
A Rare Case of Mediastinal Yolk Sac Tumor
Andhika Kesuma Putra
1
, Noni Novisari Soeroso
1*
and Muhammad Zainul Akbar
1
1
Department of Pulmonology and Respiratory Medicine, Faculty of Medicine, Universitas Sumatera Utara,
Universitas Sumatera Utara Hospital, Jl. Dr. Mansyur No. 5 Medan 20155, Sumatera Utara, Indonesia
Keywords: Yolk sac, Germ cell tumor, Core biopsy
Abstract: Yolk sac tumor is a germinal cell tumor that commonly causes testicular malignancy. The incidence of these
tumors lies in 90-95% of all testicular malignancies and commonly affects children with a median age of 1.5
years. In mixed type in adults, these tumors present in the age group 25-30 years. We reported a case of a
63-year-old man, who suffered from shortness of breath, accompanied by weight loss. Chest x-ray showed a
homogeneous consolidation in the mediastinum. With suspicion of a mediastinal tumor, the patient
underwent a core biopsy of the mass in the mediastinum. On histopathology examination showed
pleomorphic tumor cell form, enlarged nucleus, hyperchromatic, eosinophilic cytoplasm. The tumor cells
appear to form Schiller-Duval bodies. This case was diagnosed as a yolk sac tumor and underwent
chemotherapy.
1 INTRODUCTION
Germ cell tumor is a group of benign and malignant
neoplasm originated from primitive germ cell during
early embryogenesis. Germ cell tumor frequently
occurred in the gonads, only 5-10 % happened in the
extra gonad. Extragonadal germ cell tumor is mostly
found in the anterosuperior mediastinal (Bokemeyer
et al., 2002).
Primary yolk sac tumor in the anterior
mediastinum is rare and has a vicious prognosis.
Patients often present with advanced stage tumors
that are bulky and unresectable. Like other germ cell
tumors, yolk sac tumor is predominantly a disease of
young adults. However, a few cases of gonadal and
extragonadal germ cell tumors have been reported in
elderly patients as well (Nakhla and Sundararajan,
2016). We present a very rare case of an elderly 63-
year-old male with primary yolk sac tumor of the
mediastinum.
2 CASE REPORT
A 63-year-old male was admitted with shortness of
breath that he had been suffering for the past 3
months. Shortness of breath was not related to
physical activity or weather changes. The patient
also complained of cough that he had experienced in
the previous 2 months without any sputum
production. Systemic complaints experienced by
patient included very rapid weight loss during the
last 6 months and sub-febrile fever during the last 1
month. His vital signs were as follows: blood
pressure 120/80 mmHg, pulse rate of 112 beats per
minute, respiratory rate of 28 breaths per minute,
and temperature of 37.4
o
C. Based on the laboratory
findings, Hemoglobin was 12.5 gr%, leukocytes
were 9100 / mm
3
, and platelets were 424,800/mm
3
respectively. Atrial blood gas results were pH 7.45,
pCO
2
39.7 mmHg, pO
2
110.2 mmHg, HCO
3
27.9
mmol/L, BE 2,9 SaO
2
98.8%. Chest x-ray showed
widening in the mediastinal segment. With suspicion
of a mediastinal tumor, the patient underwent a core
needle biopsy of the mass in the mediastinum guided
by thoracic CT scan (Figure 1-3). Histopathology
results showed pleomorphic tumor cell form,
enlarged nucleus, hyperchromatic, eosinophilic
cytoplasm (Figure 4). The tumor cells appear to
form Schiller-Duval bodies. This case was
diagnosed as a yolk sac tumor and the patient
underwent chemotherapy.
Putra, A., Soeroso, N. and Akbar, M.
A Rare Case of Mediastinal Yolk Sac Tumor.
DOI: 10.5220/0009841000090011
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 9-11
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
9
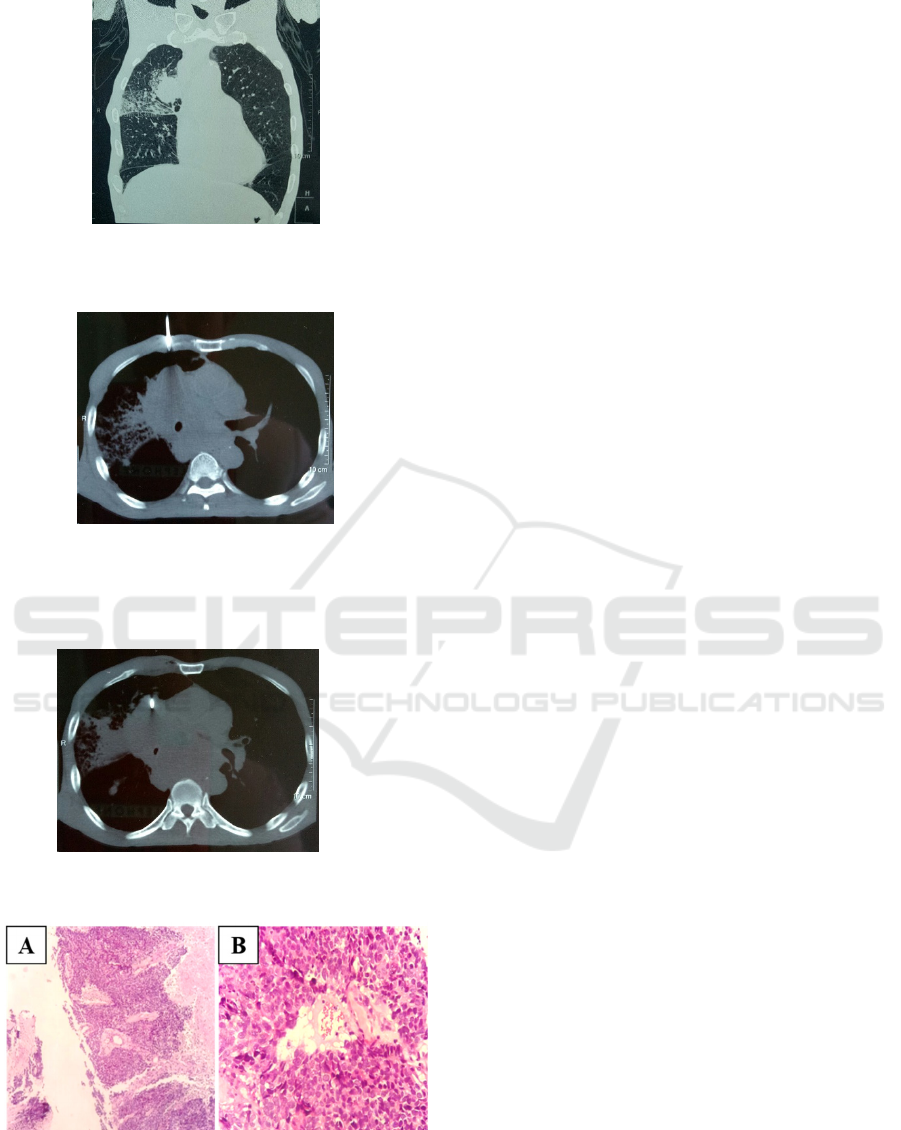
Figure 1: Coronal slice of Thorax CT showed the mass in
the right upper lobe.
Figure 2: Thorax CT showed needle marker in the
insertion phase.
Figure 3: Thorax CT showed needle marker in the tumor
site.
Figure 4: (A) Histopathology examination showed
pleomorphic tumor cell form, enlarged nucleus,
hyperchromatic, eosinophilic cytoplasm. (B) The tumor
cells appear to form Schiller-Duval bodies.
3 DISCUSSIONS
Germ cell tumors mostly occur in the gonads.
Extragonadal germ cell tumors are rare and most can
arise in the pineal gland, retroperitoneum, and the
mediastinum. The mediastinum is the most common
site of extragonadal germ cell tumors. Malignant
germ cell tumors in the mediastinum account for 1–
6% of all mediastinal tumors. Primary extragonadal
germ cell tumors, especially primary mediastinal
tumors, are considered to have a poor prognosis.
Germ cell tumors are histologically categorized into
teratomas, teratocarcinomas, seminomas, and
nonseminomatous carcinoma, including
choriocarcinoma, embryonal carcinoma, yolk sac
carcinoma, and mixed type carcinoma. Greater than
90% of malignant extragonadal tumors of the
mediastinum occur in men (Bokemeyer et al., 2002;
Nakhla and Sundararajan, 2016). In a retrospective
study by Sakurai et al. (2004) with 48 patients of
extragonadal germ cell tumors, the median age at
presentation was 28.8 years.
Yolk sac tumors can occur in both men and
women, usually arising from germ cells in testes and
ovaries, respectively. Pure yolk sac tumors are
usually found in young children and mixed germ cell
tumors with yolk sac are found in the adult. Similar
to other nonseminomatous germ cell tumors, the
latter can be associated with hematologic
Klinefelter’s syndrome (up to 20%) and other
hematological malignancies such as acute leukemia
and myelodysplastic syndrome. In an international
study by Bokemeyer et al. (2001) with 381
mediastinal germ cell tumors, the most common
symptoms on presentation were dyspnea (25%),
chest pain (23%), cough (17%), fever (13%), night
sweat, or weight loss (11%). Night sweat, fatigue,
hemoptysis, and symptoms of superior vena cava
compression were seen in <10% of patients with
mediastinal germ cell tumors (Nakhla and
Sundararajan, 2016).
Histologically, extragonadal germ cell tumors
and mediastinal germ cell tumors have many
similarities. Schiller-Duval bodies are
pathognomonic and are helpful for identification.
Yolk sac tumors immunohistochemical testing is
positive for AFP, glypican-3, SALL4, and placental
alkaline phosphatase (Bokemeyer et al., 2002;
Sakurai et al., 2004).
The treatment regimens of extragonadal and
gonadal yolk sac tumors are similar since they share
histological patterns. Extragonadal
nonseminomatous germ cell tumors have a
considerably poorer prognosis. Chemotherapeutic
schemes based on cisplatin have shown significant
results with up to 50% of patients achieving long-
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
10

term survival (Sakurai et al., 2004).
Bleomycin-
Etoposide-Cisplatin (BEP) therapy or etoposide
(Vepesid), ifosfamide, and cisplatin (VIP), with at
least 4 cycles of chemotherapy, are widely accepted
regimens. VIP regimen may be preferred over BEP
since patients with mediastinal germ cell tumors
might need postchemotherapy thoracotomy for
removal of residual tumor and bleomycin-induced
pulmonary toxicities can be potentiated by surgery
(Giannis et al., 2009).
Surgical resection as the primary treatment
modality is not recommended in mediastinal germ
cell tumors because of the likelihood of early
metastasis. However, there is a definite role for
postchemotherapy adjuvant surgery to remove
residual lesions and a rising serum tumor marker
after completion of chemotherapy is not considered
as a contraindication for surgery. Complete
resolution of serum AFP marker occurs in less than
5% of patients. Survival rates have increased in
patients who have the serum of AFP decreased after
chemotherapy and in cases with residual tumor
surgical excision (Vuky et al., 2001).
Elderly patients with germ cell tumor generally
have worse clinical outcomes compared to younger
patients. A Surveillance, Epidemiology, and End
Results (SEER) database analysis of 12,811 patients
comparing the outcomes of testicular cancers in
young adults (age <50) versus older adults (age >50
years) found survival from both localized and
metastatic nonseminomatous germ cell tumors to be
much better in younger patients compared to elderly
(76.9% versus 57.0%) (Bokemeyer et al., 2002;
Sakurai et al., 2004). Our patient had an overall poor
prognosis due to multiple reasons such as his age,
tumor location, and tumor bulk.
FUNDING
No grant support or funding from public institutions
or private enterprises was received for this case
report.
ACKNOWLEDGMENTS
The researcher would like to thank Columbia Asia
Hospital and Universitas Sumatera Utara Hospital
which have allowed the retrieval of medical history
data.
REFERENCES
Bokemeyer, C. et al., 2002. Extragonadal germ cell
tumors of the mediastinum and retroperitoneum:
Results from an international analysis. Journal of
Clinical Oncology. 20(7): 1864–1873. doi:
10.1200/JCO.2002.07.062.
Giannis, M. et al., 2009. Cisplatin-based chemotherapy for
advanced seminoma: Report of 52 cases treated in two
institutions. Journal of Cancer Research and Clinical
Oncology. 135(11): 1495–1500. doi: 10.1007/s00432-
009-0596-2.
Nakhla, S. G. and Sundararajan, S., 2016. A Rare Case of
Primary Anterior Mediastinal Yolk Sac Tumor in an
Elderly Adult Male. Case Reports in Oncological
Medicine. 16(4): 8961-8965. doi:
10.1155/2016/8961486.
Sakurai, H. et al., 2004. Management of primary
malignant germ cell tumor of the mediastinum.
Japanese Journal of Clinical Oncology. 34(7): 386–
392 doi: 10.1093/jjco/hyh062.
Vuky, J. et al., 2001. Role of postchemotherapy adjunctive
surgery in the management of patients with
nonseminoma arising in front of the mediastinum.
Journal of Clinical Oncology. 19(3): 682–688. doi:
10.1200/JCO.2001.19.3.682.
A Rare Case of Mediastinal Yolk Sac Tumor
11
