
A Case Report: The Clinical Features and Treatment Challenges of
HIV-associated Psoriasis
Teffy Nuary
1*
, Anissa Anjani
1
, Anna Ariane
2
,Lili Legiawati
1
, Sri Adi Sularsito
1
,
Shannaz Nadia Yusharyahya
1
, Rinadewi Astriningrum
1
1
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia
Dr. Cipto Mangunkusumo National Central General Hospital, Indonesia
2
Department of Internal Medicine Faculty of Medicine Universitas Indonesia
Dr. Cipto Mangunkusumo National Central General Hospital, Indonesia
Keywords: Psoriasis, Erythrodermic, Arthritis, HIV, Methotrexate
Abstract: Psoriasis is a chronic inflammatory skin disease, characterized by complex alterations in epidermal growth,
differentiation as well as multiple biochemical, immunologic, and vascular abnormalities. The prevalence of
human immunodeficiency virus (HIV)-associated psoriasis, and HIV-associated psoriatic arthritis may or
may not be the same as in the general population. Misleading, unusual clinical presentations, severe disease,
and frequent exacerbations are characteristicfindings.Many effective drugs for psoriasis and psoriatic
arthritis are immunosuppressive agents. Therefore, the treatment for the HIV-infected patient is more
challenging. A 64-year old female, the HIV-infected patient, was hospitalized because of severe generalized
skin rash (92% of BSA, PASI: 28.2) with scaling. She diagnosed with HIV 7 years ago with a CD4 count of
500 cells/uL. The patient took antiretroviral therapy (lamivudine, nevirapine, and tenofovir) regularly. She
was diagnosed with erythrodermic psoriasis and psoriatic arthritis. After the risk of opportunistic infection
was eliminated, she receivedmethotrexate (MTX) 7.5 mg/week, and the dose was increased into 10
mg/week.Two months following the treatment, there was clinical improvement (4% of BSA and PASI: 2),
without the presence of any opportunistic infections and MTX’s adverse events. Although there are limited
data on the efficacy and safety of systemic immunosuppressive agents for the treatment of psoriatic disease
in HIV-positive patients,adequate concomitant antiretroviral therapy and close monitoring for the signs and
symptoms of infectionmight reduce the likelihood of acute infection.
1 INTRODUCTION
Psoriasis is a chronic inflammatory skin disease with
a strong genetic basis, characterized by complex
alterations in epidermal growth, differentiation as
well as multiple biochemical, immunologic, and
vascular abnormalities. The relationship to a nervous
system function is poorly understood. The root cause
remains unknown.(Gudjonsson et al., 2012)
The prevalence of human immunodeficiency
virus (HIV)-associated psoriasis, and HIV-
associated psoriatic arthritis may or may not be the
same as in the general population.(Zancanaro et al.,
2006; Morar et al., 2010). Misleading, unusual
clinical presentations, severe disease, and frequent
exacerbations are characteristic findings. Psoriasis
might worsen the HIV infection or might be detected
for the first time concomitantly with HIV. It can be
very severe, but it can regress before death. The
development of HIV-associated psoriasis and HIV-
associated psoriatic arthritis might be associated
with poor prognosis in untreated patients, with a
mean life expectancy ranging from 4 to 24 months
following the diagnosis of psoriasis. (Morar et al.,
2010).
Many effective drugs for psoriasis and psoriatic
arthritis are immunosuppressive agents. Therefore,
the management for the HIV-infected patient is more
challenging, requiring both careful considerations on
the potential risks and benefits of treatment and
more fastidious monitoring for potential adverse
events. (Morar et al., 2010). In this study, we report
a case of safe and successful therapy with
methotrexate in a 64-year-old female with HIV-
associated psoriasis who responded poorly to
282
Nuary, T., Anjani, A., Ariane, A., Legiawati, L., Sularsito, S., Yusharyahya, S. and Astriningrum, R.
A Case Report: The Clinical Features and Treatment Challenges of HIV-associated Psoriasis.
DOI: 10.5220/0009986802820285
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 282-285
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

previous treatments, which were steroids and
ultraviolet B phototherapy.
2 CASE
A 64-year old female,the HIV-infected patient, was
hospitalized because of severe generalized skin rash
with scaling and joint pain in lower extremities. A
month prior to hospitalization, she began visiting an
outpatient clinic due to rashes and scaling on her
arms, trunk, and legs. She was treated with topical
steroid ointment, 5% liquor carbonic detergents
(LCD), and two courses of the narrow band-
ultraviolet B (NB-UVB) radiation. However, there
was no improvement. She diagnosed with HIV
7years ago with a CD4 count of 500 cells/uL. She
took antiretroviral therapy (lamivudine, nevirapine,
and tenofovir) regularly. She had a history of
smoking since childhood but no history of alcohol
consumption, lithium or β-blocker treatment nor
family history of psoriasis.
Erythematous skin lesions accompanied by silver
whitish scales were observed on her scalp and over
her entire body (92% of body surface area (BSA),
psoriatic area severity index (PASI): 28.2). The
patient was diagnosed with erythrodermic psoriasis.
We consulted to a rheumatologist for her complaint
of arthralgia in lower extremities, and she was
diagnosed with psoriatic arthritis.
Figure 1. Clinical lesions oferythematous skin lesions accompanied by silver-white scales were observed over the patient’s
entire body (92% of BSA, PASI: 28,2).
The laboratory test results were as follows: white
blood cells 8160/uL (63.9% neutrophils,25%
lymphocytes, 6.6% monocytes, 4% eosinophils),
hemoglobin 12.1 g/dL, platelets 273,000/uL;
aspartate aminotransferase 19 U/L, alanine
aminotransferase 18 U/L; total protein 5 g/dL,
albumin 2.94 g/dL, creatinine 1 mg/dL, and CD4 T-
cell count 750 cells/uL. Serology was negative for
anti-hepatitis B virus and anti-hepatitis C virus
antibodies. Venereal disease research laboratory
(VDRL) test and Treponema
pallidum hemagglutination (TPHA) test were non-
reactive.
The patient received sulfasalazine 500 mgbid for
ten days, but there was no clinical improvement.
After the risk of opportunistic infection was
eliminated, the patient received methotrexate(MTX)
7.5 mg/week and folic acid 5 mg/week for one week.
The MTX’s dosewas increased into 10
mg/weekfollowing no sign of hepatotoxicity.Two
months after receiving MTX therapy, there was a
clinical improvement (4% of BSA and PASI: 2). The
MTX was continued, andthe patient was still being
monitored at the outpatient clinic. After five months
of treatment, the patient showed complete
resolutionwithoutexperiencing relapsenor any MTX
adverse events.
A Case Report: The Clinical Features and Treatment Challenges of HIV-associated Psoriasis
283
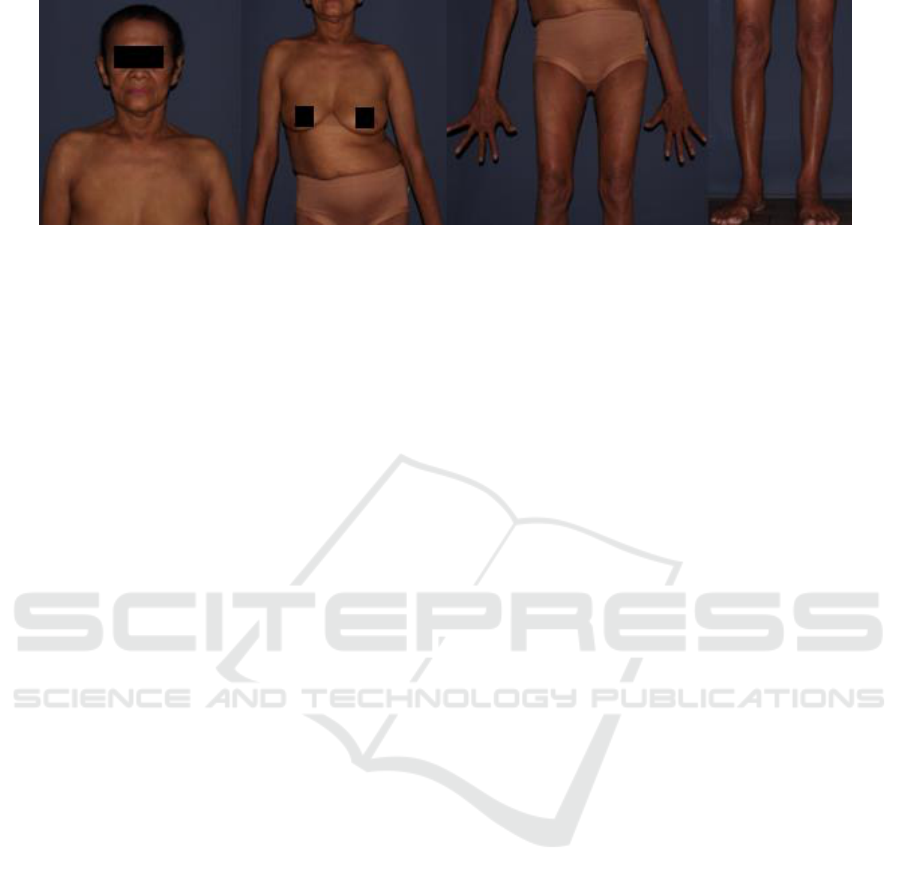
Figure 2. After five months of treatment, the erythematous cutaneous lesions and scaly plaque disappeared.
3 DISCUSSION
The characteristic traits of HIV-associated psoriasis,
which distinguish it from classic seronegative
psoriasis, are sudden onset as well as more severe,
extensive, and recalcitrant nature.(Gaspari AA et al.,
2011) The disease exhibits various morphological
types in the same patients, appearing in one-third of
their disease’s course along with the high frequency
of arthritis. Notably, the exacerbation due to
staphylococcal and streptococcal infection is more
common among HIV-infected individuals. (Morar et
al., 2010). In this case,psoriasis began suddenly, and
it became severe immediately (involving 92% of
BSA), without other risk factors,e.g., excessive
alcohol intake and the use of particular drugs
(lithium and β-blockers).
Psoriasis in HIV-infected patients often responds
poorly to the treatment and has a high morbidity
rate, thus posing a challenge to the clinicians.(Je ong
YS et al., 2014).The treatment of HIV-associated
psoriasis depends on the severity of the disease.
Mild cases (<2% of BSA) can be treated topically
with emollients, corticosteroids, tar, vitamin D
analogs, and retinoids. Meanwhile, moderate and
severe cases (2–10% and <10% of BSA, respec-
tively) can be treated with systemic therapies,
including phototherapy, acitretin, cyclosporin,
hydroxyurea, and tumor necrosis factor-α inhibitors
(e.g., etanercept and infliximab) along with effective
antiretroviral therapy.(De Socio GVL et al., 2006).
This patient was treated with topical steroid
ointment, 5% liquor carbonic detergents (LCD), and
narrow band-ultraviolet B (NB-UVB) radiation, but
there was no clinical improvement.
The treatment of moderate and severe HIV-
associated psoriasis is challenging, and the risk-to-
benefit ratio specific to these patients needs to be
taken into account when selecting therapies.
(Nakamura M et al., 2018)
In this case, after the risk of opportunistic
infection was eliminated, the patient received
MTX.There was a clinical improvement, and she
had not experienced relapse nor any MTX’s adverse
events.In the cases of refractory HIV-associated
psoriasis, more traditional systemic
immunosuppressants, such as cyclosporin A (CsA),
MTX, and hydroxyurea,can be considered under
certain circumstances. The evidence supporting the
use of these agents is limited to a few reported cases,
case series, and anecdotal experiences.(Van
Voorhees et al., 2009) The decision to use a low
dose of MTX should be made on a case-by-case
basis following close consultation with the
appropriate physicians who are caring for the
patient, and cautious use is recommended in the
cases of severe refractory disease.(Nakamura M et
al., 2018)
4 CONCLUSION
Treatment of HIV-associated psoriasis can be
challenging and needs to be tailored to suit the risk-
to-benefit ratio in each patient. Although there are
limited data on the efficacy and safety of systemic
immunosuppressive therapies for the treatment of
psoriatic disease in HIV-positive patients,adequate
concomitant antiretroviral therapy and close
monitoring for the signs and symptoms of infection
might reduce the likelihood of acute infection.
REFERENCES
De Socio GVL, Simonetti S, Stagni G. 2006. Clinical
improvement of psoriasis in an AIDS patient
effectively treated with combination antiretroviral
therapy. Scand J Infect Dis.;38(1):74–5.
Gaspari AA, Gómez-Flores M, Ancer-Rodríguez J, Bryant
JL, Mendez N, Cedeno-Laurent F, et al. 2011.New
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
284

insights into HIV-1-primary skin disorders. J Int AIDS
Soc.;14(1):5.
Gudjonsson J, James E. Psoriasis. In: Lowell AG, Katzi S,
Gilchrest BA, Paller AS, Leffell D, Klaus W.2012.
editor. Fitzpatrick’s Dermatology in General
Medicine. 8 ed. New York: McGraw-Hill;. p. 197–
231.
Jeong YS, Kim MS, Shin JH, Cho JK, Lee HI, Kim HJ, et
al.2014.A case of severe HIV-associated psoriasis
successfully treated with acitretin therapy. Infect
Chemother;46(2):115–9.
Morar N, Willis-Owen SA, Maurer T, Bunker
CB.2010.HIV-associated psoriasis: pathogenesis,
clinical features, and management. Lancet Infect
Dis.;10(7):470–8.
Nakamura M, Abrouk M, Farahnik B, Zhu TH, Bhutani
T.2018. Psoriasis treatment in HIV-positive patients: a
systematic review of systemic immunosuppressive
therapies. Cutis;101(1):38;42;56.
Van Voorhees AS, Gladman DD, Lebwohl MG, Strober
BE, Kalb RE, Bebo BF, et al. 2009. Psoriasis in
patients with HIV infection: From the Medical Board
of the National Psoriasis Foundation. J Am Acad
Dermatol;62(2):291–9.
Zancanaro PCQ, McGirt LY, Mamelak AJ, Nguyen RHN,
Martins CR.2006. Cutaneous manifestations of HIV in
the era of highly active antiretroviral therapy: An
institutional urban clinic experience. J Am Acad
Dermatol;54(4):581–8.
A Case Report: The Clinical Features and Treatment Challenges of HIV-associated Psoriasis
285
