
How to Applicate Comprehensive Geriatric Assessment
in Geriatric Rehabilitation
Wanarani Aries
Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo General Hospital,
Faculty of Medicine, University of Indonesia, Jakarta, Indonesia
kolit.rehabmedikrscm@gmail.com
Keywords: CGA, Geriatric Patients, Functional Status, Interdiscpline Approach
Abstract: Comprehensive Geriatric Assessment (CGA) is a multidimensional, multidisciplinary diagnostic instrument
designed to collect data on the medical, psychosocial-economy, enviromental, spiritual and places high
value on functional status. Measurement of functional is an essential components, and the patient’s ability to
function can be viewed as a summary measure of the overall impact of elderly health conditions. This
geriatric models of assessment used in patient first visit to assess geriatric patients who have complicated
condition and need special approach. CGA has several essential aspects of evaluating elderly patients, so it
is known for it’s costly and time consuming. This caused by difficulties in taking histories of geriatric
patients, and systematically reviewing the patients. CGA aimed to integrates the functional and medical
goals of care, allowing physicians to improve clinical outcomes and patients satisfaction. This tools can be
used in primary care (e.g puskesmas), clinic, hospital, long term care or home, and as a strategy to make
evaluation process more efficient. Prognosis is focused on medical and function information. CGA can be
applied in 4 step process, used by individual clinician but more refers to an interdisciplinary team.
1 INTRODUCTION
The population of elderly, or defined by aged 60
years old or older is increasing along with the life
expectancy. Between 2015 and 2050, the proportion
of the world's population over 60 years will nearly
double from 12% to 22%. In 2050, 80% of older
people will be living in low and middle income
countries, and the pace of population ageing is much
faster than in the past (World Health Organization,
2018). In Indonesia, the number of elderly is
increasing, from 18 million people (7.56%) in 2010
to 25.9 million people (9.7%) in 2019, and expected
to continue increasing in 2035 to 48.2 million people
(15.77%) (Kementerian Kesehatan RI, 2019). This
condition cause a face major challenges to ensure
their well-being in comprehensive aspect.
Ageing is the natural process of life, results from
the impact of the accumulation of a wide variety of
molecular and cellular damage over time. Later, it
leads to a gradual decrease in physical and mental
capacity, a growing risk of disease, and ultimately,
death. This gradual decrease could potentially
increasing disability that occur over the course of
time in health. Disability can have a negative impact
on mobility, self-care, and pain. This condition
requires the role of rehabilitation, aimed to focus on
recovery of self-care ability, mobility, and its
requires a longer period of time to achieve.
2 DISCUSSION
2.1 Comprehensive Geriatric
Assessment (CGA)
Based on complicated condition generally described
above, the elderly need special approach and the
CGA is a multidimensional, multidisciplinary
diagnostic instrument designed to collect data on the
medical, psychosocial-economy, enviromental,
spiritual and places high value on functional status.
This tool has several essential aspects of evaluating
geriatric patient, so its consist of several instrument.
CGA assess patient’s functional status, using ICF
(International Classification of Functioning,
Disability and Health), which can be viewed as a
48
Aries, W.
How to Applicate Comprehensive Geriatric Assessment in Geriatric Rehabilitation.
DOI: 10.5220/0009062100480053
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 48-53
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

summary measure of the overall impact of elderly
health conditions.
This assesment aimed to integrates the functional
and medical goals of care, allowing physicians to
improve clinical outcomes and patients satisfaction,
and as a strategy to make evaluation process more
efficient. CGA can be used at patient first visit in
primary care (e.g puskesmas), clinic, hospital, long
term care, or home, done in 4 step process by
individual clinician but more refers to an
interdisciplinary team. Because of its comprehensive
method, systematically reviewing the patients, and
difficulties in taking histories of geriatric patients, it
is known for it’s costly and time consuming. The
prognosis of this assesment focused on medical and
function information.
2.2 Review of CGA
Aging, is an inevitable and extremely complex,
multifactorial process, is characterized by the
progressive degeneration of organ systems and
tissues. It is largely determined by genetics, and
influenced by a wide range of environmental factors,
such as diet, exercise, exposure to microorganisms,
pollutants, and radiation. Gender also plays a part
and, in most developed countries, women typically
outlive men by 7–10 years. Recent research has also
reported that childhood personality and education, as
well as behavioral factors, also contribute to
longevity (Nigam et al, 2012).
Based on management model for service delivery,
elderly can be stratified into one of three strata:
robust; frail; and complex care needs. Spoorenberg
et al, 2013). Frailty is a geriatric syndrome
characterized by impaired performance and reduced
functional reserve across multiple physiologic
systems, and associated with increase vulnerability
adverse health outcomes from even minor stressor
(Sloane and Cesari, 2018). Frailty often overlapping
with sarcopenia, which is a term of the loss of
muscle function as well as the loss of muscle mass
that occurs with ageing. It is a common and
increasingly condition associated with subsequent
disability and morbidity (Dodds and Sayer, 2016).
The utilization of CGA can be used in the three
groups above, especially for screening in elderly, so
frailty can be prevented or reversed. By reversing
frailty through exercise intervention, elderly patients
can be remain physically independent and non-frail
throughout a longer period of their life (Pilotto,
2018).
2.3 Geriatric Health Problem
Multiple pathology process occur in elderly and play
important role in declining physical function. It is
clear that the loss in physical function is inevitable
in elderly, but the effects of age are highly
individual and age alone is a poor index of physical
function. Age is associated with increased
prevalence of disease conditions that are impossible
to ignore as a strong contributor to occurrence of
disability (Manini, 2011). Measurement of disability
are able to capture the impact of the presence and
severity of multiple pathologies, including physical,
cognitive, and psychological conditions, as well as
the potential synergistic effects of these conditions
on overall health status (Halter et al, 2017).
Balance and gait are important considerations in
the health of elderly subjects. Decline of sensory
systems in elderly adults has been implicated in the
reduced ability of older adults to adapt to changes in
their environment and maintain balance; the visual
system is particularly important in maintaining
postural stability. It is estimated that 13% of adults
self‐report imbalance from ages 65 to 69 and this
proportion increases to 46% in those aged 85 and
older. Furthermore, impairments of balance and gait
have been implicated in increased risks of falls. In
adults aged 65 and older, the estimated annual
prevalence of falls is 28% (Nigam et al, 2012). Falls
are associated with significant morbidity and
mortality in the elderly because they are the most
common cause of accidental death and nonfatal
accidental injury, accounting for 55.8% of accidental
deaths in those 65 and older (Osoba et al. 2019).
2.4 Comprehensive Management In
Geriatric Health Problem
The elderly population constitutes a significant
challenge for health authorities worldwide as with
advancing age multiple chronic diseases are
associated. As a result of which elderly people tend
to take multiple medications in a day that can be
referred to as polypharmacy. Elderly people are at a
greater risk for adverse drug reactions (ADRs)
because of the metabolic changes and reduced drug
clearance associated with ageing; this risk is
furthermore exacerbated by increasing the number
of drugs used. Polypharmacy may also lead to
decreased medication compliance, poor quality of
life, and unnecessary drug expenses (Dagli and
Sharma, 2014).
How to Applicate Comprehensive Geriatric Assessment in Geriatric Rehabilitation
49

As we know before, old age often goes hand in
hand with increasingly complex and often
interrelated problems, they need social support.
Social support has been recognized as an important
social determinant of health because it assists
individuals in reaching their physical and emotional
needs, and it reduces the effects of stressful events
on their quality of life
.
Social support consists of
addressing tangible needs, such as assistance with
transportation, home and personal care, as well as
emotional support such as being listened to,
understood, and comforted. This support can be done
either by family, neighbor, or other people as their
caregiver (Dai et al, 2016).
Caregivers assist the daily care needs of the care
receiver using activities of daily living (ADLs) and
instrumental activities of daily living (IADLs)
scoring. Caregiver as an individual who provides
direct care to children, elderly people, or the
chronically ill. Stress is defined as “a physical,
chemical, or emotional factor that causes bodily or
mental tension and may be a factor in disease
causation. Caregiver divided by two groups, consist
of formal and informal. Formal caregivers are
volunteers or paid employees connected to the social
service or healthcare systems. The term informal
caregiver refers to family members and friends, who
are the primary sources of care (Llanque et al, 2016).
Elderly well-being, is not just focused on disease
or curing the disease, because majority of geriatric
patients have chronic illness. Therefore, the need of
“care” become necessary to improve or maintain the
physical and cognitif function. The role of CGA
takes places to assess the functional status of the
geriatric patients as a central focus and optimize care
outcomes. This tools also used to construct the
planning of treatment such listing the comprehensive
and inclusive of functional problem for appropriate
targetting of interventions. The functionl status is
measured before and after treatment to determine the
effectiveness and efficiency of care and utilized the
necessity level of care (Pilotto, 2018).
2.5 Geriatric Rehabilitation
The most important point for geriatric rehabilitation
is maintaining the continuity of care by tracked the
patients through the system over time, and use the
care management for those with greated degrees of
disablement or handicap patient to receive additional
support. Several benefits are achieved by using CGA.
First benefit is aspect of care process, physician
could find a new diagnoses or problems uncovered
by the instrument. Second is patient outcomes, when
intervention done according problem discovered by
CGA, the score of functional status, affective, and
cognitive function could improving, and further
resulting in prolonged survival of the patients. The
third is using the nursing home, CGA can improved
placement, and reducing mean days in nursing home.
The last is health care use and costs, by improving
the use of home health care, so the using of hospital
services (mean days and hospital rates) and medical
care cost can be reduced (Pilotto, 2018).
2.6 Application CGA in Geriatric
Rehabilitation
A hallmark of geriatrics is emphasis on the
functional ability of older patients. This approach
recognizes that although individual diseases are
important and that our system of modern medicine is
oriented toward the diagnosis and treatment of
specific diseases, the consequences of single and
multiple diseases can be understood best by
evaluating the functional status of the patient (Halter
et al, 2017).
Nowadays, WHO using ICD (International
Classification of Diseases) model for approaching
diagnosis and treatment of the disease. As noted
above, functional status play very important role,
assessing the patient should also use the model of
ICF which as an integrative model of functioning
and environmental factors. This assessment could
become a comprehensive one covers the need of
“cure” and “care” in elderly, and noted that the
functional status is the end result of various efforts
of geriatric approach to care (Pilotto, 2018).
Clinical practice in order to structure the clinical
description and assesment of functioning, apply the
ICF Core Sets. This should be use in practical for
everyday use by presenting the most relevant
categories (health condition, condition group, and
healthcare context). Items of the Geriatric ICF Core
Set (GeriatrICS) grouped into clusters of health
related problems as experienced by community-
dwellling elderly in frail group devided into mental
function, physical health, mobility, personal care,
nutrition, and support (Spoorenberg et al, 2019).
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
50
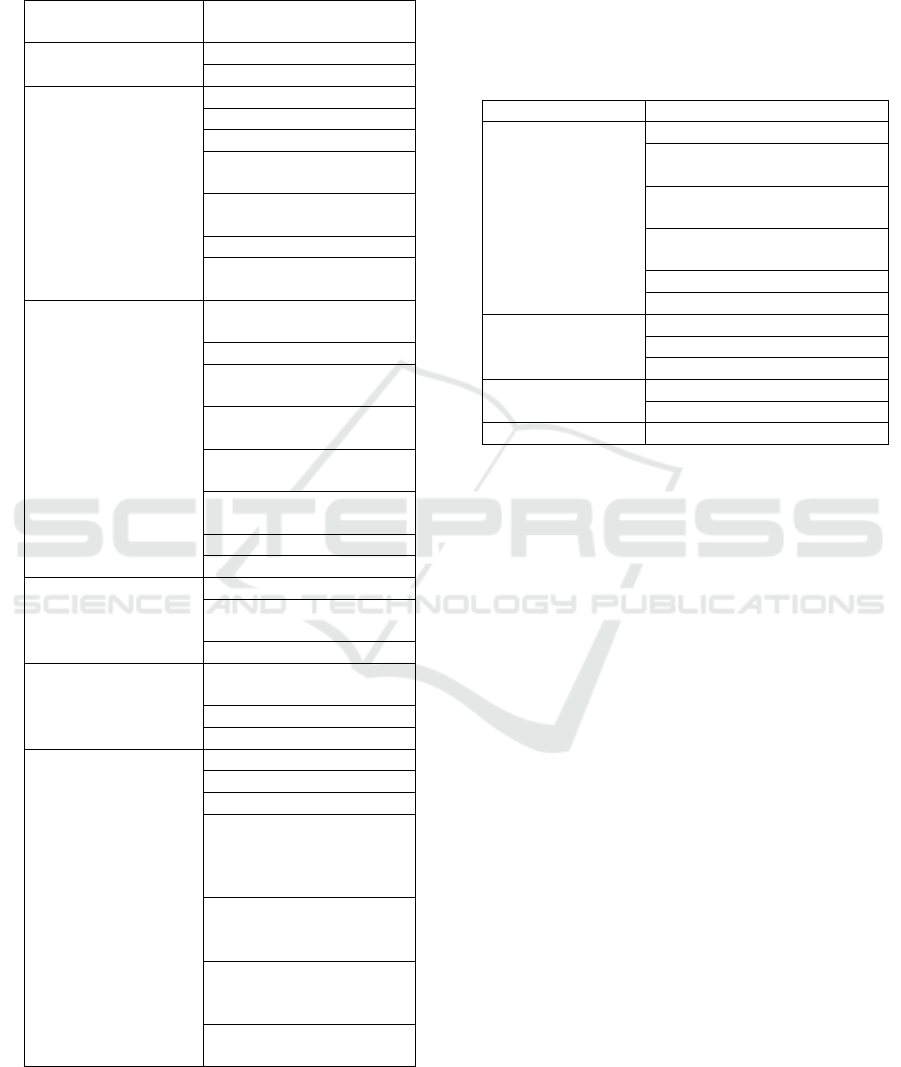
Table 1: Areas of Concern Based on the Geriatric ICF
Core Set (GeriatrICS) (Spoorenberg et al, 2019)
Cluster
GeriatrICS Item (ICF
Category)
Mental Functions
b144 Memory functions
b152 Emotional functions
Physical Health
b210 Seeing functions
b230 Hearing functions
b410 Heart functions
b420 Blood pressure
functions
b525 Defecation
functions
b620 Urination functions
b810 Protective functions
of the skin
Mobility
b240 Sensations
associated with hearing
and vestibular function
b455 Exercise tolerance
functions
b710 Mobility of joint
functions
b730 Muscle power
functions
d410 Changing basic
body position
d450 Walking
d470 Using transportation
Personal Care
d510 Washing oneself
d520 Caring for body
parts
d540 Dressing
Nutrition
b530 Weight maintenance
functions
d550 Eating
d560 Drinking
Support
d760 Family relationships
e310 Immediate family
e320 Friends
e325 Acquaintances,
peers, colleagues,
neighbors and community
members
e570 Social security
services, systems and
policies
e575 General social
support services, systems
and policies
e580 Health services,
systems and policies
CGA as tools used for this comprehensive
assesment done by 4 step, with SOAP (Subject,
Object, Assessment, and Plan) which familiar in
daily clinical practice. This step used to approach to
organizing patient information and collect subjective
and objective database. Later, this data integrate into
assessment and following with discharge planning
and create a care plan (Pilotto, 2018).
Table 2: SOAP model in CGA
Step
Content
Step 1
Subjective and
Objective Database
Chief complaint
Biomedical data impact to
physical & mental function
Assess impact of each
medication effect to function
Psychological data effect to
function
Summary scales of function
Physical examination
Step 2
Assessment
Overview
Areas of concern
Prognosis of function
Step 3
Discharge Planning
Care Plan
Step 4
Checklist
2.7 Assesing of the CGA
The first step of assessing CGA is subjective and
objective database by viewing from both patient’s
and family or caregiver’s word, and finding the
specific functional losses of geriatric patients.
Biomedical data collect the history of medical
diagnosis and history of medication, with a
statement of duration and impact on patient’s
physical and mental function (include appetite,
sexual, performance, constipation, and incontinence).
Another aspect is nutritional data, includding any
changes in weight, appetite, the way of feeding and
swallowing problems (Pilotto, 2018).
Psychological data including assessing the
cognitive function (include any episodes of ACS
following medications, hospitalizations, surgery, or
change of living situation). Its also explore the
emotional function, screen for depression, anxiety,
personality, and coping styles. The last is evaluate
the perceptive function (include vision, hearing, and
speech). Social data also assessed, including
individual social skills (include marital history,
issues of physical and emotional intimacy, need for
control, acceptance of help, and presence of
confidant). Identifying family support system,
primary contact (include list of other potential
caretakers and use of existing community resources).
Explore patient’s feeling about medical treatments
How to Applicate Comprehensive Geriatric Assessment in Geriatric Rehabilitation
51

(such as surgery, hospitalization, NGT, ventilators,
and CPR). Don’t forget to check the document
existence of prior directive (durable power of
attorney, living will, DNR, and Physician Order for
Scope of Treatment (POST). The last is summary
scales of function and physical examination (Pilotto,
2018).
Second step is assessment, integrating the patient
data and organize the problem list. There are 9
areaas of concern such as diagnosis, medication,
nutrition, continence, defecation, cognition, emotion,
mobility, and cooperation with care plan. This care
concern if systematically reviewed in preparing
discharge planning and care plan, lead to improve
health outcomes and satisfaction. This can be used
as a problem checklist to identify areas relevant to
the individual patient and as the goals of care. A
comprehensive view of the complexity ill patient can
be obtained and help the physician to provide
accurate prognostic information to both of patients
and their families (Pilotto, 2018).
The next step is discharge planning and care plan.
The care plan is reconciliation between standards of
medical practice and patient preference. Reconciling
standard medical practice and patient reference is the
most critical step in creating an appropriate and
successful care plan for patients. Physician should
identify reversible or potentially treatable factors in
each area of concern and make treatment
recomendation against the patient’s preference (e.g
no no hospitalization or surgery, no feeding tubes,
no NH placement, no chemotherapy). It is important
to consider individual preferences in each area of
concern. Once recommendation have been
reconciled with the patient’s preferences, common
goals and treatment can proceed (Pilotto, 2018).
Discharge planning is an interdisciplinary
approach to continuity of care; it is a process that
includes identification, assessment, goal setting,
planning, implementation, coordination, and
evaluation and is the quality link between
hospitals, community based services,
nongovernment organizations, and carers. It has five
component, abbreviated as IDEAL, consist of
include, discussion, education, assess, and listen.
Physician should including the patients and family
as a partners in the process of discharge planning.
The next is dicussion should be done with the patient
and family about five key prevent the problem in
house, such as describing how is living at home,
what medication is given, warning the possible
problem, explain the result of examination or
treatment, and make a schedule for the next visit
(Lin et al, 2012).
Throughout the hospital stay and at discharge,
patient and family education is critical in teaching
self-care skills and promoting treatment adherence.
Train and assess the staff on their ability to explain
health information to patients and caregivers and to
use proven teaching methods such as teach-back.
The last is listen to what patients and families have
to say about their needs, concerns, and goals (Lin et
al, 2012).
Outcome measures usually include the following:
length of stay in hospital; readmission rate to
hospital; complication rate; place of discharge;
mortality rate; patient health status; patient
satisfaction; carer satisfaction, both professional and
nonprofessional; psychological health of patient;
psychological health of carers; cost of discharge
planning to the hospital and the community; and use
of medication (Lin et al, 2012).
The last step of CGA is checklist, used to
monitor outcomes of care. The nine areas of concern
provide a comprehensive and convenient checklist
which the physician can monitor the outcomes of
care plan recommendations. Checklist could
reevaluate the patient’s current medical and
functional status. Further, of up-to-date care plans
that reflect new findings can be created (Pilotto,
2018).
CGA may be done by one person or through an
interdiciplinary team approach. Interdiciplinary
approach defined by combining knowledge and
methods from different disciplines, using effective
methods of synthesis (e.g combining of internal
medicine, rehabilitation medicine, and psychiatric).
CGA needs to be providing comprehensive care to
geriatric patients, collaboration and team
communication; well planned team meeting;
pantient specific goals; clearly understood and
agreed by all members (Pilotto, 2018).
3 CONCLUSION
CGA is the comprehensive and multidiciplinary
instrument for assessing geriatric patients, who need
a special approach due to multiple problem
associated with aging. This tools not only focused on
disease itself, but also places high value on
functional status based on ICF model, or using ICF
Core Sets in daily clinical practice. CGA has four
step consist of SOAP model, which is familiar to
physician. CGA and multidisciplinary intervention
can improve health outcomes of older people at risk
of deteriorating health and admission to hospital,
and further maintain the functional status of elderly.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
52

Elderly patients can be remain physically
independent through a longer period of their life, and
reducing their morbidity.
REFERENCES
Dagli RJ, Sharma A. 2014. Polypharmacy: A Global Risk
Factor for Elderly People. J. Int Oral Health. 6(6):i-ii
Dai Y, Zhang CY, Zhang BQ, et al. 2016. Social Support
and The Self-Rated Health of Older People: A
Comparative Study in Tainan Taiwan and Fuzhou
Fujian Province. Medicine (Baltimore). 95(24):e3881
Dodds R, Sayer AA. 2016. Sarcopenia and Frailty: New
Challenges for Clinical Practice. Clin Med (London).
16(5):455-8
Halter JB, Ouslander JG, Studenski S. 2017. Hazzard's
Geriatric Medicine and Gerontology. McGraw-Hill,
United States, 7th edition
Kementerian Kesehatan RI. 2019. Indonesia MasukI
Periode Aging Population [internet]. Jakarta:
Kementerian Kesehatan RI;[cited 2 October 2019].
Available from: http://www.depkes.go.id/
Lin CJ, Cheng SJ, Shih SC, et al. 2012. Discharge
Planning. International Journal of Gerontology.
6(4):237-240
Llanque S, Savage L, Rosenburg N, et al. 2016. Concept
Analysis: Alzheimer’s Caregiver Stress. Nurs Forum.
51(1):21-31
Manini, T. 2011. Development of Physical Disability in
Older Adults. Curr Aging Sci. 4(3):184-191
Nigam Y, Knight J, Bhattacharya S, et al. 2012.
Physiological Changes Associated with Aging and
Immobility. J Aging Research. 2012:468-9
Osoba MY, Rao AK, Agrawal SK, et al. 2019. Balance
and Gait in the Elderly : A Contemporary Review.
Laryngoscope Investig Otolaryngol. 4(1):143-153
Pilotto, A. 2018. Practical Issues in Geriatric
Comprehensive Assessment. Springer, Switzerland
Sloane PD, Cesari M. 2018. Research on Frailty:
Continued Progress, Continued Challenges. The
Journal Post-Acute and Long-Term Medicine.
19(4):279-281
Spoorenberg SLW, Reijneveld SA, Uittenbroek RJ, et al.
2019. Health-Related Problems and Changes After 1
Year as Assessed With the Geriatric ICF Core Set
(GeriatrICS) in Community-Living Older Adults Who
Are Frail Receiving Person-Centered and Integrated
Care From Embrace. American Congress of
Rehabilitation Medicine.
Spoorenberg SLW, Uittenbroek RJ, Middel B, et al. 2013.
Embrace, A Model for Integrated Elderly Care: Study
Protocol of A Randomized Controlled Trial on The
Effectiveness Regarding Patient Outcomes, Service
Use, Costs, and Quality of Care. BMC Geriatrics.
13:62
World Health Organization. 2018. Ageing and Health.
Geneva: World Health Organization
How to Applicate Comprehensive Geriatric Assessment in Geriatric Rehabilitation
53
