
A Rare Case of Unilateral Psoriasis with Verruca Vulgaris:
Challenges in Diagnosis and Treatment
Marsha Bianti
1*
, Shannaz Nadia Yusharyahya
1
,Sondang P. Sirait
1
,
Eyleny Meisyah Fitri
1
, Endi Novianto
1
1
Department of Dermatology and Venereology, Faculty of Medicine Universitas Indonesia/
Dr. Cipto Mangunkusumo National Central General Hospital, Indonesia
Keywords: HPV, Unilateral Psoriasis, Verruca Vulgaris
Abstract: Unilateral psoriasis is a rare clinical variant of plaque psoriasis with unclear pathogenesis. We report a 51-
year old woman with a 5-year history of itchy, red, scaly patches on the unilateral right breast, arm, and leg.
There were also some vegetating masses on top of the red patches on her lower right leg. Physical
examination revealed multiple erythematous plaques with coarse-white scales overlying it, distributed along
Blaschko lines on her right side of the body and multiple verrucous nodules on erythematous plaques on her
lateral aspect of lower right leg. Histopathology examination showed epidermal psoriasiform hyperplasia
and collections of neutrophils. Numerous koilocytes were also seen. Qualitative Human Papillomavirus
(HPV) genotyping test was done on lesion on the leg and the result was positive. The diagnosis of unilateral
psoriasis with verruca vulgaris was made based onclinico-histopathological findings. To date, there is no
guideline available for unilateral psoriasis. She was treated with topical steroid and 5% LCD in vaseline
album for psoriasis and 30% salicylic acid in vaseline album for verruca vulgaris and reported
improvement. In this case, HPV infection occurs simultaneously. Theoretically, psoriasis lesions are
resistant to infection. On the other hand, various microorganisms, including viruses, are known to be
associated with exacerbations of psoriasis and HPV infection is considered an opportunistic
infection.Unilateral psoriasis with verruca vulgaris is a very rare case. Recognition of this unusual clinical
picture of psoriasis variant with overlapping verruca vulgaris is necessary to avoid delayed diagnosis and
perform prompt treatment.
1 INTRODUCTION
Psoriasis is a chronic, immune-mediated disorder
with a various predisposition combined with
environmental triggers, for example trauma,
infections, medications, and psychological
stress.(Yan de Kerkhof et al., 2018)The lesion is
characterized by sharply demarcated erythematous
plaque with coarse-micaceous scale. The plaque may
be localized or widespread in distribution with
predilection in scalp, elbows, knees, hands, feet,
trunk, and nails. Yan de Kerkhof et al.,
2018;Gudjonsson et al., 2012)
The occurrence of psoriasis in a linear or
unilateral orsegmental along the lines of Blaschko is
very rare.(Nasimi et al., 2016;Ghoneim et al. 2017).
Considerable diagnostic confusion exists, since these
lesions can clinically resemble very closely to other
linear dermatoses such as inflammatory linear
verrucous epidermal nevus (ILVEN). The
pathogenesis of unilateral psoriasis remains unclear,
however genetic mosaicism is proposed to be the
underlying mechanism. (Ghoneim et al. 2017).
To date, there is no treatment guideline
specifically for unilateral psoriasis, so treatment was
based on the algorithm for psoriasis vulgaris.
However, the prognosis is not very good due to
various inconsistent treatment results and
recalcitrant cases. (Ghoneim et al. 2017).
Psoriasis can be provoked or exacerbated by a
variety of different environmental factors, including
viral infections, such as papillomaviruses and
retroviruses. (Fry L et al., 2007). Nevertheless, the
incidence of overlapping psoriasis and verruca
vulgaris cases are extremely rare. During 2016-
2018, there was only one case of unilateral psoriasis
and verruca vulgaris in Department of Dermatology
and Venereology, Faculty of Medicine Universitas
286
Bianti, M., Yusharyahya, S., Sirait, S., Fitri, E. and Novianto, E.
A Rare Case of Unilateral Psoriasis with Verruca Vulgaris: Challenges in Diagnosis and Treatment.
DOI: 10.5220/0009986902860289
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 286-289
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Indonesia/Dr. Cipto Mangun kusumo National
Central General Hospital. (Data Kunjungan Pasien
Poliklinik Kulit dan Kelamin RSUPN Cipto Mangun
Kusumo Divisi Alergi - Imunologi, 2016-2018). We
report a rare case of unilateral psoriasis with verruca
vulgaris. The aim of this case report is recognition of
this uncommon psoriasis variant with overlapping
HPV infection to avoid delayed diagnosis and
perform prompt treatment.
2 CASE
A 51-year-old woman with no past medical history
presented with itchy, red, scaly patches on the
unilateral right breast, arm, and leg. She came to our
clinic on July 19
th
2018 with chief complaints of red,
scaly patches on her right side of the body, started
on her right lower leg, accompanied by itch, which
she felt very bothersome, since 5 years ago.
She had not seek medical treatment for this
condition and self-treated with application of cajuput
oil, engine lubricant oil, and several over-the-
counter ointments for itch. She also soaked her leg
with hot water and scratch the lesions to alleviate the
itch. Sometimes she used tools, such as comb, back
of the knife, or stones to scratch. These provide
transient symptomatic relief but the skin lesions
persist.
One year ago, the lesion spread to the right arm
and right lower back. Still, she had not seek medical
treatment and continue the application of previous
oils. Two weeks prior to admission, the lesions
spread to right breast. Patient also complained of a
vegetating mass in her lower right leg. The
vegetating mass was located on the previous
patches. She forgot the time of the onset, but she
noticed enlargement of the mass. There were no itch
or pain reported.
Patient denied any joint pain. No history of
atopic and allergy were recorded on patient, as well
as on her family. There were no history of similar
complaints in family. History of contact with plants
or farming-related were denied. History of contact
with irritants, other than mentioned above, were
denied.
Physical examination revealed multiple,
erythematous plaque, lenticular-plaques in size,
circumscribed, discrete-confluent, with coarse-white
scale overlying it on the right breast, lower right
back, right arm, right leg-foot. The lesions are
unilaterally distributed. There were
onychodystrophy and onychodiscoloration on 1
st
to
5
th
digits of right foot. On her lateral aspect of lower
right leg, we found multiple verrucous nodules on
the top of the erythematous scaly plaques. The Body
Surface Area (BSA) was 8% and the Psoriasis Area
Severity Index (PASI) score was 6.6. The itch was
evaluated with Visual Analog Scale (VAS) and
showed mild itch with score 3-4.
Biopsies from two locations were performed.
The first was from erythematous plaque on patient’s
right breast. Histopathological examination revealed
regular acanthosis, column of parakeratosis,
orthokeratosis, and collections of
neutrophilsbeneaththe stratum corneum (Munro
microabcesses). In the dermis, infiltration of
lymphocytes was seen. These findings were
according to psoriasis. The second location is from
her right lower leg. The lesion was verrucous nodule
with granulation tissue. In the epidermis, seen
parakeratosis, crust, acanthosis with elongated rete
ridges, some rete ridges were seen arborizing.
Spongiform pustules and numerous koilocytes were
seen. In the dermis, seen some chronic inflammatory
cells. Qualitative HPV genotyping test was done on
lesion on the leg and the result was positive,
indicating the presence of HPV infection
concomitantly with psoriasis.
The diagnosis of unilateral psoriasis with verruca
vulgaris was made based on clinic-histopathological
findings. She was treated with 0.25%
desoximethasone ointment and 5% LCD in vaseline
album for psoriasis and 30% salicylic acid in
vaseline album for verruca vulgaris. She has not
come for follow up yet but reported mild
improvement in her skin lesions.
A Rare Case of Unilateral Psoriasis with Verruca Vulgaris: Challenges in Diagnosis and Treatment
287
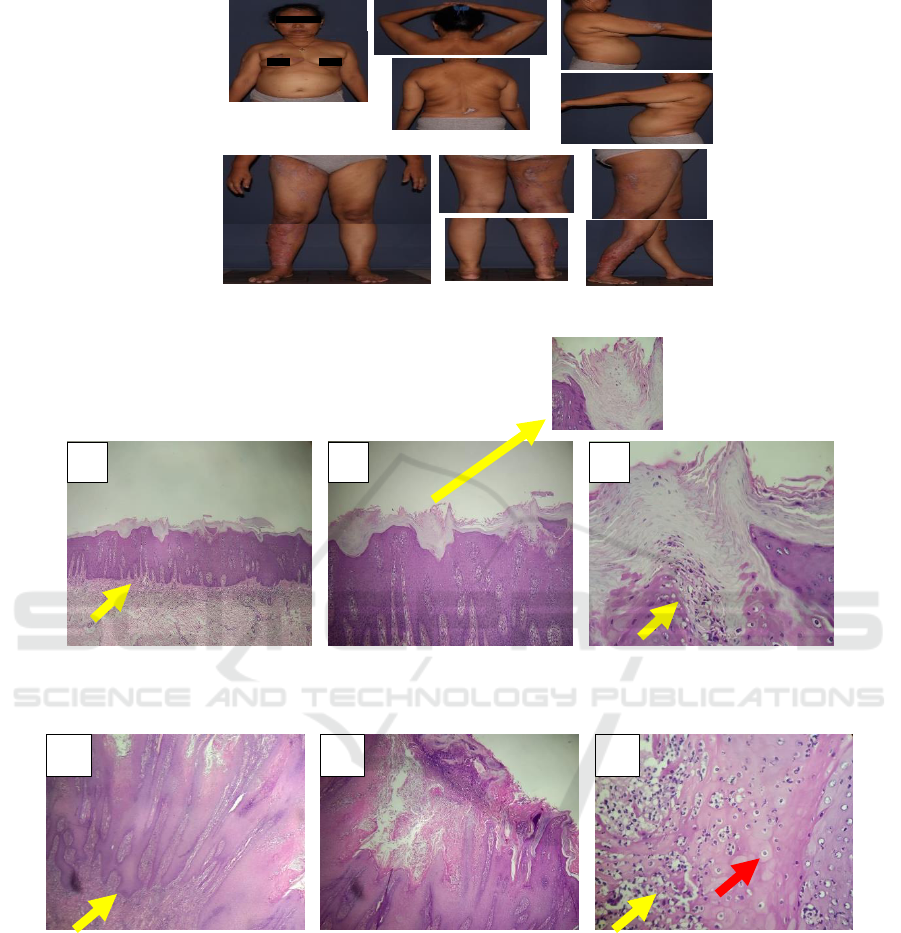
Figure 1.Clinical manifestation in patient
Figure 2.Histopathology findings from erythematous plaque on right breast. (Pointed by yellow arrow) A. regular
acanthosis B. column of parakeratosis C. collections of neutrophils (Munro microabscesses)
Figure 3. Histopathology findings from verrucous nodules on right lower leg. (Pointed by yellow arrow) A. acanthosis with
arborizing elongated rete ridges B. acanthosis with arborizing elongated rete ridges C. collections of neutrophils (Pointed by
yellow arrow) andkoilocytes (pointed by red arrow)
3 DISCUSSION
Unilateralpsoriasis is a rare form of psoriasis
which characterized by typical psoriasis lesion but
only unilaterallydistributed. Case reports of this
variant of psoriasis are still scarce and the
pathogenesis remains unclear although genetic
mosaicismwas suggested to be the cause. (Ghoneim
et al. 2017).Occurrence of psoriasis in a linear or
unilateral distribution raised diagnostic confusion,
since these lesions can clinically resemble other
linear dermatoses.
The main differential diagnosis is ILVEN which
shows similar distribution. (Altmant et al., 1971)
described the diagnostic criteria of ILVEN: early
onset, predominance in women, prevalence in the
lower extremity, pruritus, and recalcitrance to
A
B
C
B
A
C
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
288

treatment. Histopathology examination in addition to
the clinical characteristics to some degree could help
to distinguish between these two entities. In some
cases, if they share the same histology findings, a
definite diagnosis can be made only with meticulous
history taking, detailed clinical examination and
follow-up to observe treatment result (Gudjonsson et
al., 2012;Saraswat A. et al., 2004). Late onset of
erythematous and scaly plaques with quite rapid
progression and involvement of nails, and a response
to antipsoriatic treatment indicate psoriasis in this
case.
Patient was initially suspected with
chromoblastomycosis because of the lesions on her
lower right leg (verrucous nodules on erythematous
plaques) mimicked subcutaneous mycoses infection.
There were no history of contact with plants or
penetrating injury, such as a thorn prick, and the
histopathology findings showed no muriform bodies.
Therefore, chromoblastomycosis could be excluded
from our differential diagnosis.
Histopathology examination was performed to
confirm the diagnosis. Two specimens were taken,
the first was from patient’s right breast and the
findings were according to psoriasis. The second
specimen was taken from patient’s right leg and
interestingly, numerous koilocytes were seen. This
finding was according to psoriasis with verruca
vulgaris. To establish the diagnosis even further,
qualitative HPV genotyping was done and the result
was positive, indicating HPV infection
concomitant with psoriasis lesions. Theoretically,
psoriasis lesions are resistant to infection due to high
production of antimicrobial peptides and interferon
gamma. On the other hand, various microorganisms,
including viruses, are known to be associated with
exacerbations of psoriasis. HPV infection of
keratinocytes is favored by epidermal proliferation,
it could be argued that infection is secondary to the
hyperproliferative process in psoriasis and represents
a type of opportunistic infection.(Fry L et al., 2007).
In addition, patient’s habit to manipulate lesions by
scratching due to the itch may cause trauma that
became port d’entrée of HPV infection.
To date, there are no specific guideline for
unilateral psoriasis. Treatment options were based
on the algorithm for psoriasis vulgaris and some of
the cases showed unresponsiveness. The patient was
treated in accordance with treatment algorithm from
Indonesian PsoriasisStudy Group. Patient was
classified as moderate psoriasis and received topical
treatment with 0.25% desoximethasone ointment
and 5% LCD in vaseline album. We didn’t perform
phototherapy because it may further worsen the
verruca vulgaris. Segmental manifestations of
psoriasis respond less favorably to systemic
therapies. The chronicity and resistance to
antipsoriatic agents were suggested to be in part due
to the loss of heterozygosity in cells where the
lesions occur.
4
As for the verruca vulgaris, 30%
salicylic acid in vaseline album was prescribed. She
has not come for follow up yet but reported mild
improvement in her skin lesions, particularly lesions
on her right leg.
4 CONCLUSION
Unilateral psoriasis with verruca vulgaris is a very
rare case. We report a 51-year old woman with a 5-
year history of itchy, red, scaly patches on the
unilateral right breast, arm, and leg. Over the
following year there were also some vegetating
masses on top of the red patches on her lower right
leg. The diagnosis of unilateral psoriasis with
verruca vulgaris was made based on clinico-
histopathological findings. The patient was treated in
accordance with treatment algorithm for psoriasis
vulgaris from Indonesian Psoriasis Study Group. She
was treated with topical steroid and 5% LCD in
vaseline album for psoriasis and 30% salicylic acid
in vaseline album for verruca vulgaris and reported
improvement.
REFERENCES
Altman J, Mehregan. 1971A. Inflammatory linear
verrucose epidermal nevus.Arch Dermatol.;104:385-9.
Data KunjunganPasienPoliklinikKulitdanKelamin RSUPN
CiptomangunkusumoDivisiAlergi-ImunologiTahun.
2016-2018.
Fry L, Baker BS.2007.Triggering psoriasis: the role of
infections and medications. Clin Dermatol; 25:606-15.
Ghoneim S, Ramos-Rodriguez AJ, de Lara FV, Bonomo
L. 2017.The successful treatment of a case of linear
psoriasis with ixekizumab. Case Rep Dermatol
Med;3280215.
Gudjonsson JE, Elder JT. Psoriasis. In: Goldsmith LA,
Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K,
Eds. Fitzpatrick's.2012.Dermatology in General
Medicine. 8
th
Ed. New York: McGrawHill; p.197-231.
Nasimi M, Abedini R, Azizpour A, Nikoo A.2016.
Isolated linear blaschkoid psoriasis. ClinExpDermatol;
41:775-8.
Saraswat A, Sandhu K, Shukla R, Handa S.2004.
Unilateral linear psoriasis with palmoplantar, nail, and
scalp involvement. PediatrDermatol;21:70-3.
van de Kerkhof PCM, Nestle FO. 2018. Psoriasis. In:
Bolognia JL, Schaffer JV, Cerroni L. Eds.
Dermatology. 4
th
Ed. Philadelphia: Elsevier. p.138-59.
A Rare Case of Unilateral Psoriasis with Verruca Vulgaris: Challenges in Diagnosis and Treatment
289
