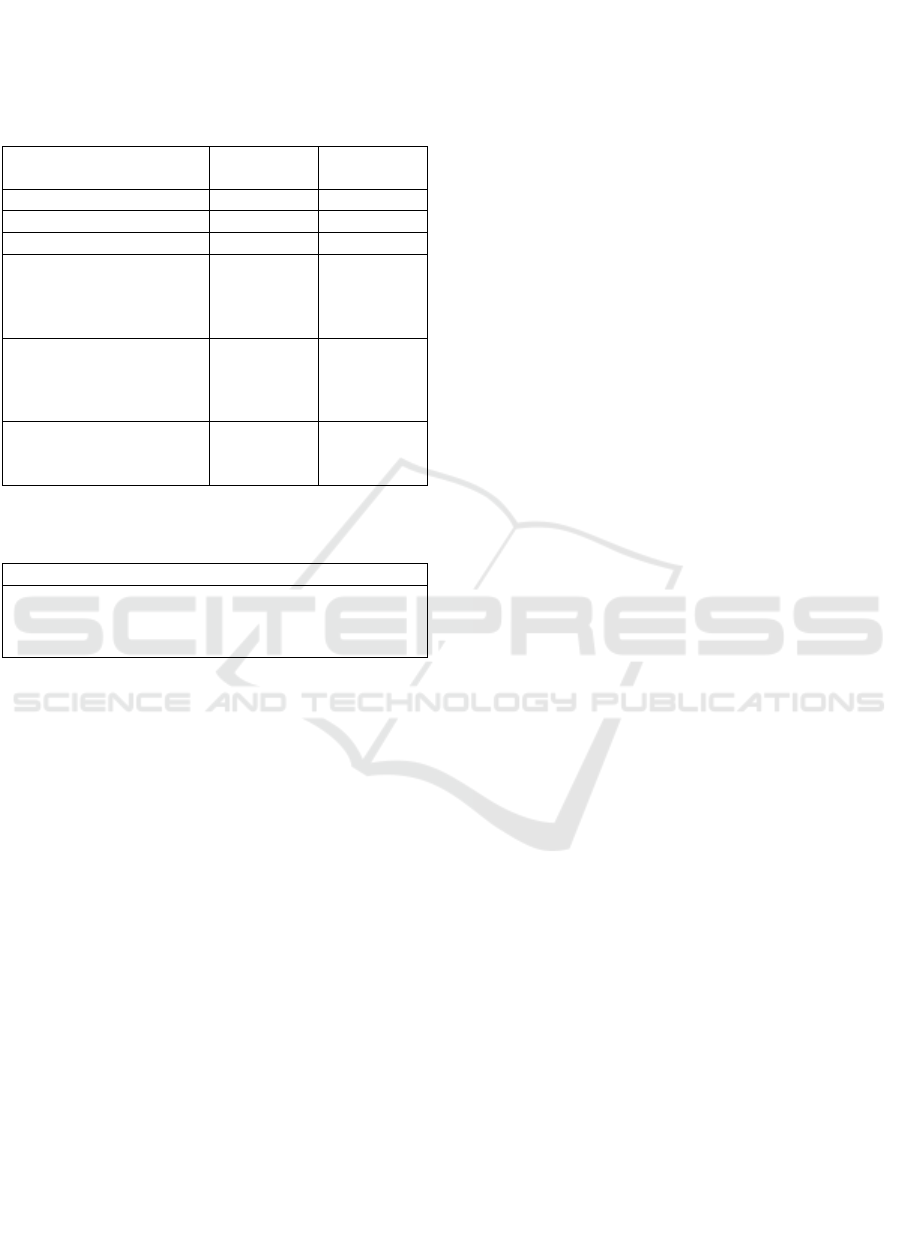
This study found that (see table 1) out of a total of 88
males chronic methamphetamine users had an age
range (years) with a median value of (min-max) being
24 (15-40) years, the median age for first use is 18
(12-33) years, and the median of use duration is 5 (1-
21). According to the marital status, the dominant
ones are 53 subjects (60.2%) who have not been
married, in education level (senior high school) is 78
subjects (88.6%), and 58 subjects (65.9%) are
employed. The score of level of dependency was
found median (min-max) namely 30.5 (6-41). HADS
score with a mean (standard deviation) is 15.67
(4.76). This study obtained Pearson correlation of
Correlation between Psychological Distress with Level of Methamphetamine Dependence in Male Chronic Methamphetamine Users in the
Rehabilitation Center of North Sumatra Province
323
psychological distress level scores and dependency
level scores with r = 0.242 and p = 0.023 (see table
2).
Table 1: Characteristics of chronic methamphetamine users
with Substance use disorders.
Variable n (%)
Median
(
min-
m
ax
)
A
g
e 24
(
15-40
)
A
g
e of first time use
r
18
(
12-33
)
Duration of use 5 (1-21)
Marital Status
Single
Married
Divorce
53 (60.2)
27 (30.7)
8
(
9.1
)
Education level
Junior high
Senior high
Academic de
g
ree
8 (9,1)
78 (88.6)
2
(
2,3
)
Occupation
Employed
Unem
p
lo
y
e
d
58 (65.9)
30
(
34.1
)
Table 2: Correlation of HADS scores and
Methamphetamine dependency scores.
HADS score
WHO ASSIST r = 0.242
score p = 0.023
n = 88
Pearson correlation test
4 DISCUSSION
This study found that the higher the level of
dependence of chronic methamphetamine users show
a higher level of psychological distress, although this
correlation shows a significant relationship with a
positive correlation, but the relationship shown is a
weak relationship. This study found the average
HADS (Hospital Anxiety and Depression Scale)
score showed a high level of psychological distress
that is above the cut-off. And the level of the
dependence of chronic methamphetamine users more
than half is above a score of 30.5. Which shows a high
level of dependency. All respondents who were
predominantly educated were high school and
unmarried and according to Gywali, et al, that risk
factors for depression and anxiety among patients
with substance use disorders in western countries that
have been reported were female, younger age, low
family income and single. Gyawali et al., (2016)
found in their study that 51.1% who were treated at
the Kathmandu Hill medical center experienced high
psychological distress symptoms by using the Kessler
psychological distress instrument with multivariate
analysis showing various factors related to
psychologic distress symptoms including age,
education, the severity of substance abuse using the-
10 DAST and family function.
Glassner-Edwards et al., (2010) who assessed
psychiatric problems, substance use and functional
outcomes of methamphetamine users with
concomitant anxiety disorders three years after
treatment. That anxiety disorders are associated with
poor drug and alcohol use, high health service use and
high psychiatric symptoms including suicide.
Emphasis on symptoms and anxiety syndromes in
methamphetamine users can help to optimize
meaningful treatment outcomes. Studies have shown
that high symptoms of anxiety and depression affect
help-seeking behaviors such as getting diagnosed and
treated for substance abuse disorders, which also
affect treatment adherence, decreased quality of life,
increased risk of breathing, increased social isolation
and the risk of premature death.
This study found that half of the respondents who
underwent rehabilitation were using
methamphetamine for less than five years and half
had rehabilitation after using methamphetamine more
than five years. This shows the religiosity in seeking
treatment which is in line with the research of Lee et
al., (2012) found that previous mental health
problems were high and at present from respondents
using methamphetamine, they found as many as 22%
(18 people) reported mental health problems
preceding methamphetamine use and as many as 72%
reported having mental health problems after regular
methamphetamine use the first time and around the
same time as problematic methamphetamine users
(Lee et al., 2012). Respondents identified a time delay
of five years between the time of the first problematic
use of methamphetamine and the search for a
treatment for problems related to methamphetamine.
This study also found that half of the respondents
started using methamphetamine under the age of 18,
the earliest is 12 years old and the latest is 33 years
old. While the duration of using of respondents is
stretched from five years to 21 years. The
interconnection of substance use and psychological
distress from adolescents (aged 16 years) to half-life
(age 47 years) and continual use over time in African
Americans (in cohorts), they found substance use,
alcohol and ongoing psychological distress from
adolescence to middle age in men and women. Also
found that substance use in adolescents predicts
greater psychological distress in young adulthood in
groups of men.
IMC-SciMath 2019 - The International MIPAnet Conference on Science and Mathematics (IMC-SciMath)
324

The explanation for psychological distress and
substance use problems is self-medication. People
who use psychoactive substances to alleviate
psychological symptoms, another explanation that the
use of substances causes psychological distress. The
use of substances including intoxication and
substance release can induce symptoms of anxiety
and depression, which will then change
spontaneously with the cessation of use and reduction
of withdrawal symptoms. Furthermore, the use of
substances can cause prolonged psychological
distress due to the consequences of the use of putting
the individual on a long journey of loss.
This study suggests that it is necessary to detect
the presence of psychological distress in chronic
methamphetamine users before detoxification, post-
detoxification to determine the appropriate treatment
according to the individual's needs. Stuart et al.,
(2017) stated that various studies supporting
psychologic treatments that combine elements of
psychotherapy, psychoeducation and relapse
prevention are the main treatments for
methamphetamine users who focus on abstinence and
reduce mental health symptoms, including cognitive
behavioral therapy and motivational interviewing
approaches that have been shown to be effective in
reducing the use of methamphetamine focusing on
abstinence and reducing mental health symptoms,
including cognitive-behavioral therapy and
motivational interviewing approaches that have been
shown to be effective in reducing the use of
methamphetamine and depressive symptoms in
people who use methamphetamine.
ACKNOWLEDGEMENTS
This study funded by DRPM of Ministry of Research
Technology and High Education of the Republic of
Indonesia.
REFERENCES
Glasner-Edwards, S., Marinelli-Casey, P., Hillhouse, M.,
Ang, A., & Mooney, L. (2009). Depression among
methamphetamine users: association with outcomes
from the methamphetamine treatment project at 3-year
follow-up. J Nerv Ment Dis, 197(4), 225–231.
Glassner-Edwards, S., Mooney, L., Marinelli-Casey, P.,
Hillhouse, M., & Ang, A. (2010). Anxiety disorders
among methamphetamin dependent adults: association
with posttreatment functioning. Am J Addict, 19(5),
385–390.
Gyawali, B., Choulagai, B., Paneru, D., & Ahmad, M.
(2016). Prevalence and correlates of psychological
distress symptoms among patients with substance use
disorders in drug rehabilitation centers in urban Nepal:
a cross-sectional study. BMC Psychiatry, 16, 314.
Karila, L., Weinstein, A., Aubin, H., Benyamina, A., &
Reynaud, M. (2010). Pharmacological approaches to
metamphetamin dependence: a focused review. Br J
Clin Pharmacol, 69(6), 578–592.
Lee, N., Harney, A., & Pennay, A. (2012). Examining the
temporal relationship between methamphetamine use
and mental health comorbidity. Advances in Dual
Diagnosis, 5(1), 23–31.
Marshall, B., Wood, E., Shoeveller, J., Buxton, J.,
Montaner, J., & Kerr, T. (2011). Individual, social and
environtmental factors associated with initiating
methamphetamine injection: implications for drug use
and HIV prevention strategies. Prev Sci, 12(2), 173–
180.
Opsal, A., Kristensen, O., Larsen, T., Syversen, G., &
Rudshaug, E. (2013). Factors associated with
involuntary admissions among patients with substance
use disorders and comorbidity: a cross-sectional study.
BMC Health Services Research, 13, 57.
Ozalp, E., Soygur, H., Cankurtaran, E., Turhan, L.,
Akbiyik, D., & Geyik, P. (2008). Psychiatric morbidity
and its screening in Turkish women with breast cancer:
a comparison between the HADS and SCID test.
Psychooncology, 17, 668–675.
PUSLITDATIN. (2019). Penggunaan narkotika di
kalangan remaja meningkat.
Stuart, A., Baker, A., Bowman, J., McCarter, K., & Denhan,
A. (2017). Protocol for systematic review of
psychological treatment for methamphetamine use: an
analysis of methamphetamine use and mental health
symptom outcomes. BMJ, 7, e015383.
WHO. (2010). ASSIST the alcohol, smoking and substance
involvement screening test. WHO Library Cataloguing
in Publication Data.
Zigmond, A., & Snaith, M. R. (1983). The hospital anxiety
and depression scale. Acta Psychiatr Scand, 67, 361–
370.
Correlation between Psychological Distress with Level of Methamphetamine Dependence in Male Chronic Methamphetamine Users in the
Rehabilitation Center of North Sumatra Province
325
