
The Difference of Spirometry Result before and after Coronary
Artery Bypass Graft Procedure
Yosep Aloys Hamonangan
1*
, Marshal
2
and Doddy Prabisma Pohan
2
1
Department of General Surgery, Universitas Sumatera Utara/ Haji Adam Malik Hospital, Medan, Indonesia
2
Department of General Surgery, Division of Thoracic and Cardiovascular Surgery, Universitas Sumatera Utara/ Haji
Adam Malik Hospital, Medan, Indonesia
Keywords: Coronary artery bypass graft, spirometry, pulmonary function
Abstract: To evaluate the differences of pulmonary function test before and after CABG procedure. A descriptive
analytic cohort study was performed in Division of Cardiothoracic Surgery, Department of Surgery, H.
Adam Malik General Hospital, Medan, Indonesia from January 2018 to January 2019. All patients was
underwent coronary artery bypass graft procedure in our center from October 2017 to April 2018. A
preoperative pulmonary function test was compared with postoperative CABG results. A total of 35 patients
were included in the study, averaging 57.6 (± 4.6) years old. The
FEV1/FVC before and after CABG
procedure were recorded with the mean value of 75.97
± 6.22 and 89.35 ± 5.59 respectively. A
statistically significant difference was noted (p<0.001). An improvement of pulmonary function test after
CABG was found compared to preoperative pulmonary function test.
1 INTRODUCTION
Coronary Artery Bypass Graft (CABG) is one of the
most common surgical procedure done, account for
approximately 400.000 operation each year in the
United States. In the last decade, there was a trend
towards less CABG procedures due to percutaneous
coronary intervention (Alexander, 2016).
A CABG procedure was introduced in the 1960
by creating two parallel way to bypass the coronary
artery obstruction, using either internal mammary
artery (IMA) or saphenous vein graft (SVG).
Cardiac surgeon mostly prefer SVG in performing
CABG procedure in 1970. However, during the
present days, most patients were underwent the
surgery using a left IMA (LIMA) (S-hikhman,
2011).
One of the drawbacks of CABG procedures is
the negative effect on pulmonary function.
Pulmonary function test such as VC, FVC, FEV1,
FEV1/FVC, and MVV have lower results after the
surgery compared to before surgery (El-Sobkey,
2011). The decreased of the pulmonary function
could remained for 4-6 months, moreover as long as
1 year, after surgery (Westerdahl, 2016).
From these findings, pulmonary complications
after cardiac surgery are multifactor phenomenon
and statistical explanation to describe these
problems is mandatory (El-Sobkey, 2011). In this
study, we aimed to evaluate if there were any
differences of pulmonary function test before and
after CABG procedure.
2 METHODS
A descriptive analytic cohort study was performed to
all patients who underwent CABG procedures in
Division of Cardiothoracic Surgery, Department of
Surgery, H. Adam Malik General Hospital, Medan,
Indonesia from January 2018 to January 2019. All
CABG patients from October 2017 to April 2018
was our first inclusion criteria. In this study all
patients were between 20 to 60 years old, and having
a valid spirometry test results. A history of unstable
cardiovascular condition; cerebral, abdomen, or
pulmonal aneurism; pneumothorax or hemoptysis
for the last month; recent pulmonary or abdominal
surgery; pulmonary infection; and congenital
164
Siregar, Y., Marshal, . and Pohan, D.
The Difference of Spirometry Result before and after Coronary Artery Bypass Graft Procedure.
DOI: 10.5220/0009862501640166
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 164-166
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
pulmonary condition were the exclusion criteria in
this study.
Demographic data of all patients who underwent
the CABG procedure in our center, such as age,
gender, and job were recorded, including pulmonary
test result before surgery. After that, the patients
were called back to the hospital and underwent
history taking and physical examination. All eligible
patients were included into the study and underwent
a spirometry test in the integrated diagnostic center
H. Adam Malik General Hospital, Medan,
Indonesia. A calibrated spirometry tool was used,
and a maneuver to perform spirometry test was
demonstrated before the test.
Statistical analysis using paired T-test was done
to evaluate the pulmonary function before and after
CABG procedure.
3 RESULTS
A total of 51 patients were underwent spirometry
examination before CABG procedures, 10 patients
did not come for the spirometry test after CABG
procedures. Six patients were diagnosed with
chronic obstructive pulmonary disease (COPD) and
excluded from the study. Finally, 35 patients were
included in the study. The mean of age of all
participants was 57.6 ± 4.6 years old and men were
noted in 22 patients (62.9%) compared to 13
(37.1%) women.
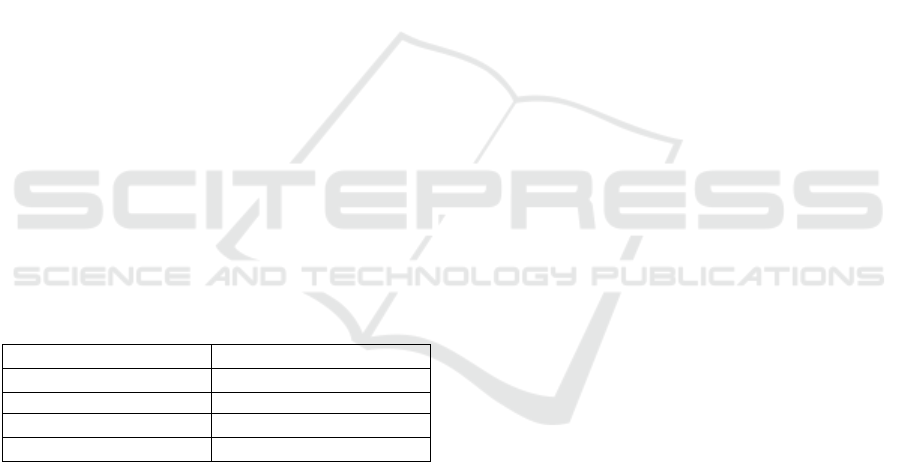
Table 1: Demographic characteristics
Characteristics (n=35)
Mean ± SD
Age
57.6
± 4.6
FEV1/FVC
Before CABG
75.97%
± 6.22
After CABG
89.35
± 5.59
The
ratio of FEV1 to FVC before and after CABG
procedure were averaging 75.97 ± 6.22 and 89.35 ±
5.59 respectively. These indicate no obstructive
symptoms in all of our patients. Subsequently, a
paired T-test was done and showed a statistically
significant result, p<0.001.
4 DISCUSSION
A significant change was noted in the vital capacity
after miocardiac revascularization. In the first day
postoperative, an approximately 70% decrease was
found in comparison of preoperative result. After
that, a rise will be found gradually, mostly after the
patients out from the hospital. Cardiac surgery was
also proved to have a negative effect on the
pulmonary function. All of the test results, including
VC; FVC; FEV1; FEV1/FVC were lower
postoperatively compared to preoperative setting.
Several studies have supported these findings
(Shenkman et al., 1997; Saxena et al., 2007;
Weissman, 1999; Stenseth et al., 1996; Vaidya et al.,
1996).
Spirometry test was used because it was an
objective, valid, and capable to evaluate pulmonary
function test. Moreover, it was a non-invasive
method especially for postoperative patients.
Pulmonary hypertension could be caused by
combination of increase left atrial pressure,
pulmonary arteriole narrowing, and organic change
in the pulmonary vessels. Pulmonary dysfunction
was related to interstitial and alveolar edema,
reactive fibrosis, previous pulmonary infarct, pleural
effusion, and decrease of pulmonary volume
postoperatively Shenkman et al., 1997; Saxena et al.,
2007; Weissman, 1999; Stenseth et al., 1996; Vaidya
et al., 1996).
Women were tend to have a lower pulmonary
function test score compared to men as they may
have a worse reaction to pain. This may explain the
reason of lower pulmonary function test was noted
in valve replacement surgery compared to CABG.
But further question is whether there could be
another factors explaining the findings. A proposed
mechanism is inflammatory respons that secreted in
the pulmonary system and resulted in pulmonary
dysfunction or edema (Mahmoud et al, 2005; Barnas
et al, 1994). Beside the worse gas exchange, a
decrease in FVC, FEV1, PEF was more common in
a longer cardiopulmonary bypass procedure (more
than 80 minutes) (Kochamba et al, 2000; Chandra et
al, 1998).
Compared to alternative study, we have a similar
result. A difference in pulmonary function test with
spirometry before and after CABG procedure could
be a threshold in assessing respiratory quality in post
CABG patients. An increasing pulmonary function
test after CABG was found compared to
preoperative pulmonary function test.
REFERENCES
Alexander, J.H., Smith, P.K., 2016. Coronary-Artery
Bypass Grafting. N Engl J Med. 374: 1954–1964.
Barnas, G.M., Watson, R.J., Green, M.D., Sequeira, A.J.,
Gilbert, T.B., Kent, J., Villamater, E., 1994. Lung and
chest wall mechanical properties before and after
cardiac surgery with cardiopulmonary bypass.
The Difference of Spirometry Result before and after Coronary Artery Bypass Graft Procedure
165

Chandra, Shenkman, Z., Shir, Y., Weiss, Y.G., et al. 1997.
The effects of cardiac surgery on early and late
pulmonary function. Acta Anaesthesiol Scand
41:1193-1199.
El-Sobkey, S.B., Gomaa, M., 2011. Assessment of
pulmonary function tests in cardiac patients. J Saudi
Hear Assoc. 23: 81–86.
Kochamba, G.S., Yun, K.L., Pfeffer, T.A., Sinte, C.F.,
Khonsari, S., 2000. Pulmonary abnormalities after
coronary arterial bypass grafting operation:
Cardiopulmonary bypass versus mechanical
stabilization. Ann. Thorac. Surg. 69 (5), 1466–1470.
Mahmoud, A.B., Burhani, M.S., Hannef, A.A., Jamjoom,
A.A., AlGithmi, I.S., Baslaim, G.M., 2005. Effects of
modified ultrafiltration on pulmonary function after
cardiopulmonary bypass. Chest 128 (5), 3447–3453.
S–hikhman, M., Scott, A., 2013. Coronary Artery Bypass
Grafting (CABG). J Chem Inf Model. 53: 16891699.
Saxena, P., Luthra, S., Dhaliwal, R.S., Rana, S.S., Behera,
D., 2007. Early changes in pulmonary functions after
mitral valve replacement. Ann. Thorac. Med. 2 (3),
111–117.
Shenkman, Z., Shir, Y., Weiss, Y.G., Bleiberg, B., Gross,
D., 1997. The effects of cardiac surgery on early and
late pulmonary functions. Acta Anaesthesiol Scand.
41:1193–9.
Stenseth, R., Bjella, L., Berg, E.M., Christensen, O.,
Levang, O.W., Gisvold, S.E., 1996. Effects of thoracic
epidural analgesia on pulmonary function after
coronary artery bypass surgery. Eur. J. Cardiothorac.
Surg. 10, 859–865.
Vaidya, R., Husain, T., Ghosh, P.K., 1996. Spirometric
changes after open mitral surgery. J. Cardiovasc.
Surg. 37 (3), 295–300.
Weissman, C., 1999. Pulmonary function after cardiac
and thoracic surgery. Anesth. Analg. 88, 1272.
Westerdahl, E., Jonsson, M., Emtner, M., 2016.
Pulmonary function and health-related quality of life
1-year follow up after cardiac surgery. J Cardiothorac
Surg. 11: 1–8.
Moore, R., Lopes, J., 1999. Paper templates. In
TEMPLATE’06, 1st International Conference on
Template Production. SCITEPRESS.
Smith, J., 1998. The book, The publishing company.
London, 2
nd
edition.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
166
