
Application of Fuzzy Method to Predict Patient's Belief in Doctor
Qualifications
Rudiyanto, Ermi Girsang, Ali Napiah Nasution
Faculty of Medical, Universitas Prima Indonesia, Indonesia
Keywords: Patient Confidence, Doctor Qualifications, Prediction, Fuzzy, Modeling.
Abstract: It was found that the majority of hospitals lately tend to experience a decrease in visits, especially at the
nursery, presumably because some patients are not sure about the practicing doctor. The aim of this study is
to identify factors related to patient belief in practicing doctors. For the data, from 9,919 respondents, 260
samples were used. Data identification using univariate, bivariate with chi-square test, and multivariate with
multiple logistic regression at 95% confidence level ( = 0.05) were selected. The results of the identification
are then modeled using the fuzzy method to predict the patient's confidence in the qualifications of doctors.
The design of the independent variable factor relationship model with the dependent variable of 90% is
achieved. It is hoped that the results of the model prediction will greatly assist management in making policies.
Identification result showed that the factors of doctor reliability, doctor's communication style, and doctor-
patient relationship were the most significant factors (p <0.05) in increasing patient confidence in doctors.
The dominant variable was found in the doctor-patient relationship (having a weight of confidence in the
practicing doctor of 11.1 times higher).
1 INTRODUCTION
An important human resource in a hospital is a doctor.
Doctors are not only needed when sick, but also when
healthy to prevent illness or maintain and improve the
physical and psychological health of a patient.
Patients can choose medical services that suit
themselves (Setyawan, 2017).
In India, over the past decade, a series of failures
in service in the health system, especially in the
medical profession, has caused a great lack of trust in
hospitals and the medical profession. In many low
and middle income countries, the situation is similar
and has reached crisis proportions (Kane & Calnan,
2017).
Some important factors that influence the
selection of medical services as explained by Shaikh
& Hatcher (2004) are: demographic, gender,
economic factors, availability of treatment facilities
and the severity of the disease. Other factors were
also stated by Ahmed (2005), such as; medical costs,
education level, ethnicity, age, and distance of the
patient's residence from the treatment facility.
Sarafino (2006) also added another important factor
was the patient's belief or trust.
Hall, Dugan, Zheng, and Mishra (2001) believe
that belief is the optimism of the patient in a
vulnerable condition where the patient trusts the
doctor for the patient's interests. In medical settings,
belief or trust can be divided into two forms, namely
institutional trust and interpersonal trust. Institutional
trust is trust in medical institutions or systems and
doctors in general, influenced by the media and
institutions related to the health sector, such as the
reputation of hospitals, completeness of
infrastructure, and others. Whereas what is meant by
interpersonal trust is trust in a health provider, such
as a doctor who is built through repetition of
interactions and expectations about behavior,
reliability, kindness (honesty), communication,
physical appearance, empathy from a trusted person
can be tested from time to time (Hall, Dugan, Zheng,
& Mishra, 2001; Pearson & Raeke, 2000).
According to the Indonesian Medical Ethics
Honorary Council (MKEK), a doctor tries to cure a
patient of his illness and restore his health. One way
to cure the disease by a doctor is to cause and
strengthen the patient's confidence and belief that he
can recover. Turning his attention to things that are
hopeful, and optimistic. Psychological / mental state
of the patient must be considered so that an
118
Rudiyanto, ., Girsang, E. and Nasution, A.
Application of Fuzzy Method to Predict Patient’s Belief in Doctor Qualifications.
DOI: 10.5220/0010291001180125
In Proceedings of the International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical (HIMBEP 2020), pages 118-125
ISBN: 978-989-758-500-5
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

explanation of the patient's illness, must be able to
generate confidence that the disease can heal or the
symptoms of the disease can be reduced (MKEK IDI,
2004).
The relationship between a doctor and a patient is
a relationship based on trust, in which the patient
places his belief in his doctor that his illness can be
cured (Guwandi, 2015). Patients' trust in the services
of doctors in hospitals becomes the basis in the
ongoing relationship between health care providers
with patients. A doctor who has a good track record
will attract more patients as consumers because he
believes that the doctor has good quality and can be
trusted for healing his illness (Soetjiningsih, 2016;
Turnip et al, 2020; Wijaya et al, 2019).
The accuracy of the examination carried out by
the doctor will affect the level of patient confidence
in the reliability of the hospital in providing services.
Patients will feel safe and comfortable receiving the
services provided if what they receive is as expected
(Maksum, Maidin, & Anggareni, 2013). This is
consistent with the opinion of Bowers, Swan, &
Kochler (2014) states that in looking at the quality of
health services mentioned factors that determine the
quality of services, namely the ability, skills and
knowledge of officers must be in accordance with
service providers and doctors who are well trained.
This will increase the patient's confidence in the
doctor who handles the disease.
Several previous studies that examined the factors
that influence patient confidence, Djohan's study
(2015) found that the reliability of doctors and
perceived benevolence (operational benevolence) had
a significant positive effect on the confidence of
hospitalized patients in private hospitals in
Banjarmasin. Research conducted by Croker et al.
(2013) found that belief in the doctor was because the
doctor gave the patient enough time, the doctor asked
about the symptoms of the patient's illness, the doctor
listened to the patient, the doctor explained the
examination and treatment, the doctor involved the
patient in the decision about treatment, the doctor
treated the patient with care and attention and the
doctor takes the patient's problem seriously. Another
study by Jiang & Street (2017), that patients' trust in
doctors positively moderate the relationship between
patient activation and doctor-patient communication
online, and between perceptions of health status and
doctor-patient communication online.
Research conducted by Chandra,
Mohammadnezhad, & Ward (2018) on 17 selected
articles from electronic databases including PubMed,
Hinari, Cochrane, Scopus, and Google Scholar
obtained results that in addition to doctor
communication skills, interpersonal care levels and
knowledge about patient illnesses, respect for
patients' illnesses, respect for doctors and care
guarantees increase patient confidence or confidence.
Another study by Gopichandran & Chetlapalli (2013)
in Tamil Nadu, South India found that patients' beliefs
or trust in doctors are influenced by doctor behavior,
perceived comfort levels, personal involvement with
patients, and to a lesser extent by cultural competence
and physical appearance doctor. Based on the results
of some of these studies indicate that the patient's
belief or trust in the doctor is an important concern
and need to know what factors influence the patient's
belief or trust.
The preliminary survey conducted by researchers
interviewed 20 patients who received doctor's
services by asking their beliefs / trust about doctors
practicing their illness or their families showing as
many as 11 people said they were very confident in
their ability, 5 people said they were quite sure, and 4
people said they were not sure . Patients who believe
in the doctor's practice are caused by good doctor's
behavior, friendly, polite communicative. Doctors
understand about illnesses suffered by patients and
family members. The doctor shows empathy to the
patient and looks neat. Conversely, patients who are
not sure say that doctors are not friendly, doctors are
considered less communicative in explaining
illnesses suffered by patients, in addition there are
also some who say that they are not satisfied with the
answers given by practicing doctors when asked by
patients. The patient's beliefs or trust are influenced
by several factors that will be the topic of this
research.
2 METHOD
This type of research was a quantitative analytic study
with a cross sectional study design. This research was
conducted at the Stella Maris Hospital in Medan in
November 2019. The population of the study was
9,919 people, and the samples were 260 people. The
research sampling technique was done by accidental
sampling. The sample in this study was a portion of
the population whose size was taken using the
Lemeshow formula as follows:
2
2
12/1
1)1(
PoPa
PaPaZPoPoZ
n
where, n is the sample size, Z
(1
is the standard
deviation of the alpha for = 0.05 Z = 1,96, Z-
(1
is the standard deviation of beta for = 0,10
Z = 1,282, Po is the proportion of the prevalence of
Application of Fuzzy Method to Predict Patient’s Belief in Doctor Qualifications
119
SC non-medical indications, Pa is the estimated
maternal cesarean section without medical indication,
Pa-Po is the proportion difference of 0.10. Inclusion
criteria used include: Inpatient / Inpatient status the
way, get a doctor's service, can communicate well,
willing to be a respondent, while the exclusion criteria
include not being able to talk (deaf / deaf) and not
willing to be a respondent.
Validity test is used to measure the validity of an
instrument used, meaning that it is able to reveal
what is measured. Validity test was carried out at
Sarah Medan General Hospital 30 patients. The test
conducted is to determine the correlation between
the questions with the total construct score or
variable. A construct is declared valid if there is a
positive and significant correlation. The correlation
value must be greater than 0.361 or the Corrected
Indicator-Total Correlation value in the SPSS output
greater than 0.361 using the Pearson Product
Moment correlation test (Ghozali, 2015). Univariate
data analysis, bivariate using chi-square test, and
multivariate using multiple logistic regression tests
with a confidence level of 95% ( = 0.05).
Soft Computing is a new innovation in building
intelligent systems. This intelligent system is a
system that has expertise like humans in a particular
domain, is able to adapt and learn so that it can work
better in the event of environmental changes. The
basic elements in Soft Computing are: Fuzzy
Systems, Artificial Neural Networks, Probabilistic
Reasoning, Evolutionary Computing.
Fuzzy systems generally consist of 5 steps in
reasoning: Enter fuzzy input, apply the fuzy operator,
apply the implication method, the composition of all
outputs, and defuzifikasi process. Fuzzy logic is an
appropriate way to map an input space into an output
space. For very complex systems, the use of fuzzy
logic (fuzzy logic) is one solution (Kusumandari et al,
2018; Turnip et al, 2018). In general, fuzzy systems
are very suitable for reasoning approaches, especially
for systems that deal with problems that are difficult
to define using mathematical models. For example,
the input values and parameters of a system are less
accurate or unclear, making it difficult to define
mathematical models.
A membership function is a curve that shows the
mapping of data input / output points into their
membership values. One method that can be used to
get membership values is through the function
approach such as triangular, trapesoidal, gaussian,
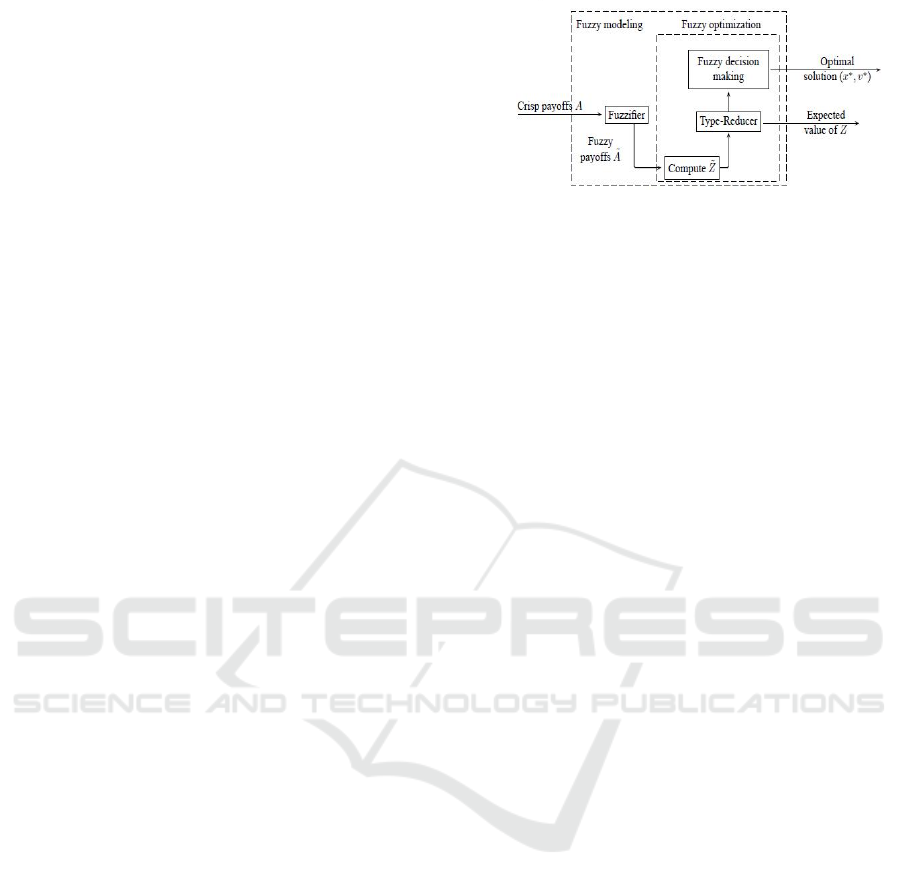
and others. The diagram of fuzzy modeling is shown
in Figure 1.
Figure 1: Scheme of Fuzzy Model
If in a fuzzy system there is a fuzzy rule with
several inputs, then those inputs can be connected
with Zadeh operators, for example AND and OR.
When the inputs in the fuzzy rule are connected using
the AND operator, the degree of membership of the
set of fuzzy outputs is taken from the minimum
degree of membership of the inputs. Conversely, if
the input operator used is the OR function, then the
degree of membership of the fuzzy output set is taken
from the maximum membership degree of the input
fuzzy set (Turnip et al 2018). Besides being formed
based on fuzzy operations on input, the output graph
is cut or scaled using the MIN or DOT implication
function. Furthermore, decisions can be taken
through the defuzzification process.
3 RESULTS AND DISCUSSION
Respondent characteristics include age, sex, last
education, occupation, and reason for the visit. Table
1 shows that the majority of respondents aged <43
years (54.6%), a small proportion aged> 43 years
(45.4%). Based on gender, all respondents were
female (100.0%). Based on education, the majority of
respondents were highly educated (diploma / higher)
(78.5%), a small proportion were middle educated
(high school) (21.5%). Based on work, most
respondents work as entrepreneurs / traders (37.7%),
a small proportion of respondents work as civil
servants (13.0%). Based on the reason for visiting
Stella Maris Hospital in Medan, the majority of
respondents went to the hospital for treatment
(50.8%), a small portion went to the hospital for
control (routine check) (49.2%).
Based on the results of the bivariate analysis
obtained a significant correlation of independent
variables with confidence / trust in lecturers who
practice at RSIA Stella Maris in 2019 namely
physician behavior (p = 0.003), physician honesty (p
= 0.005), physician reliability (p = 0,000), style
doctor communication (p = 0,000), doctor empathy (p
= 0,000), choice recommendations (p = 0,000), and
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
120
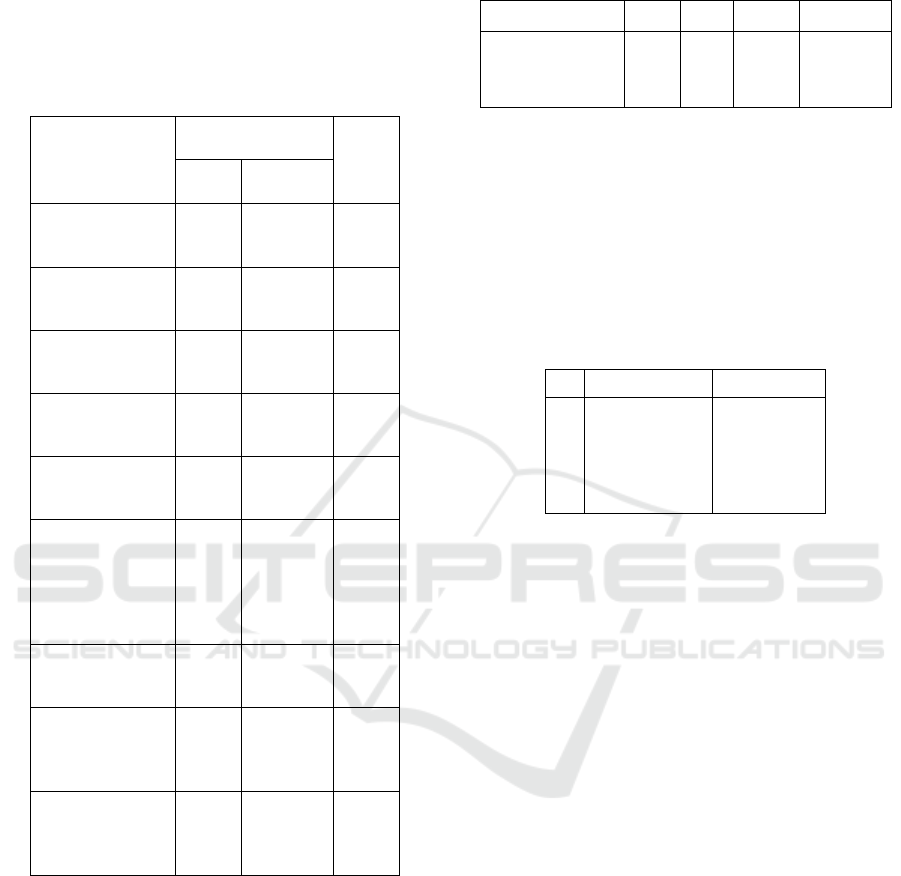
doctor-patient relationship (p = 0,000). Unrelated
variables are gender (0.879), and education (0.582).
The complete Chi-Square statistical test results can be
seen in Table 1.
Table 1: Relationship of Each Independent and Dependent
Variable.
Variables
Patient's Belief /
Trust
p-
value
Believ
e
Unbelieve
Sex:
Male
Female
96
109
27
28
0,879
Education :
Midle
High
46
159
10
45
0,582
Doctor Behavior:
Good
Not Good
176
29
37
18
0,003
Doctor Honesty:
Honest
Not Honest
163
42
33
22
0,005
Doctor reliability:
Reliable
Not Reliable
172
33
22
33
0,000
Doctor's
Communication
Style:
Communicative
Not
Communicative
168
37
31
24
0,000
Doctor Empathy:
Empathy
Not Em
p
ath
y
167
38
31
24
0,000
Recommended
Choice:
Personally
Others
160
45
29
26
0,000
Doctor-Patient
Relationship:
Good
Not Good
170
35
20
35
0,000
The results of multivariate analysis (Table 2) with
multiple logistic regression tests showed that from 7
model candidate variables, only 3 variables were
associated with patients' beliefs / trust in practicing
physicians namely reliability, communication style,
and doctor-patient relationship. The most significant
variable was the doctor-patient relationship variable
which had an Exp (B) / OR value = 11,180 meaning
that the patient who stated the doctor's relationship
with the patient was good, had confidence in the
practicing doctor by 11.1 times higher than the
unfavorable one.
Table 2: Multiple Logistic Regression Test Results
(Significant).
Variabel B Sig. Exp(B)
95%CI for
Exp(B)
Reliability
Communication style
Doctor-Patient
Relationship
Constan
t
2,220
1,750
2,414
-9,979
0,00
0,00
0,00
0,00
9,207
5,753
11,180
4,148-20,437
2,479-13,349
4,978-25,106
The results of the multiple logistic regression tests
also showed variables that were not related to the
beliefs / trust of patients in practicing doctors because
they had a significant value> 0.05, namely behavior
(p = 0.056), honesty (p = 0.110), empathy (p = 0.055)
and choice recommendations (p = 0.051). More can
be seen in Table 3.
Table 3: Multiple Logistic Regression Test Results (not
significant).
No. Variables Si
g
.
(p
-value
)
1.
2.
3.
4.
Behaviour
Honesty
Empathy
Recommended
Choice
0,056
0,110
0,055
0,051
3.1 Doctor Reliability
The results showed that there was a relationship
between physician reliability and patient confidence /
trust in the practice physician, p = 0,000 <0.05.
Reliability variable that has a value of Exp (B) / OR
= 9,207 means that patients who state that doctors
have confidence in doctors who practice were 9.2
times higher than less reliable ones.
Based on the assumptions it was found that
physician reliability was significantly related to
patient confidence / belief. Patients who say that
doctors are reliable tend to feel more confident about
these doctors than patients who state that doctors
were less reliable and feel less sure or lack trust in
doctors. The reliability of the doctor in conducting the
examination was the key to the patient's confidence.
The reliability of doctors was also judged by the
doctor's rapid response in providing services to
patients. In addition, doctors also show readiness to
always serve patients, because by providing the
services that patients want, patients will be satisfied
and confident of the services they receive from
doctors. To increase patient confidence, doctors must
also explain in detail if there are questions raised by
patients. Patients' beliefs also get stronger when the
doctor states there is always for the patient.
Application of Fuzzy Method to Predict Patient’s Belief in Doctor Qualifications
121

3.2 Communication Style
The relationship between doctor's communication
style and patient's belief / trust was found, p = 0,000
<0.05. The doctor communication style variable that
has the value Exp (B) / OR = 5.753 means that
patients who declare communicative doctors have
confidence in doctors who practice 5.7 times higher
than those who are less communicative.
Communication in the process of history taking is
not only done to the patient (auto history taking), but
also to other people who know the patient's disease
history. A significant contribution of the
communication process in the doctor's history to the
patient shows that communication skills were an
absolute requirement for a doctor to get complete
information about the symptoms experienced by the
patient. If a doctor is unable to carry out the
communication process, this inability can result in an
inaccurate diagnosis that is made because information
cannot be extracted from the patient. Communication
delivered in a style that is easy to understand, polite,
relaxed will make it easier for patients to understand
what is delivered by the doctor. Improving the
communication skills of doctors in hospitals must
also be a concern of hospital management because by
establishing good communication between doctors
and patients will be able to create a comfortable
atmosphere and will arise mutual trust, mutual respect
and respect.
According to the researchers' assumptions, this
study proves that the doctor's communication style
was related to the patient's belief / trust. Patients who
state that the doctor has a communicative style of
communication tend to believe in the doctor. The
communication style of the doctor was related to the
style of speaking in a clear voice. When
communicating, provide information to patients and
always smile. Doctors also use language that is easily
understood by patients so that patients feel confident
that the information provided adds to the knowledge
and insight of patients about the disease they are
experiencing. Doctors also act interactively by
inviting patients to ask things that are not understood
or not understood.
3.3 Doctor-Patient Relationship
Based on the results of the study showed that there
was a doctor-patient relationship with the patient's
belief / trust in the doctor, p = 0,000 <0.05. The
doctor-patient relationship variable that has an Exp
value (B) / OR = 11.180 means that the patient who
states that the doctor-patient relationship is good, has
confidence in the doctor practicing 11.1 times higher
than the unfavorable one.
In principle, in the relationship between doctors
and patients there are two important things that must
be considered, namely how doctors place patient
autonomy as individuals, especially in making
medical decisions and how doctors build harmony
through effective communication. During this time
doctors put themselves in medical decisions as a
guardian and the most versatile, so that patient
autonomy has less place.
The results of this study prove that the patient's
doctor relationship is significantly related to the
patient's confidence in the doctor. Patients who state
that a good relationship between the doctor and the
patient makes them believe and trust with the doctor.
According to the majority of respondents surveyed
stated that patients feel familiar with doctors who
examine them especially those who often seek
treatment. This makes the patient feel comfortable
and close to the doctor so that patients do not hesitate
to ask questions related to the disease they are
experiencing. The closeness of the doctor and patient
is caused by the doctor often giving input when the
patient confides about his health condition.
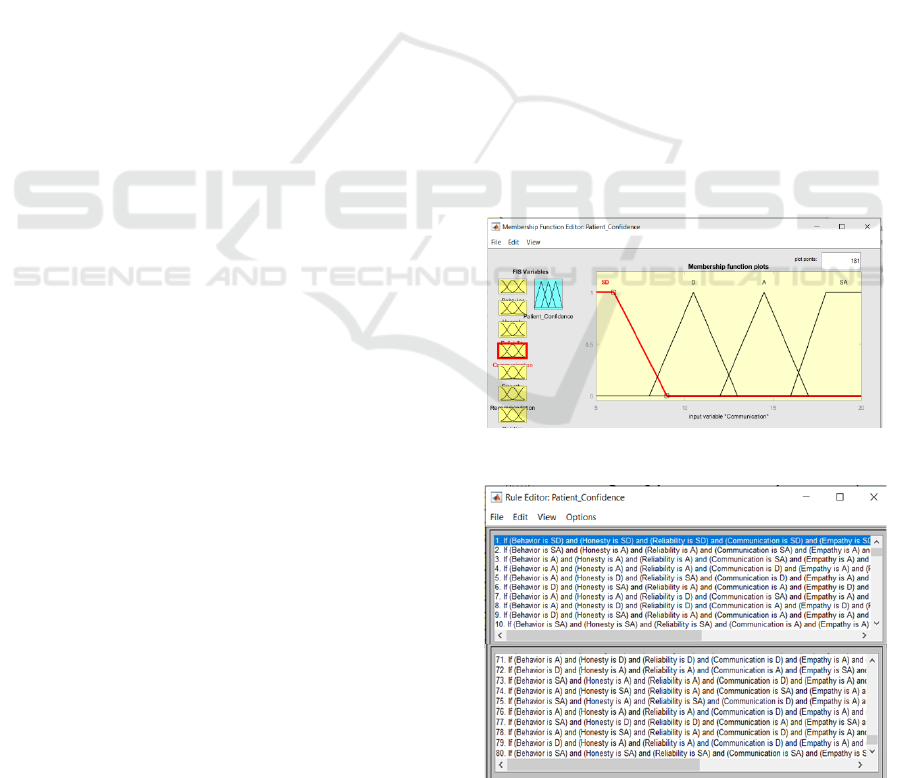
3.4. Fuzzy Model
After the formation of the fuzzy set, the fuzzy rules
are formed. Rules were formed to state the relation
between input and output. Each rule was an
implication. The operator used to connect between
the two inputs is the AND operator, and the one
mapping the input-output is IF-THEN. Propositions
that follow IF are called antecedents, while
propositions that follow THEN are called consistent.
The following are 15 out of 80 built rules in the model
design were:
[R1] IF Behavior is SD AND Honesty is SD AND
Reliability is SD AND Communication style is SD
AND Emapti is SD AND Recommended Choice is
SD AND Patient Doctor Relationship is SD THEN
Patient Confidence in Doctors is SD.
[R2] IF Behavior is SA AND Honesty is A AND
Reliability is A AND Communication Style is SA
AND Emapti is A AND Recommended Choice is A
AND Patient Doctor Relationship is SA THEN
Patient Confidence in Doctors is A.
[R3] IF Behavior is A AND Honesty is A AND
Reliability is A AND Communication Style is SA
AND Emapti is A AND Recommended Choice is D
AND Patient Doctor Relationship is SA THEN
Patient Confidence in Doctors is A.
[R4] IF Behavior is A AND Honesty is D AND
Reliability is D AND Communication style is A AND
Emapti is SD AND Recommended Choice is D AND
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
122
Patient Doctor Relationship is A THEN Patient
Confidence in Doctors is A.
[R5] IF Behavior is A AND Honesty is D AND
Reliability is SA AND Communication style is D
AND Emapti is A AND Recommended Choice is SA
AND Patient Doctor Relationship is A THEN Patient
Confidence in Doctors is A.
[R6] IF Behavior is D AND Honesty is SA AND
Reliability is A AND Communication style is A AND
Emapti is D AND Recommended Choice is D AND
Patient Doctor Relationship is D THEN Patient
Confidence in Doctors is D.
[R7] IF Behavior is A AND Honesty is A AND
Reliability is D AND Communication style is SA
AND Emapti is A AND Recommended Choice is A
AND Patient Doctor Relationship is A THEN Patient
Confidence in Doctors is A.
[R8] IF Behavior is A AND Honesty is D AND
Reliability is D AND Communication style is A AND
Emapti is D AND Recommended Choice is A AND
Patient Doctor Relationship is D THEN Patient
Confidence in Doctors is D.
[R9] IF Behavior is D AND Honesty is SA AND
Reliability is A AND Communication style is A AND
Emapti is A AND Recommended Choice is A AND
Patient Doctor Relationship is SA THEN Patient
Confidence in Doctors is A.
[R10] IF Behavior is SA AND Honesty is SA AND
Reliability is SA AND Communication style is A
AND Emapti is A AND Recommended Choice is A
AND Patient Doctor Relationship is A THEN Patient
Confidence in Doctors is A.
[R11] IF Behavior is SA AND Honesty is A AND
Reliability is D AND Communication style is A AND
Emapti is A AND Recommended Choice is SA AND
Patient Doctor Relationship is A THEN Patient
Confidence in Doctors is A.
[R12] IF Behavior is A AND Honesty is SA AND
Reliability is A AND Communication style is A AND
Emapti is A AND Recommended Choice is A AND
Patient Doctor Relationship is A THEN Patient
Confidence in Doctors is SA.
[R13] IF Behavior is A AND Honesty is SA AND
Reliability is A AND Communication Style is D
AND Emapti is A AND Recommended Choice is D
AND Patient Doctor Relationship is A THEN Patient
Confidence in Doctors is A.
[R14] IF Behavior is SA AND Honesty is SA AND
Reliability is D AND Communication style is A AND
Emapti is A AND Recommended Choice is A AND
Patient Doctor Relationship is SA THEN Patient
Confidence in Doctors is SA.
[R15] IF Behavior is A AND Honesty is A AND
Reliability is A AND Communication style is A AND
Emapti is SA AND Recommended Choice is A AND
Patient Doctor Relationship is SA THEN Patient
Confidence in Doctors is SA.
In the rules, SD is strongly disagree, D is disagree, A
is agree, SA is strongly agree.
Next up toFor training, 30% of the training data
wasused. The input and output design is shown in
Figure 2. Fugure 3 is the capture of the 80 built rules
on fuzzy. Figure 4 is the surface form of the fuzzy
program which shows that if the Behavior value is
12.5 and the Honesty value is 12.5, then the Patient
Confidence value is at 25. Data Test results with
about 100 data training data are used to test the
accuracy of the fuzzy model. Figure 5 is a plot of the
measurement data and fuzzy results. From the test
results obtained a model with an accuracy of 92.82%
(blue is the measured data and orange is fuzzy model
results). From Figure 5 it is noted that accuracy
decreases from data to 41. This is because the data is
the first data recognized by the model. However, the
decrease is still not very significant with the meaning
that the model still managed to predict patient
confidence with an accuracy of 92.82%. Without
having to take measurements at any time, the
management can predict the level of patient
confidence with the next to control the related
variables.
Figure 2: Input and output design.
Figure 3: The capture of 80 rules.
Application of Fuzzy Method to Predict Patient’s Belief in Doctor Qualifications
123

Figure 4: Viewer surface of patient confidence toward
honesty and behaviour.
Figure 5: The comparison of patient confidence obtained
from fuzzy model toward measured data.
4 CONCLUSIONS
The results showed that reliability, communication
style, and doctor-patient relationship were related to
the patient's belief / trust in the doctor. The variable
with the greatest relationship in this study is the
doctor-patient relationship variable which has a value
of Exp (B) / OR = 11,180 which mean patients who
stated that they had a good relationship with the
doctor have an odds of 11,1 times to believe more in
their doctor than those who didn't.
REFERENCES
Ahmed, S. M. (2005). Exploring health-seeking behavior of
disadvantaged populations in rural Bangladesh.
Division of International Health(IHCAR), Department
of Health Public Sciences of Karolinska Institutet.
Bowers, M., Swan, J. E., & Kochler, W. F. (2014). What
Atibutes Determine Quality and Satisfaction With
Health Care Delivery. Health Care Management
Review, Aspen Publisher, Inc, 4(1), 49–55.
Chandra, S., Mohammadnezhad, M., & Ward, P. (2018).
Trust and Communication in a Doctor- Patient
Relationship: A Literature Review. Journal of
Healthcare Communications, 03(03), 1–6.
https://doi.org/10.4172/2472-1654.100146
Croker, J. E., Swancutt, D. R., Roberts, M. J., Abel, G. A.,
Roland, M., & Campbell, J. L. (2013). Factors affecting
patients’ trust and confidence in GPs: Evidence from
the English national GP patient survey. BMJ Open,
3(5), e002762. https://doi.org/10.1136/bmjopen-2013-
002762
Depkes RI. (2005). Indikator Kinerja Rumah Sakit. Jakarta:
Departemen Kesehatan Republik Indonesia.
Djohan, A. J. (2015). Faktor-Faktor yang Mempengaruhi
Kepuasan dan Kepercayaan untuk Mencapai Loyalitas
Pasien Rawat Inap pada Rumah Sakit Swasta di Kota
Banjarmasin. Jurnal Aplikasi Manajemen, 13(2), 257–
271.
Goold, S. D. (2012). Trust, distrust and trustworthiness. J
Gen Intern Med, 17(1), 79–81.
Gopichandran, V., & Chetlapalli, S. K. (2013). Factors
influencing trust in doctors: A community
segmentation strategy for quality improvement in
healthcare. BMJ Open, 3(1), 1–7.
Guwandi, J. (2015). Hukum Medik (Medical Law). Jakarta:
FK Universitas Indonesia.
Hall, M. A., Dugan, E., Zheng, B. Y., & Mishra, A. K.
(2001). Trust in physicians and medical institutions:
what is it, can it be measured, and does it matter?
Milbank Quarterly, 79(6), 13–39.
Hall, M. A., Zheng, B., Dugan, E., Camacho, F., Kidd, K.,
Mishra, A., & Balkrishnan, R. (2002). Measuring
patients’ trust in their primary careproviders. Medical
Care Research and Review, 59(3), 293–318.
Jiang, S., & Street, R. L. (2017). Factors Influencing
Communication with Doctors via the Internet: A Cross-
Sectional Analysis of 2014 HINTS Survey. Health
Communication, 32(2), 180–188.
Kane, S., & Calnan, M. (2017). Erosion of trust in the
medical profession in India: Time for doctors to act.
International Journal of Health Policy and
Management, 6(1), 5–8.
Kusumandari, D., Risqyawan, M., Yazir, M., Turnip, M.,
Darma, A. and Turnip, A., 2018. Application of
convolutional neural network classifier for wireless
arrhythmia detection, Journal of Physics: Conference
Series, Volume 1080 (2018) 012048 doi:
10.1088/1742-6596/1080/1/012048.
Maksum, W., Maidin, A., & Anggareni, R. (2013).
Gambaran Tentang Mutu Pelayanan Dokter
Berdasarkan Persepsi Pasien di Instalasi Rawat Jalan
Rumah Sakit Universitas Hasanuddin Kota Makassar.
Bagian Manajemen Rumah Sakit FKM Universitas
Hasanuddin.
MKEK IDI. (2004). Kode Etik Kedokteran Indonesia Dan
Pedoman Pelaksanaan Kode Etik Kedokteran
Indonesia. Retrieved from
https://luk.staff.ugm.ac.id/atur/sehat/Kode-Etik-
Kedokteran.pdf
Moordiningsih. (2016). Relasi Psikologis Dokter-Pasien
Dalam Layanan Kesehatan : Persepsi, Komunikasi,
Empati Dan Unsur Kepercayaan. Psikologika, 22(11),
85–91.
HIMBEP 2020 - International Conference on Health Informatics, Medical, Biological Engineering, and Pharmaceutical
124

Pearson, S. D., & Raeke, L. H. (2000). Patients’ trust in
physicians: many theories, fewmeasures, and little data.
J Gen Intern Med, 15(1), 509–513.
Rahmulyono. (2015). Konsep Rumah Sakit (Cetakan 1).
Jakarta: Gramedia Pustaka Utama.
RSIA Stella Maris. (2019a). Data Laporan Kinerja RSIA
Stella Maris Medan Tahun 2017-2018. Medan.
RSIA Stella Maris. (2019b). Data Pegawai dan Kunjungan
Rawat Inap di RSIA Stella Maris Medan Tahun 2019.
Medan.
Sarafino, E. P. (2006). Health Psychology (5th editio).
USA: GTS Companies.
Setyawan, F. E. B. (2017). Komunikasi Medis : Hubungan
Dokter - Pasien. BIKKIK FK Unmuh Malang, 1(4), 51–
57.
Shaikh, B. T., & Hatcher, J. (2004). Health Seeking
Behaviour and Health Service Utilization in Pakistan:
Challenging The Policy Makers. Journal of Public
Health, 27(1), 49–54.
Soetjiningsih. (2016). Modul Komunikasi Pasien Dengan
Dokter (Cetakan 2). Jakarta: EGC.
Supranto. (2015). Pengukuran Tingkat Kepuasan
Pelanggan untuk Menaikkan Pangsa Pasar (Cetakan 2).
Jakarta: Rineka Cipta.
Thom, D. H., Ribisl, K. M., Stewart, A. L., & Luke, D. A.
(1999). Further validation andreliability testing of the
trust in physician scale. Medical Care, 37(5), 510–517.
Turnip, A., Andrian, Turnip, M., Dharma, A., Paninsari, D.,
Nababan, T., Ginting, C.N., 2020. An application of
modified filter algorithm fetal electrocardiogram
signals with various subjects, International Journal of
Artificial Intelligence, vol. 18, no., 2020.
Turnip, A., Ilham Rizqywan, M., Kusumandari, D., et al.,
2018. Classification of ECG signal with Support Vector
Machine Method for Arrhythmia Detection, Journal of
Physics: Conference Series, Vol. 970 (2018) 012012
doi: 10.1088/1742-6596/970/1/012012.
Turnip, A., Kusumandari, D., Pamungkas, D., 2018. Drug
Abuse Identification based EEG-P300 Amplitude and
Latency with Fuzzy Logic Calssifier, IEEE International
Conference on Applied Engineering, (ICAE), 3-4 Oct.
2018, DOI: 10.1109/INCAE.2018.8579378.
Wijaya, C., Andrian, M., Harahap, M., Turnip, A., 2019.
Abnormalities State Detection from P-Wave, QRS
Complex, and T-Wave in Noisy ECG, Journal of
Physics: Conference Series, Volume 1230, (2019)
012015. doi:10.1088/1742-6596/1230/1/012015.
Yunanto. (2015). Pertanggungjawaban Dokter Dalam
Transaksi Terapeutik (Cetakan 1). Semarang:
Universitas Diponegoro Semarang Press.
Application of Fuzzy Method to Predict Patient’s Belief in Doctor Qualifications
125
