
Corticosteroid Pulse Therapy for the Treatment of Bullous Systemic
Lupus Erythematosus with Lupus Nephritis
Hayra Diah Avianggi
1*
, Intan Nurmawati
1
, Radityastuti
1
, Widyawati
1
, Meira Dewi Kusuma
2
1
Departmentof Dermatovenereology, Faculty of Medicine, Diponegoro University /
dr. Kariadi General Hospital, Semarang
2
Department of Pathology Anatomical, Faculty of Medicine, Diponegoro University /
dr. Kariadi General Hospital, Semarang
*Corresponding author
Keywords: Bullous systemic lupus erythematosus, SLICC criteria, corticosteroid pulse therapy, lupus nephritis
Abstract: Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease. Skin involvement occurs in
nearly 76 % of all lupus patients. The Bullous Systemic Lupus Erythematosus (BSLE) is a rare cutaneous
variant of SLE, affecting in less than 1%. A26-year-old female with a history of a vesiculobullous eruption
on face, neck, trunks, andarms, along with oral mucosa ulcers.She hadphotosensitivity, a non-scarring
alopecia, hemolytic anemia, serositis, arthralgia, renal impairment, and high antibody titers confirmingSLE.
Histopathologicalexamination showed features in accordance with SLE, tends to beBSLE. The renal biopsy
confirmed the features of lupus nephritis. The patient was diagnosed as BSLE based on the Systemic Lupus
International Collaborating Clinics (SLICC) criteria, location of a blister, and histopathologicfinding. She
responded well to systemic corticosteroid pulse therapy. BSLE should be considered as a differential
diagnosis among patients with bullous lesions.It is vital to prevent the complication of SLE, that is lupus
nephritis because it relates to a worse prognosis. We choose corticosteroid given as pulsed therapy to
enhance the therapeutic effect and reduce the side effects, followed by azathioprine as sparing agent.
Systemic corticosteroid pulse therapy is considered as first-line therapy, with azathioprine which has been
proved to be effective in maintaining disease remission. The objectiveof BSLE therapy is to prevent new
blisters, promote healing, and prevent scarring.Prognosis ad vitamdubiaadbonam, ad sanamdubiaadmalam,
ad cosmetic dubiaadbonam.
1 INTRODUCTION
The systemic lupus erythematosus (SLE) is a
multisystem autoimmune disease. The bullous
systemic lupus erythematosus (BSLE) is a rare
cutaneous variant of SLE, accounts less than 1%.
BSLE is an autoantibody-mediated vesiculobullous
disease in patients with SLE (Chen et al, 2015). The
etiology of BSLE is unclear (Contestable et al,
2014). In the USA there is an association between
SLE with HLA-DR2 (Wojnarowska et al, 2010;
James et al, 2016). BSLE usually manifests in the
second and third decades of life, most frequently in
black women (Momen et al, 2016). If there is a
bullous eruption, we have to consider BSLE as a
differential diagnosis. Multiple case reports show
that BSLE can be the initial presentation of SLE
(Contestable et al, 2014; Momen et al, 2016). Here
in we report a case of BSLE treated with
corticosteroid pulse therapyas an alternative therapy
to Dapsone.
2 CASE
A 26-year-old female was admitted to emergency
department Dr. Kariadi General Hospital with a 1-
week history of a progressive non-itching blistering
eruption, erosion and crust around the face, neck,
trunks, and arms. She also complained of diffuse
hair loss, moderate fever, and arthralgias for the last
three months. Bullae have appeared on the sun-
exposed areas with the erythematous base while
those on the arms had a clear base. There were
histories of malar rash after sun exposure and
conjunctivitis on the right eye. She has never had
Avianggi, H., Nurmawati, I., Radityastuti, ., Widyawati, . and Kusuma, M.
Corticosteroid Pulse Therapy for the Treatment of Bullous Systemic Lupus Erythematosus with Lupus Nephritis.
DOI: 10.5220/0009988803570361
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 357-361
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
357
any seizure, psychosis, and history of blistering
lesions before. She was not taking any drugs and
never had a drug allergy. There is no family member
with the same complaint. She weighed 42 kg with a
height of 150 cm. Clinical examination revealed
poor nutritional status with moderate pallor, bilateral
pitting pedal edema with facial puffiness, and
temperature (37.8°C). Her pulse rate was 92/min,
Blood pressure was 110/70 mmHg, and respiration
rate was 20/min. There was no enlargementon liver,
spleen, and lymph node. The anogenital regions
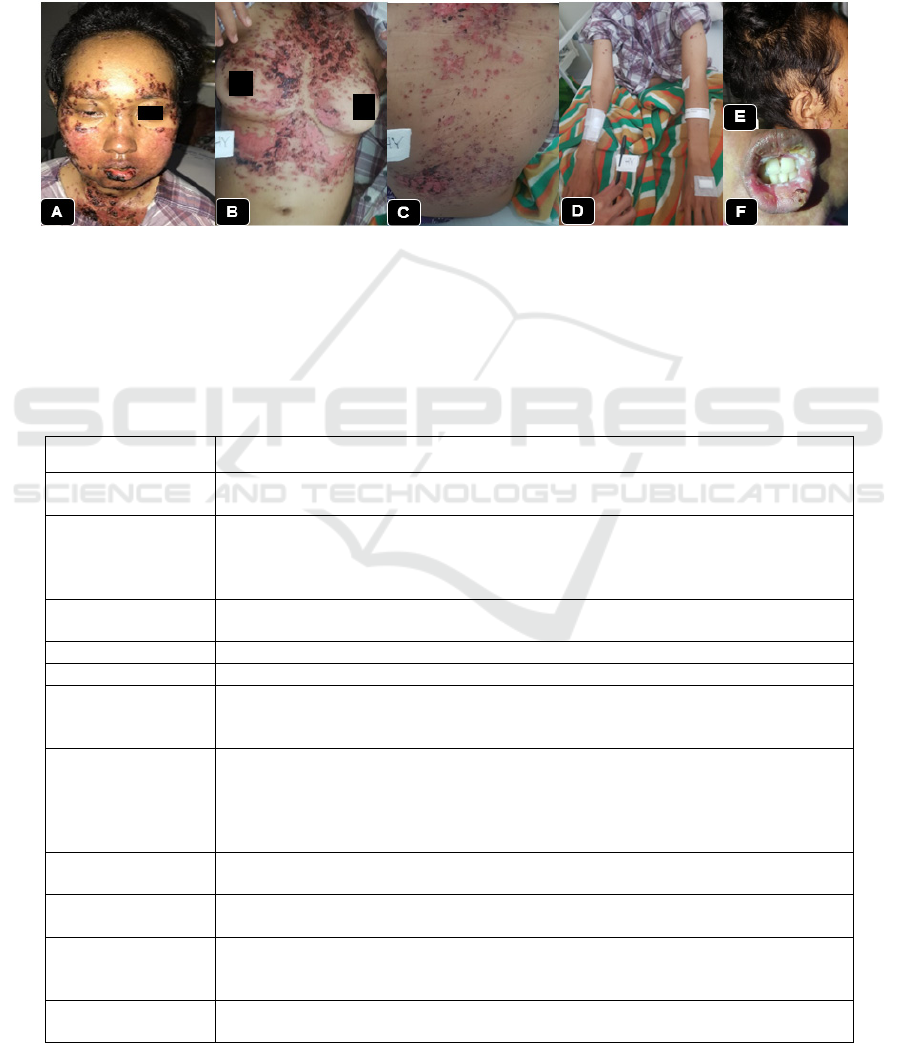
were spared. The dermatologicexamination
demonstrated erosion and crusts on face, neck,
trunks, and arms (Figure.1 A, B, C, D).Diffuse hair
loss (Figure.1 E). Curdy white discharge was seen
over the oral ulcers (Figure.1 F).
Figure 1. A. Erosion and crusts on the face, conjunctivitis on right eye (B, C, D) Erosion and crusts on the neck, trunks, and
arms,E. Diffuse hair loss,F. Oral ulcers, and crust.
Based on the anamnesis and physical
examination, there were several differential
diagnoses: bullous systemic lupus erythematosus
(BSLE) andpemphigus erythematosus with SLE
(Senear-Usher syndrome). She was referred to the
Department of Nephrology for kidney
biopsy.Laboratory examination shows (Table.1).
Table.1. Laboratory examination
EXAMINATION RESULT
Hematology
- Haemoglobin 8,5 g/dL, increase RDW 16,4%
- Leukopenia 3,7x10
3
/UL, lymphopenia 3%
Blood
Biochemistry
- Increased serum creatinine 2,08 mg/dl and (Duplo test)
- Increased serum ureum 188 mg/dl (Duplo test).
- Creatinine clearance 30ml/min. Hypoalbuminemia (2,4 g/dl)
- Random Glucose Test (GDS), SGOT and SGPT within normal limits
Peripheral blood
smear
- Anisocytosis, poikilocytosis (ovalosit, pearshape, teardrop, burr cell).
Chest X-RAY
- Cardiomegaly (LV, LA)
ECG
- Pericardial effusion with LvH concentric, no features of Myocarditis
USG
- Pleura effusion sinistra
- Bilateral cortical echogenicity increased, suggestive of renal parenchymal disease
(Brenbridge 1).
Urine Routine
- Proteinuria 15mg/dl, Reduction 500mg/dl
- Leukocyte sediment 232,1/ul, leukocyte 25-30 LPB, glitter cell (+), cylinder
3,22/ul, hyaline cylinder 3,5 /ul
- Yeast cell 82,3/ul.Bacteria 7177,6/ul (++).
- Urinesbach 0 g/L volume 350 cc in 24 hour
Immunology test
- Serum anti-nuclear antibodies (ANA) 268,7 unit (> 60 positive)
- Anti double-stranded DNA (Anti dsDNA) 1098 IU/ml (> 300 Positive)
Serologic test
- Venereal Disease Research Laboratory (VDRL), HBsAg, and Human
immunodeficiency virus (HIV) were negative. CD4: 137.
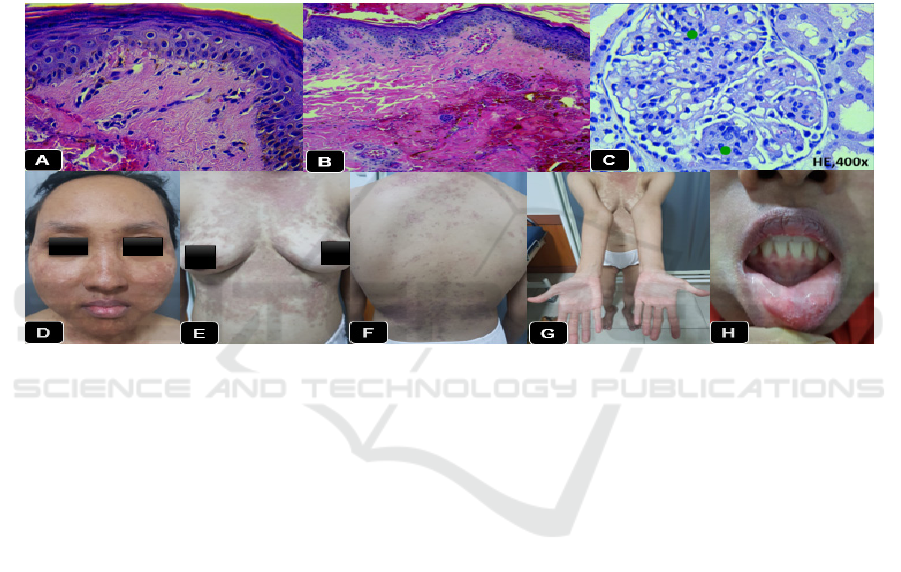
Histopathology
examination
- Granulosis, spongiosis, and degeneration vacuolar(Figure 2A).
- Fibrous stromascattered with lymphocytes, histiocytes, perivascular in the
papillary dermis(Figure 2B).
Kidney biopsy
- Diffuse Lupus Nephritis Class IV of ISN/RPS 2004 classification with an active
lesion (Figure 2C).
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
358
Based on anamnesis, physical examination, and
laboratory examination, the patient was diagnosed as
Bullous systemic lupus erythematosuswith lupus
nephritis and oral thrush. The patient was managed
with methylprednisolonepulse therapy 500mg/day
(equivalent to prednisone 15 mg/kg/day) IV for three
consecutive days, followed by half adjusting dose
every three days until 32 mg/day orally (equivalent
to prednisone 1 mg/kg/day) for one week.
Azathioprine was started with 50 mg once daily
peroral, ranitidine 150 mg twice a day IV, and
systemic broad-spectrum antibiotics (ciprofloxacin)
500 mg twice a day, folic acid 1 mg once daily. The
lesion was soaked with 0.9% NaCl for ± 15 minutes
before the use of fusidic acid cream and silver
sulfadiazine cream twice a day to erosions and
crusts, nystatin drop 100,000 UI, 1cc / 8 hours for
lesions in the oral cavity and triamcinolone
acetonide in orabase. The results of the therapy are
quite satisfactory. The patient is also given a whole
blood transfusion to treat anemia. The patient was
referred to Department of Nephrology for the
treatment of lupus nephritis, and she was put on
cyclophosphamide and lisinopril. She was
discharged with no new skin lesions after 20
days.(Figure 2 D,E,F,G, H).
Figure 2. A.The epidermis, granulosis, spongiosis and degeneration vacuolarB. Dermis; subepidermalvesiculation, fibrous
stromascattered with lymphocytes, histiocytes and perivascular inpapillary dermisC. Diffuse Lupus Nephritis Class IVD, E,
F, G. Hyperpigmentedmacula on the face, neck, trunks, and arms H. No sign of oral ulcers
The patient was advised to visit a dermato-
venereology clinic every two weeks to monitor side
effects due to the long-term of topical and systemic
corticosteroids, to do periodic blood, urine and
serology tests, and to always use a sunscreen with
SPF ≥30, 20 minutes before sun exposure.
3 DISCUSSION
The bullous systemic lupus erythematosus (BSLE) is
a rare autoimmune blistering disorder that typically
manifests as a vesiculobullous eruption in a patient
with SLE.(Contestable et al, 2014) Clinically, BSLE
is characterized by rapid onset of widespread, tense,
clear or hemorrhagic fluid containing vesicles to
bullae which rupture spontaneously resulting in
erosions and crusts. These blisters are distributed
over the neck, face, trunks, and extremities.The
occurrence of blisters on the healthy skin should
always arouse suspicion of BSLE. (Chen et al, 2015)
The diagnostic criteria of BSLE were first
described by Camisa and Sharma in 1983 and were
revised in 1988. These criteria were (1) diagnosis of
SLE based on ACR criteria; (2) vesicles and/or
bullae; (3) The histopathology is characterized by
subepidermal bullae with microabscesses of
neutrophils in the dermal papillae; (4) DIF with IgG
and/or IgM and often IgA at the BMZ; and (5) IIF
testing that can be negative or positive for
circulating autoantibodies against the BMZ via the
salt-split skin technique. (Contestable et al, 2014)
The American College of Rheumatology
(ACR) revised criteria for SLE in 1997, which were
recently validated by the Systemic Lupus
International Collaborating Clinic (SLICC) group in
2012 that results in higher sensitivity with equal
specificity (Table 2).(Kuhn et al, 2015)
Corticosteroid Pulse Therapy for the Treatment of Bullous Systemic Lupus Erythematosus with Lupus Nephritis
359
Table 2. Classification of SLE based on the Systemic Lupus International Collaborating Clinic (SLICC) Criteria,
and case
Classification of SLE: The Systemic Lupus International
Collaborating Clinic (SLICC) Criteria
Case
Clinical criteria
- The acute cutaneous lupus erythematosus (butterfly rash)
- The chronic cutaneous lupus erythematosus (discoid LE)
- Oral ulcers
- Non-scarring alope
cia
- Synovitis (≥ 2 joints) or tenderness on palpation (≥ 2 joints)
and morning stiffness (≥ 30 minutes)
- Serositis (pleurisy / pericardial pain for > 1 day)
- Renal involvement (single urine: protein/ creatinine ratio/24-
hour urine protein >0,5g)
- Neurological involvement (seizures, psychosis)
- Hemolytic anemia
- Leukopenia (<4000/µL) or lymphopenia (<1000/µL)
- Thrombocytopenia (<100.000/µL)
Clinical criteria
- Butterfly rash positive
- Negative
- Oral ulcers positive
- Positive, 3 months ago
- Arthralgia (ankle, interdigital)
- Pericardial and pleural effusion
- Proteinuria 15 mg/dl and Creatinine
clearance 30 ml/min.
- Negative
- Anemia normositiknormokrom
- Leukopenia 3,7x10
3
/UL
- Within normal limits
Immunological criteria
- ANA level; above laboratory reference range
- Anti-dsDNA antibodies
- Anti-sm antibodies
- Antiphopolipid antibodies (anticardiolipin and anti-β2-
glycoprotein I antibodies, false-positive VDRL test
- Low complement (C3, C4, or CH50)
- Direct coombs (in the absence of hemolytic anemia)
Immunological criteria
- ANA 268,7 unit (Positive > 60)
- Anti dsDNA 1098 IU/ml (Positive >
300)
- No examination
- VDRL negative
- No examination
- No examination
(References: The Diagnosis and Treatment of Systemic Lupus Erythematosus)
According to the SLICC rule, the patient must
manifest at least four criteria (including at least one
clinical criterion and one immunologic criterion) or
must have biopsy-proven lupus nephritis in the
presence of either ANAs or anti-dsDNA antibodies
(Contestable et al, 2014; Kuhn et al, 2015)
Thehistopathological section in trunks erosion
showed old lesion, and the feature view shows a
central focus of degeneration vacuolar,
subepidermalvesiculation, striking inflammatory
changes outline the dermal vasculature. This is in
accordance with the other features of BSLE(Calonje
et al, 2012). Skin biopsy report only to corroborate
our clinical impression and to form our final
diagnosis. (Momen et al,2016)
Differential diagnosis of BSLE is pemphigus
erythematosus with SLE (Senear-Usher syndrome).
Senear-Usher syndrome can be ruled out because it
is an autoimmune condition where there is overlap
between the clinical and immunological features of
pemphigus erythematosus and lupus erythematosus,
include like scattered scaly flaccid blisters with
erosions and crusts on ‘seborrhoeic’ areas along with
malar rash, absence of mucous membrane
involvement. ANA test is negative or weakly
positive. Histopathological showedacanthotic
epidermis with large subcorneal blisters.(Amatya et
al,2017)
Dapsone is the initial treatment of choice for
BSLE. (Contestable et al, 2014) The mechanism of
actionmainly relies upon its inhibition of the
functions of PMN leukocytes and of complement
activation via the alternative pathway that has been
postulated. (Chen et al, 2015) We didn't choose
dapsone due to patient‘s hemolytic anemia and its
unavailability in our facility. A corticosteroid may
be active in patients who cannot tolerate dapsone,
have an inadequate response to dapsone, or require
treatment of concurrent systemic manifestations of
systemic lupus erythematosus. (Visser et al, 2017)
Based on recommendations of GRh (German
Society of Rheumatology) where corticosteroids as
first-line therapy, begin with methylprednisolone
500–750 mg iv on three consecutive days (level of
evidence 3, the strength of statement C); then per os
0.5 mg/kg body weight/day for four weeks with
subsequent tapering.
6
Corticosteroid pulse therapy
means it refers to treatment with more than 250 mg
prednisone or its equivalent per day, for one or more
days.The effects of corticosteroid pulse therapy
appear to include downregulation of activation of
immune cells and proinflammatory cytokine
production, leading to reduced expression of
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
360

adhesion molecules and reduced movement of
neutrophils into sites of inflammation. (Visser et al,
2017;Panat,2012) On this patient, we used
methylprednisolone intermediate-acting with a low
tendency to induce sodium and water retention.
When decreasing corticosteroid doses, treatment
with a sparing agent (azathioprine) regimen
begins..(Visser et al, 2017) The aim of corticosteroid
pulse therapy is getting quicker and stronger efficacy
and decreasing the need for long-term use of
steroids. (Panat,2012)
Azathioprinehas proved to be effective in
maintaining disease remission. (Chen et al, 2015) It
is a purine analog that inhibits the nucleic acid
synthesis and affects both cellular and humoral
immune functions. The drug is transformed to 6-
mercaptopurine (6-MP) and then to its active
metabolites, thiocyanic and thioguanine acid (6
TGN), which incorporate into DNA, thereby causing
DNA/protein crosslinks and interfering with nucleic
acid structure. The daily dose is 1 - 2.5 mg/kg.
Regular monitoring of complete blood counts and
liver function tests is required during therapy.(Visser
et al, 2017)
Prognosis of this patient was ad
vitamdubiaadbonam, ad sanamdubiaadmalam, ad
cosmetic dubiaadbonam. The course of BSLE is
often remitting. The disorder frequently resolves
spontaneously in less than one year. BSLE is an
autoimmune disease that tends to relapse. In some
cases, post-inflammatory hypopigmentation may
remain. The development of BSLE in patients with
SLE does not typically lead to increased mortality.
Morbidity depends on the extent of the eruption and
the response to therapy.(Chen et al,
2015;Contestable et al, 2014; Kuhn et al, 2015).
4 CONCLUSION
BSLE should be considered as a differential
diagnosis of patients with bullous lesions.
Differentiation between BSLE and other blister
disease is vital to prevent further complications of
SLE that may coexist. Corticosteroid pulse therapy
proved can be given as an alternative to Dapsone in
BSLE with nephritis lupus.
REFERENCES
Amatya B, Mm AS, Maharjan L. 2017. Dermatology Case
Reports Pemphigus Erythematosus in a Middle Aged
Nepali Male : Case Report and Literature Review.
2(1):2–4.
Calonje Eduardo; Brenn Thomas; Lazar Alexander;
McKee Phillip, editor. 2012. Of the Skin. In: McKEE’s
Pathology Of The Skin With Clinical Correlations.
Fourth. British: Elsevier Saunders. p. 99–150.
Chen J, Zhong S, He Y, Wang Y, Shi G, Duan L, et
al. 2015. Treatment of Bullous Systemic Lupus
Erythematosus. J Immunol Res.m. 2015:1–6.
Contestable JJ, Edhegard KD, Meyerle JH. 2014.
Bullous Systemic Lupus Erythematosus: A
Review and Update to Diagnosis and Treatment.
Am J Clin Dermatol. 15(6):517–24.
James W, Berger T, Elston D NI. 2016. Connective
Tissue Disease. In: Andrews’ Diseases of The
Skin Clinical Dermatology. Twelfth. USA. p.
153–64.
Kuhn A, Bonsmann G, Anders HJ, Herzer P,
Tenbrock K, Schneider M. 2015. The Diagnosis
and Treatment of Systemic Lupus Erythematosus.
Dtsch Arztebl Int. 112(25):423–32.
Momen T, Madihi Y. 2016. Bullous systemic lupus
erythematosus and lupus nephritis in a young
girl. Oman Med J. 31(6):453–5.
Panat SR, Aggarwal A, Joshi A. 2012. Pulse
Therapy : A Boon or Bane. (May):3–5.
Visser K, Houssiau FA, Antonio J, Silva P. 2017.
Systemic lupus erythematosus : treatment.
Module 18. EULAR.
Wojnarowska, F. Venning V. 2010. Immunobullous
Diseases. In: Tony Burns, Stephen Breathnach
CG ths and NC, editor. Rooks Textbook of
Dermatology Dermatology. eight edit. USA. p.
1895–957.
Corticosteroid Pulse Therapy for the Treatment of Bullous Systemic Lupus Erythematosus with Lupus Nephritis
361
