
Using a Hybrid Simulation Model to Maximize Patient Throughput
of Magnetic Resonance Imaging in a Medical Center
Li-Hui Lee
1 a
, Yang-Yu Ou
1
, Yu-Ting Cheng
*1
, Ying-Chou Sun
2
, Hsiu-Mei Wu
2
and
Wan-You Guo
2
1
Department of Health Care Management, National Taipei University of Nursing and Health Sciences, No. 89,
Neijiang Street, Wanhua District, Taipei City, Taiwan
2
Department of Radiology, Taipei Veterans General Hospital, No.201, Sec. 2, Shipai Rd., Beitou Dist.,
Taipei City 112, Taiwan
Keywords: Agent-based, Magnetic Resonance Imaging, Waiting Time, Throughput, Cost-effectiveness Analysis.
Abstract: The purpose of this study is to shorten the waiting time of a patient to undergo a magnetic resonance imaging
(MRI) examination as well as to increase the utilization rates of the five MRI scanners in a 2,735-bed medical
center of Taiwan. We simulate the current MRI examination workflow through a hybrid simulation model,
consisting of discrete event and agent-based simulations. Then, we maximize the MRI patient throughput per
day with more radiographers during current business hours. For reasons of feasibility, a cost-effectiveness
analysis is also conducted. AnyLogic, Excel, and SAS were used for building the simulation models and
conducting the statistical analysis. The results show that providing 248 additional patient examinations with
one additional radiographer employed during the 11:00 to 19:00 time frame would shorten the waiting time
of a patient to undergo an MRI examination by 2.51 days, increase the utilization rate of each MRI scanner
by an average of 6.15%, and bring an additional gross income of US$38,424 to US$69,169 per 31-day month.
1 INTRODUCTION
For decades, high-tech medical imaging scanners,
such as magnetic resonance imaging (MRI), have
been widely used in the examination, diagnosis and
tracking of various diseases and in the detection of
cancer stages and the determination of cancer
metastasis position. With the improvement of
personal health awareness and the rapid
dissemination of health-related information through
the Internet, people pay more attention to their health
status and that of their family members than before.
Precise preventive photographic examination in
medical institutions or health examination centers is
becoming increasingly common (Global Views, 2015,
National Health Insurance Administration Ministry
of Health and Welfare, 2018b).
To meet the needs of MRI examination, the
number of medical imaging scanners in some
countries has been increasing yearly. According to
the Organization for Economic Co-operation and
Development (OECD) statistics up to 2017, the U.S.
a
https://orcid.org/0000-0003-0377-7459
has more scanners than any other European or
American country, at 37.6 scanners per million
people. Germany and Italy are in second and third
places at 34.5 and 28.4 scanners per million people,
respectively. Asia ranks first in the world with 51.7
scanners per million people in Japan, followed by
29.1 scanners per million people in South Korea.
According to the statistics of the Central Health
Insurance Agency of the Ministry of Health and
Welfare, the number of scanners in Taiwan had
increased to 226 by the second half of 2017, with
approximately 9.58 scanners per million people,
which is between Slovakia (9 scanners per million
people) and Canada (10 scanners per million people)
(National Health Insurance Administration Ministry
of Health and Welfare, 2018a, The Organisation for
Economic Co-operation and Development, 2017).
Although the number of MRI scanners has
increased yearly, the waiting time for the examination
is still too long. According to the standards in Ontario,
Canada, patients with preferential treatment
classifications P1 and P2 are very urgent outpatients,
inpatients, and Emergency Department (ED) patients
Lee, L., Ou, Y., Cheng, Y., Sun, Y., Wu, H. and Guo, W.
Using a Hybrid Simulation Model to Maximize Patient Throughput of Magnetic Resonance Imaging in a Medical Center.
DOI: 10.5220/0007932003090316
In Proceedings of the 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications (SIMULTECH 2019), pages 309-316
ISBN: 978-989-758-381-0
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
309

who should be examined immediately or within 48
hours; the classification P3 denotes emergency
outpatients who should be examined in 2 to 10 days;
and the classification of P4 denotes general
outpatients. The waiting time for MRI examinations
should not exceed 28 days. However, the average
MRI waiting time for adult outpatients is 59 days
(Health Quality Ontario, 2018). The waiting time in
Manitoba, Canada, is approximately 68 workdays
(Province of Manitoba, 2018). Taiwan currently has
no similar statistics for the waiting time for MRI
examination. However, the waiting time for MRI
examination is still recognized as long.
In the health care management field, to understand
the effects of new policies and new technology
introductions, organizations may need to analyze
relevant economic roles (e.g., competitors and
suppliers), responses from users, and environmental
impact. However, exploring the effectiveness of a
new strategy by traditional techniques has its
limitations. Most of the traditional techniques can
only analyze data theoretically or qualitatively. Even
some new strategies require actual or trial investment
in human and material resources so that managers can
understand the impact and determine whether a
strategy deserves continued investment. To avoid the
losses caused by failure after investment, many
simulation analyses have been applied to ED research
since 1999 (Hurwitz et al., 2014, Saoud et al., 2016).
Additionally, a small number of studies have been
applied to rehabilitation (New et al., 2015),
orthopedics (Rohleder et al., 2011), surgery (Sobolev
et al., 2011), hospitalization (Hahn-Goldberg et al.,
2014), ophthalmology and radiology (Lindsköld et
al., 2012, Viana, 2014). All these studies show that a
good simulation model is adaptable (Paranjape, 2009)
and can be adapted to practice changes as an aid to
the evaluation decision before the new strategy is
adopted.
A patient’s waiting time for an examination in a
radiology department includes the duration from
when a radiology request is made in the clinic, the
radiology department receives the request, the
radiology department vets the request, the radiology
department schedules the examination, to when the
patient attends, waits and completes the examination
(Olisemeke et al., 2014). Retrospective to 1987, a
study simulated the daily non-admission patients
through the radiology department of a large acute care
hospital. This study showed that the addition of one
more radiologist would lead to a reduction in the
length of stay of non-admission patients (Klafehn,
1987).
Later studies focused on radiology department
services, such as mammography (Coelli et al., 2007),
sonography (Johnston et al., 2009), computed
tomography (CT) (Ramakrishnan et al., 2004, van
Lent et al., 2012), and X-ray (Oh et al., 2011,
Lindsköld et al., 2012),. The examination process has
been simulated to explore the relevant key
performance indicators (KPIs) before and after the
improvement plan. These studies assessed the number
of patients examined within one hour, the time of
completing image reports, the time of the patient
waits for the examination, the length of time the
patient stays in the department, and the utilization rate
of the radiologist as effective indicators as to assist in
the formulation and implementation of preplanning
decisions (Ramakrishnan et al., 2004, Coelli et Al.,
2007, Johnston et al., 2009, Oh et al., 2011). The MRI
examination workflow and KPIs are different in
different organizations and units. Additionally, an
MRI scanner cannot provide all examination services.
It depends on if the needed coil types are adopted by
the scanner or not. However, a review of past studies
in radiology, mostly using discrete event simulation
as the main analytical method, the characteristic of
patient, staff, and scanner were lack to control and
define in a simulated workflow. The KPIs of the
individual patient, scanner and the department could
not be accurately estimated.
Hence, the purpose of the study was to propose a
new strategy to maximize patients throughput so that
the waiting time of a patient to undergo a magnetic
MRI examination can be shortened as well as the
utilization rates of MRI scanners can be increased.
The specific aims in this study are (a) to develop a
discrete event (DES) and agent-based simulations
(ABS) model to simulate the MRI examination
workflow at an MRI department in a medical center
of Taiwan, and (b) to identify which time frames of
day have fewer patients examined, to experiment with
the proposed strategy by hiring radiographers in those
time periods in the simulation model, and then to
explore the changes in KPIs, including the daily MRI
scanner utilization rate, monthly gross income, and
waiting time to undergo an MRI examination.
2 RADIOLOGY DEPARTMENT
SETTING
2.1 MRI Examination Services
The research setting was the MRI department, under
the radiology department, of Taipei Veterans General
Hospital (TVGH), which is a 2,735-bed medical
center in northern Taiwan. This department provides
MRI examination services for ED patients, inpatients,
and outpatients. The MRI examination service runs
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
310
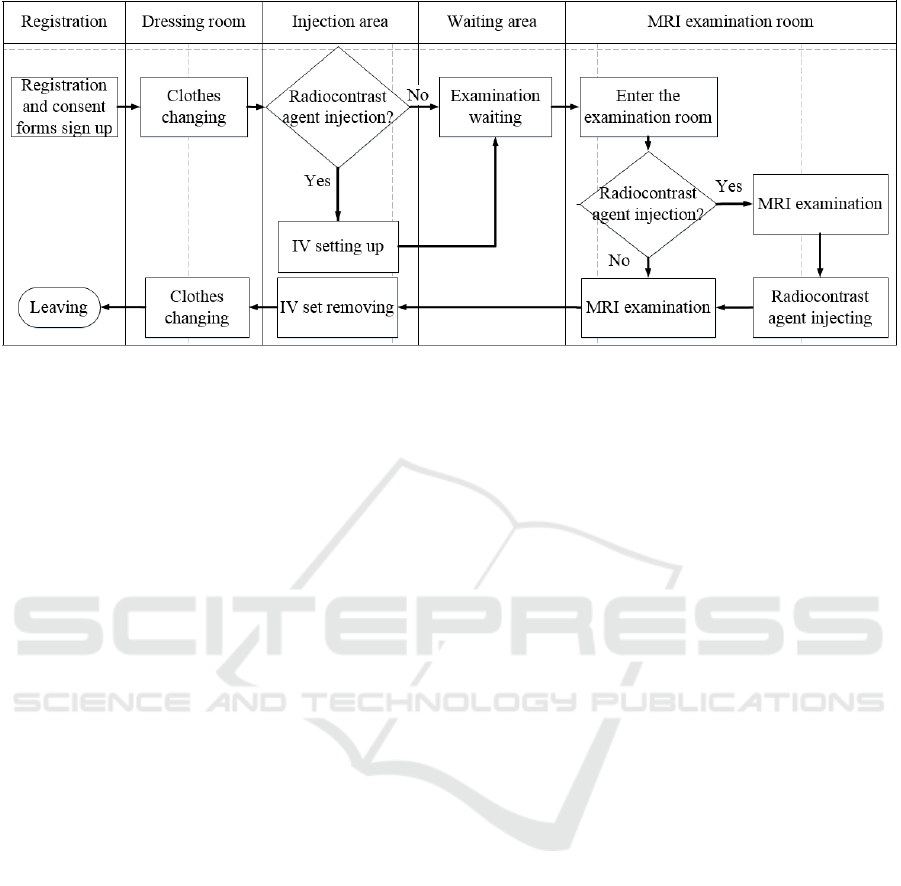
Figure 1: The patient flow of MRI examination.
from 7:30 to 23:00 on workdays and from 8:00 to 23:00
on weekends. The shifts are different for four types of
human resources, including administrators, nurses,
radiographers, and medical resident. The administrator
and nurse only work the day shift from 8:00 to 17:30.
Nevertheless, radiographers need work in either the
day shift from 7:00 to 15:00 or the night shift from
15:00 to 23:00. Medical residents work shifts
depending on the departmental regulations, but they
are available to support the MRI examination services
from 7:00 or 8:00 to 23:00, depending on the day.
The duties of each worker are as follows:
An administrator is responsible for examination
date and time scheduling, registration affairs and
explanation of related matters for patients.
Nurses are responsible for intravenous (IV)
injection and assisting the administrator.
Radiographers are responsible for MRI scanner
operation and MRI examination execution.
Medical residents are responsible for
radiocontrast agent injection and the tasks of
nurses when nurses are off work, i.e., before 8:00
and after 17:30.
The fixed resources of the MRI department
include one 3.0 Tesla (3.0-T) MRI scanner (Scanner
A) and four 1.5 Tesla (1.5-T) MRI scanners (Scanner
B to E). The former is for a specific examination.
Patients will be assigned to the scanner after check-in
if they schedule the 3.0-T MRI service. The latter is
for general examinations. Patients will be randomly
assigned to one of four available scanners after check-
in if they schedule for a 1.5-T MRI examination.
In the MRI department, an average of 91 patients
(92 and 89 patients on weekdays and weekends,
respectively) are examined a day, i.e., 18 patients for
each scanner. However, the need for MRI
examination service exceeds the supply. When an ED
patient, inpatient, or outpatient needs an MRI
examination service, he or she must wait to be
examined for five hours, three days, or 30 days,
respectively. The utilization rate of our five scanners
ranges from 55% to 73%. Therefore, how to reduce
the idle condition of the scanner and to increase the
number of served patients each day warrants attention.
2.2 MRI Examination Flow
Figure 1 is the patient flow of MRI examination in the
TVGH. First, patients have to check in at the
registration counter and sign the consent form for MRI
examinations. Then, patients walk to the dressing room
to change into loose-fitting hospital clothes. If patients
need a radiocontrast agent injected, the nurse will then
perform the set up for intravenous placement. All
patients will wait in the waiting area until the
radiographer calls their names to enter the MRI
examination room. Then, the patients will be examined
without radiocontrast agent injection or examined
before and after radiocontrast agent injection by
medical residents. The examined patients with an IV
set will have the IV set removed. All patients will
change back into their clothes before leaving.
3 MODEL DEVELOPMENT AND
EVALUATION
3.1 Simulation Framework
The simulation framework applies DES and ABS
(Hamrock et al., 2013, Viana et al., 2018). The DES is
used for MRI examination flow, the MRI scanners, and
staffs. The ABS is applied when the patient with the
Using a Hybrid Simulation Model to Maximize Patient Throughput of Magnetic Resonance Imaging in a Medical Center
311
different need of MRI coil types interact with each
other by competing for MRI scanners. The patients
have been modeled as agents to allow future
development and provide a base for future expansion
of the model.
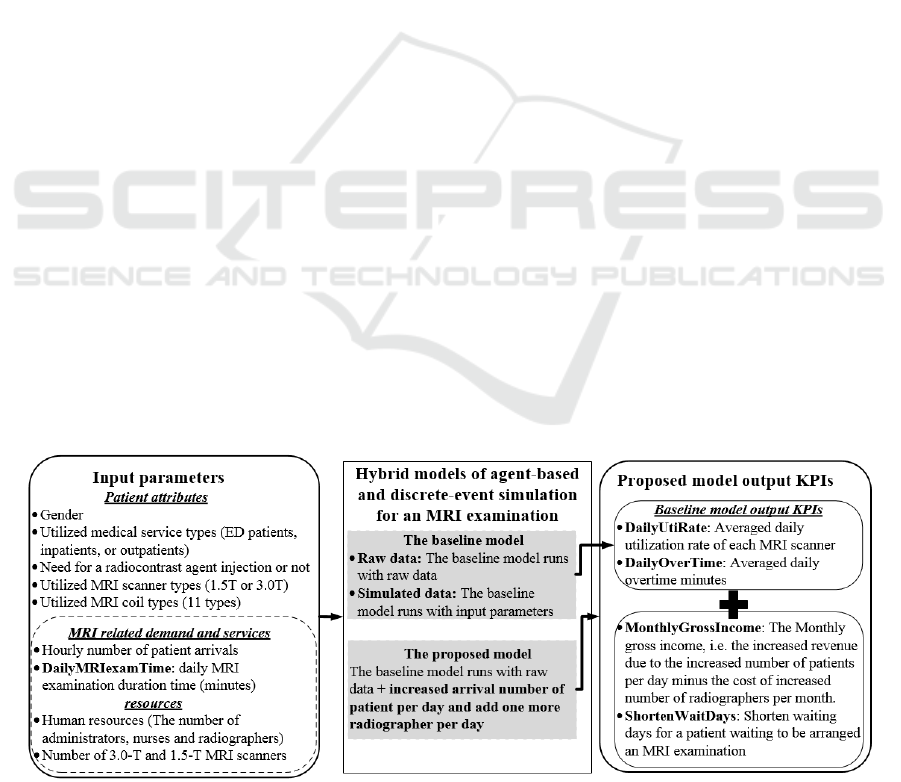
As shown in Figure 2, there are two types of input
parameters. One parameter is the patient attributes, and
the other parameter is MRI examinations-related
demand, services and resources. The former includes
patients’ gender, the utilized medical service types (ED
patients, inpatient, or outpatients), need for a
radiocontrast agent injection or not, utilized MRI
scanner type (3.0-T or 1.5-T), and utilized MRI coil
type (11 types). The latter includes an hourly number
of patient arrivals, daily MRI examination duration
time in minutes (DailyMRIexamTime), human
resources (one administrator, one nurse, and ten
radiographers), and one 3.0-T and four 1.5-T MRI
scanners. For DailyMRIexamTime, if a patient needs
radiocontrast agent injection, DailyMRIexamTime
will encompass the injection of the radiocontrast agent
as well as the coil and scanner preparation and the MRI
examination execution. Otherwise, the
DailyMRIexamTime includes only time in the coil and
scanner preparation, and examination execution.
Output parameters are composed of four KPIs,
which are the average daily utilization rates of each
MRI scanner (DailyUtiRate, i.e., each MRI scanner’s
examination duration time per day divided by 16
hours), average daily overtime minutes
(DailyOverTime), the monthly gross income
(MonthlyGrossIncome, i.e., the increased revenue
due to the increased number of patients minus the cost
of the increased number of radiographers per month),
and the shortened waiting time (ShortenWaitDays)
for a patient who originally would have to wait for 30
days, i.e., an outpatient’ waiting days for an MRI
examination in the TVGH, to be underwent an MRI
examination.
The study first built a baseline model to simulate
the current MRI examination workflow in the MRI
department in the TVGH. To validate if the model with
simulated data is the same as the model with raw data,
the Wilcoxon rank-sum test was used for comparing
three input parameters and two output KPIs. The
former includes a daily number of patient arrivals
(DailyNumPatients), the number of patients utilizing
the three medical service types
(DailyNumServiceTypes) and DailyMRIexamTime.
The later includes DailyUtiRate and DailyOverTime.
After confirmation that the baseline model with
simulated data has a statistically nonsignificant
difference from the baseline model with raw data, we
conduct experiments to build the proposed model
based on the baseline model with simulated data. The
proposed model is developed by adding numbers of
patients and staffs per day to find an optimal
DailyUtiRate with statistically nonsignificant
DailyOverTime. Additionally, we not only validate
that DailyOverTime has a statistically nonsignificant
difference from the baseline model with simulated data,
but also confirm that DailyUtiRate,
MonthlyGrossIncome, and ShortenWaitDays are
positive results in the proposed model.
3.2 Material and Data Preprocessing
The 2,814 MRI examination logs with de-
identification of patients and radiographers in
December of 2016 are collected from the MRI
department. One log that belonged to the MRI
examination in November is excluded. All data fields
include patients’ gender, utilized medical service
types, need for a radiocontrast agent injection or not,
utilized MRI scanner (labeled A to E), the received
MRI examination name (96 classifications), and
Figure 2: Simulation framework of MRI examinations workflow.
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
312

DateTime of getting on and off the MRI examination
table. Other information, such as workflow, business
hours, human resources allocation, the number and
location of 3.0-T and 1.5-T scanners are informed by
authors Sun, Wu, and Guo according to their work
experience. This study was approved by the Taipei
Veterans General Hospital Institutional Review
Board in December 2018 (2018-01-010CC).
To generate input parameters and output KPIs,
data preprocessing was conducted. To produce an
hourly number of patient arrivals on each day, the
study presumed that arrival time was 40 minutes
before the DateTime of patients getting on the MRI
examination table. Additionally, the utilized MRI
scanners are converted into two types of MRI scanner
types (scanner A is 3.0-T, while scanners B to E are
1.5-T). Distinct 96 MRI examination names are
converted into 11 coil types. DailyMRIexamTime
equals to the DateTime of getting off minus getting
on the MRI examination table. DailyOverTime equals
to the DateTime of getting off the MRI examination
table minus 23:00.
3.3 Input Parameters
Regarding the patient attributes in the simulation
models, 49.6% of patients were male, according to the
raw data. The percentage of ED patients, inpatients,
and outpatients are 5.6%, 19.1%, and 75.3%,
respectively. Some 57.96% of all patients need
radiocontrast agent injection for the MRI examination.
The MRI scanner A (3.0-T) is pre-arranged for 13%
of all patients, while MRI scanners B to E (1.5-T) are
pre-arranged for 87% of all patients. The eleven types
of MRI examination coil have different utilization
rate, i.e., standard head (1.07%), torso (16.71%),
shoulder (1.78%), 8-inch head (51.21%), low
extremity (0.07%), neck (6.83%), torso head flexible
(2.67%), breast (0.71%), spine (14.05%), cardiac
(1.03%), and knee (3.88%).
The MRI examination service applies the first in,
first out (FIFO) method. For each patient to be
examined, the MRI scanner B, C, D, or E is arranged
according to what coil type the patient needs. Each
scanner’s monthly examination service volume in
different coil types from high to low decides the
scanner’s priority for the patient. For example, if the
patient needs coil type “cardiac” and scanners’
service volume for using the cardiac coil from high to
low are scanners D, B, C, and E, the patient will be
arranged to the available MRI scanner D, B, C, or E,
accordingly.
For the MRI examinations-related demand, an
hourly number of patient arrivals (Table 1) is
calculated using the MRI examination records of
December 2016. The DailyMRIexamTime for each
scanner is used to generate a custom distribution.
Additionally, the study adopts the thumb rule by
using the triangular distribution (setting minimum,
maximum and mode in minutes) for configurations of
the time registration service (1,3,5), clothes changing
1,3,2), IV setting up (1,4,3), and IV set removing
(1,3,2).
3.4 Output Key Performance
Indicators (KPIs)
As mentioned above, MonthlyGrossIncome is
estimated by the increased monthly revenue minus
increased monthly cost of the proposed solution. The
increased monthly revenue equals the increased
number of patients multiplied by the points of the
hospital global budget payment (pts) for providing
each MRI examination to a patient without
radiocontrast (6,500 pts) or with radiocontrast agent
injection (11,500 pts) (Ministry of Health and
Welfare, 2017). The monetary value of points was
converted at a 0.8265 ratio and a rate of 30 Taiwanese
dollars to one US dollar (National Health Insurance
Committee Ministry of Health and Welfare, 2018).
The increased monthly cost equals the increased
number of radiographers multiplied by US$1,546,
which is a market salary for a radiographer with a
postgraduate degree.
3.5 The Proposed MRI Examination
Model
Based on the baseline model, the study experiments
with seven configurations by gradually adding even
numbers of patients (i.e., 2, 4, 6, up to 14 patients) a
day to the proposed model. We chose even numbers
of patients because fewer patients were examined at
two-time slots (i.e., 11:00, during lunch, and 17:00,
during dinner) each day. To satisfy the examination
needs of patients, the proposed model is designed by
hiring one additional radiographer from 11:00 to
19:00 per month to provide service to these added
patients.
Table 1: Number of patient arrivals per hour.
Time
6:00
7:00
8:00
9:00
10:00
11:00
12:00
13:00
14:00
15:00
16:00
17:00
18:00
19:00
20:00
21:00
22:00
Number
of patients
3
6
6
6
6
4
6
6
7
6
6
4
6
6
7
5
1
Using a Hybrid Simulation Model to Maximize Patient Throughput of Magnetic Resonance Imaging in a Medical Center
313
3.6 The Proposed Model Validation
and Analysis Tool
The simulated dates for the baseline and proposed
models are from 1 December 2016 to 1 January 2017.
According to the simulation framework (in section
3.1), the study tests the baseline model and the
proposed model with simulated data to confirm that
both have nonsignificant differences in
DailyOverTime. The statistical test method used is
the Wilcoxon rank sum test. The study used flow
charts for workflow analysis, AnyLogic for
simulation model development, Excel for exported
logs of AnyLogic, and SAS for statistical analysis.
4 SIMULATION RESULTS
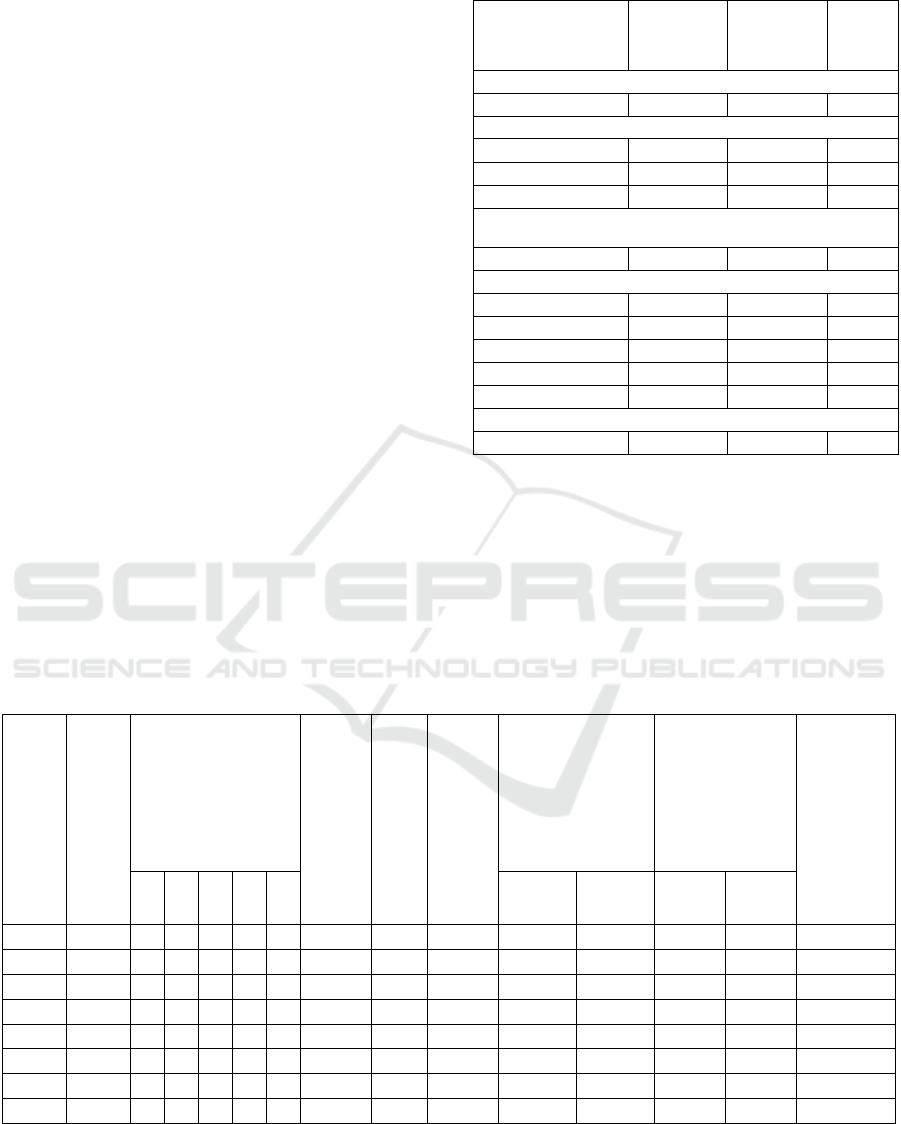
As shown in Table 2, the baseline model with raw
data and simulated data have nonsignificant
differences in DailyNumPatients,
DailyNumServiceTypes, DailyMRIexamTime,
DailyUtiRate, and DailyOverTime. In the raw and
simulated data, DailyNumPatients are 2,813 and
2,821 patients, respectively. DailyNumServiceType,
including ED patient, inpatient, and outpatient, are
5.62, 19.09, and 75.29%, respectively, in the raw data
and 5.28, 19.00, and 75.72%, respectively, in the
simulated data DailyMRIexamTime is 35.78 and
36.10 minutes, respectively.
Table 2: The validation of the baseline model.
Statistical parameters
Baseline
model with
raw data
Baseline
model with
simulated
data
p-value
DailyNumPatients: n
2,813
2,821
0.6384
DailyNumServiceTypes: n (%)
ED patients
158(05.62)
149(05.28)
0.7916
Inpatients
537(19.09)
536(19.00)
0.8433
Outpatients
2,118 (75.29)
2,136(75.72)
0.8820
DailyMRIexamTime: mean in minutes (standard
deviation)
35.78(1.98)
36.10(1.38)
0.5685
DailyUtiRate: (%)
MRI scanner A
55.10
50.41
0.1570
MRI scanner B
74.20
76.19
0.7514
MRI scanner C
74.39
75.50
0.3638
MRI scanner D
74.85
74.52
0.2050
MRI scanner E
73.35
76.22
0.3107
DailyOverTime: median in minutes (standard deviation)
0(42.13)
0(10.35)
0.9300
DailyUtiRate for each scanner from A to E is 55.10,
74.20, 74.39, 74.85, and 73.35%, respectively, in the
raw data and 50.41, 76.19, 75.50, 74.52, and 76.22%,
respectively, in the simulated data. DailyOverTime is
0 in both models.
As shown in Table 3, when the number of daily
patients is increased to greater than or equal to eight
patients, at least one scanner’s DailyUtiRate can
Table 3: One-month simulation in the proposed model.
Note:
†
without contrast: number of monthly patients multiplied by points of the hospital global budget payment (pts) for
providing each MRI examination to a patient without radiocontrast agent injection (6,500 pts);
‡
with contrast: number of
monthly patients multiplied by points of the hospital global budget payment (pts) for providing each MRI examination to a
patient with radiocontrast agent injection (11,500 pts).
Experi-
ments
:Added
No. of
patient
arrivals
per day
Total
No. of
patients
in the
month
Utilization rate
of the MRI scanner
(daily) (%, used
hours/16 hours)
Average
daily
overtime
minutes
Added
No. of
radio-
grapher
per
month
①
Increased
staff cost
(US$)
per
month
②
Increased point of
hospital global
budget payment
(pts) per month
(31 days)
③
Increased
gross income per
month (31 days)
【② x 0.8265
x 0.03US-①】
Shortened
days of
patient
waiting to
schedule an
MRI
examination
(1 working
day=16
hours)
A
B
C
D
E
without
contrast
†
with
contrast
‡
without
contrast
with
contrast
Baseline
2,821
50
76
75
74
76
6
-
-
-
-
-
-
-
+2
2,883
44
78
78
79
78
5
1
1,546
403,000
713,000
8,446
16,133
11H
+4
2,945
50
79
78
79
79
8
1
1,546
806,000
1,426,000
18,439
33,812
1D & 5H
+6
3,007
52
80
81
80
80
11
1
1,546
1,209,000
2,139,000
28,431
51,491
1D & 15H
+8
3,069
53
81
83
83
81
15
1
1,546
1,612,000
2,852,000
38,424
69,169
2D & 8H
+10
3,131
60
82
82
83
83
22
1
1,546
2,015,000
3,565,000
48,416
86,848
3D & 1H
+12
3,193
50
85
87
86
85
22
1
1,546
2,418,000
4,278,000
58,408
104,527
3D & 10H
+14
3,255
56
87
86
88
87
28
1
1,546
2,821,000
4,991,000
68,401
122,206
4D & 2H
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
314

reach more than 83%. However, only when the
proposed model adding eight patients a day has a
statistically nonsignificant difference in
DailyOverTime (median=0 minute) compared to the
raw data (p=.3257). The other experiments increase
DailyOverTime.
To hire one additional radiographer will increase
the cost by US$1,546 per month. The increased
monthly hospital global budget payment points
(income) due to MRI examination without and with
radiocontrast agent injection are 1,612,000 and
2,852,000 points, respectively. As a result,
MonthlyGrossIncome will be between US$38,242
and US$69,169. For a patient who originally has to
wait for 30 days to be arranged an MRI examination,
under this situation, the patient can be examined two
days and eight hours sooner.
5 DISCUSSION AND
CONCLUSION
Here, we report preliminary research on the
maximization of MRI examination patient throughput.
A major finding is that to hire one additional
radiographer for MRI examination in the TVGH
would increase the serviced volume by 248 patients a
month (31 days). This proposed solution would
increase the utilization rate of scanners, raise the
monthly gross income, and shorten the waiting time
for patients who need the MRI examination service.
Except for scanner A, the other scanners have a
relatively high utilization rate. This observation is
because scanner A is also used for research purposes.
Compared to the discrete event-based simulation, the
hybrid method can not only simulate the MRI
examination workflow but also include
characteristics of patients, staffs, and scanners. This
characteristic makes the simulation model easy to
adjust to service logic according to the agent
characteristics, e.g., the utilized coil type, and lead to
a nonsignificant difference from the reality.
This is also the first study in Taiwan to use
simulation analysis methods to analyze and improve
the evaluation of the current situation of the MRI
department. In addition to proposing different
opinions on improving the evaluation of the program
from the traditional improvement methods, this
simulation also assists the managers of the MRI
department in evaluating the feasibility of the
improvement program in practice and provides
different decision-making aids for managers as a
reference.
Despite the hybrid simulation model’s
advantages, it does have four limitations. First, the
time stamps of patient registration, clothes changing,
IV setting up and IV set removal cannot be obtained.
We calculate these timestamps according to the
thumb rule. Moreover, the DateTime of getting on
and off the MRI examination table were manually
entered into an information system by radiographers.
The accuracy of our data is unknown, although the
simulated model is well developed. Third, the
simulation model is based on the data during
December 2016. The variances due to seasonal
reasons are not accounted for in the study. Fourth, the
simulated model cannot be generalized to other fields.
However, the study design and simulation method,
including the parameters, can be a reference for
related workflows, e.g., CT examinations.
This maximization of MRI examination patient
throughput is still in the experimental stage, and much
more work has yet to be conducted. Much more also
needs to be known about how to pre-arrange patients
with different coil-type needs and how to properly
assign on-site patients to busy scanners. This study
should provide a simulation basis for additional
research. There is a continuing need for an adequate
solution with big-data simulations for the practical
application of MRI examination management with a
high utilization rate of scanners and less waiting time
for undergoing an examination.
ACKNOWLEDGMENTS
This study is supported by the Taiwan Ministry of
Science and Technology under grant number MOST
107-2221-E-227-002-.
REFERENCES
Coelli, F. C., Ferreira, R. B., Almeida, R. M. V. & Pereira,
W. C. A. 2007. Computer simulation and discrete-event
models in the analysis of a mammography clinic patient
flow. Computer methods and programs in biomedicine,
87, 201-207.
Global Views 2015. The investigation of physical
examination center in Taiwan.
Hahn-Goldberg, S., Chow, E., Appel, E., Ko, F., Tan, P.,
Gavin, M., Ng, T., Abrams, H., Casaubon, L. & Carter,
M. 2014. Discrete event simulation of patient
admissions to a neurovascular unit. Journal of
healthcare engineering, 5, 347-360.
Hamrock, E., Paige, K., Parks, J., Scheulen, J. & Levin, S.
2013. Discrete event simulation for healthcare
organizations: a tool for decision making. Journal of
Healthcare Management, 58, 110-124.
Health Quality Ontario. 2018. WAIT TIMES FOR
DIAGNOSTIC IMAGING [Online]. Available:
https://www.hqontario.ca/System-Performance/Wait-
Using a Hybrid Simulation Model to Maximize Patient Throughput of Magnetic Resonance Imaging in a Medical Center
315

Times-for-Diagnostic-Imaging?ScanType=AdultMRI
[Accessed].
Hurwitz, J. E., Lee, J. A., Lopiano, K. K., Mckinley, S. A.,
Keesling, J. & Tyndall, J. A. 2014. A flexible
simulation platform to quantify and manage emergency
department crowding. BMC medical informatics and
decision making, 14, 50.
Johnston, M., Samaranayake, P., Dadich, A. & Fitzgerald,
J. Modelling radiology department operation using
discrete event simulation. MODSIM, International
Congress on Modelling and Simulation, Cairns, 2009.
678-84.
Klafehn, K. A. Impact points in patient flows through a
radiology department provided through simulation.
Proceedings of the 19th conference on Winter
simulation, 1987. ACM, 914-918.
Lindsköld, L., Wintell, M., Aspelin, P. & Lundberg, N.
2012. Simulation of radiology workflow and
throughput. Radiology management, 34.
Ministry of Health and Welfare. 2017. What is the meaning
of points in Annual Report? [Online]. Available:
https://dep.mohw.gov.tw/DOS/cp-1716-14931-
113.html [Accessed].
National Health Insurance Administration Ministry of
Health and Welfare. 2018a. The amount, brand, type,
date of manufacture, date of purchase and service life
of MRI sanner in Taiwan. [Online]. Available:
https://data.gov.tw/dataset/22238 [Accessed].
National Health Insurance Administration Ministry of
Health and Welfare. 2018b. The physical examination
popularizing rate of age 40-64 adult in Taiwan.
[Online]. Available: https://data.gov.tw/dataset/21274
[Accessed].
National Health Insurance Committee Ministry of Health
and Welfare. 2018. The total payment of national health
insurance medical consultation fee reference index
[Online]. Available: https://dep.mohw.gov.tw/NHIC/
lp-1665-116.html [Accessed].
New, P. W., Racp, F., Stockman, K., Cameron, P. A., Olver,
J. H. & Stoelwinder, J. U. 2015. Computer simulation
of improvements in hospital length of stay for
rehabilitation patients. Journal of rehabilitation
medicine, 47, 403-411.
Oh, H. C., Toh, H. G. & Giap Cheong, E. S. 2011.
Realization of process improvement at a diagnostic
radiology department with aid of simulation modeling.
Journal for Healthcare Quality, 33, 40-47.
Olisemeke, B., Chen, Y., Hemming, K. & Girling, A. 2014.
The effectiveness of service delivery initiatives at
improving patients’ waiting times in clinical radiology
departments: a systematic review. Journal of digital
imaging, 27, 751-778.
Paranjape, R. 2009. Multi-Agent Systems for Healthcare
Simulation and Modeling: Applications for System
Improvement: Applications for System Improvement,
IGI Global.
Province of Manitoba 2018. Health Services Wait Time
Information.
Ramakrishnan, S., Nagarkar, K., Degennaro, M., Srihari,
K., Courtney, A. K. & Emick, F. A study of the CT scan
area of a healthcare provider. Proceedings of the 36th
conference on Winter simulation, 2004. Winter
Simulation Conference, 2025-2031.
Rohleder, T. R., Lewkonia, P., Bischak, D. P., Duffy, P. &
Hendijani, R. 2011. Using simulation modeling to
improve patient flow at an outpatient orthopedic clinic.
Health care management science, 14, 135-145.
Saoud, M. S., Boubetra, A. & Attia, S. 2016. A Simulation
Knowledge Extraction-based Decision Support System
for the Healthcare Emergency Department.
International Journal of Healthcare Information
Systems and Informatics (IJHISI), 11, 19-37.
Sobolev, B. G., Sanchez, V. & Vasilakis, C. 2011.
Systematic review of the use of computer simulation
modeling of patient flow in surgical care. Journal of
medical systems, 35, 1-16.
The Organisation for Economic Co-Operation and
Development. 2017. Magnetic resonance imaging
(MRI) units [Online]. Available:
https://data.oecd.org/healtheqt/magnetic-resonance-
imaging-mri-units.htm [Accessed].
Van Lent, W. A., Deetman, J. W., Teertstra, H. J., Muller,
S. H., Hans, E. W. & Van Harten, W. H. 2012.
Reducing the throughput time of the diagnostic track
involving CT scanning with computer simulation.
European journal of radiology, 81, 3131-3140.
Viana, J. Reflections on two approaches to hybrid
simulation in healthcare. Simulation Conference
(WSC), 2014 Winter, 2014. IEEE, 1585-1596.
Viana, J., Simonsen, T. B., Dahl, F. A., & Flo, K. A hybrid
discrete event agent based overdue preganancy
outpatient clinical simulation model. Simulation
Conference (WSC), 20118 Winter, 2018. IEEE, 1488-
1499.
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
316
