
The Role of Chlorogenic Acid on Mice with Unilateral Ureteral
Obstruction Model: A Study toward Tubular Injury
Gina Andyka Hutasoit
1a
, Nur Arfian
2b
, Dwi Cahyani Ratna Sari
2c
,
Gabriella Bamba Ratih Lintin
3 d
, Mohammad Salman
4e
, Muhammad Mansyur Romi
2f
1
Patology Anatomy Department, Faculty of Medicine Universitas Tadulako, Palu, Indonesia
2
Anatomy Department, Faculty of Medicine, Public Health, and Nursing
Universitas Gadjah Mada, Yogyakarta, Indonesia
3
Anatomy Department, Faculty of Medicine Universitas Tadulako, Palu, Indonesia
4
Histology Department, Faculty of Medicine Universitas Tadulako, Palu, Indonesia
Keywords: Unilateral Ureteral Obstruction (UUO), Tubular Injury, Chlorogenic Acid (CGA)
Abstract: Chronic kidney disease is a global public health problem with a poor prognosis of renal fibrosis. Injury to
tubular epithelial cells is the beginning of the occurrence of renal fibrosis. Unilateral Ureteral Obstruction
(UUO) is a representative method for obtaining models of renal fibrosis. Chlorogenic acid (CGA) is known
to have a renoprotective, anti-inflammatory and antioxidant effect. This study aims to examine the role of
CGA preventing tubular injury on mice with UUO model. This study was a quasi-experimental research with
post-test only with control group design. Subjects were 25 male adult Swiss Webster mice (2-3 months old,
20-30 g weight). Subjects were divided into five groups: SO (Sham Operation), U7 (UUO day-7), U14 (UUO
day-14), UC7 (UUO+CGA day-7) and UC14 (UUO+CGA day-14). CGA 14 mg/kg body weight/day was
induced intraperitoneally. Tubular injury scores were examined with Periodic Acid Schiff staining. The data
obtained from this study were analyzed using SPSS. UUO group with CGA showed the tubular injury score
was lower than the UUO group without CGA with p-value < 0,005. The application of chlorogenic acid could
prevent tubular injury in mice model of UUO.
1 INTRODUCTION
Chronic renal disease was a global public health
problem with increased prevalence and incidence,
poor prognosis and high costs. According to the
Global Burden of Disease (2015), chronic renal
disease is the 18
th
leading cause of death in 2010 and
increased to 12
th
in 2015 (Neuen et al., 2017). The
global prevalence of chronic renal kidney is 13.4%
and tends to increased as the elderly population
increased, and the incidence of diabetes mellitus
(DM) and hypertension (Kemenkes, 2017). Central
Sulawesi Province was the region with the highest
prevalence of chronic kidney disease in Indonesia,
a
https://orcid.org/0000-0002-8043-564X
b
https://orcid.org/0000-0003-1694-2054
c
https://orcid.org/0000-0002-1126-4939
d
https://orcid.org/0000-0002-9791-1200
e
https://orcid.org/0000-0002-9417-1999
f
https://orcid.org/0000-0002-5842-9091
which was 0.5%, followed by Aceh, Gorontalo and
North Sulawesi (Kemenkes, 2013).
Chronic kidney disease results from an injury
such as an obstruction. This injury causes renal
structure changes such as renal fibrosis, tubular
atrophy, apoptosis and inflammation (Ucero et al.,
2013). Fibrosis was an excessive deposition of
extracellular matrix proteins in tissues that caused
scar formation. The existence of structural changes
due to fibrosis in the kidneys results in renal
physiological function loss to become End-Stage
Renal Disease (ESRD) (Neuen et al., 2017).
Unilateral Ureteral Obstruction (UUO) was the
most representative experimental method for
obtaining renal fibrosis inflammation models (Ucero
58
Hutasoit, G., Arfian, N., Ratna Sari, D., Ratih Lintin, G., Salman, M. and Romi, M.
The Role of Chlorogenic Acid on Mice with Unilateral Ureteral Obstruction Model: A Study toward Tubular Injury.
DOI: 10.5220/0010487700580062
In Proceedings of the 1st Jenderal Soedirman International Medical Conference in conjunction with the 5th Annual Scientific Meeting (Temilnas) Consortium of Biomedical Science Indonesia
(JIMC 2020), pages 58-62
ISBN: 978-989-758-499-2
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

et al., 2013). The UUO method was performed by
binding or unilateral ureteric ligation in experimental
animals. That could be subacute kidney injury
characterized by tubular cell injury, interstitial
inflammation, and increased intratubular pressure and
renal fibrosis inflammation (Ucero et al., 2013).
Tubular epithelial cells have multicellular structures
that bind together and acting as a barrier and
absorption/secretion. Injuries at tubular epithelial
cells were the beginning of renal fibrosis
(Guarino et
al., 2009). A tubular injury would make a decrease in
renal blood flow.
Chlorogenic acid was a compound polyphenol in
coffee which had contain a high antioxidant.
Chlorogenic acid effectively decreased the
metabolites of arachidonic acid, nitric oxide and the
production of proinflammatory cytokines compared
to ibuprofen
(Chauhan et al., 2012). This active
ingredient improved kidney dysfunction and kidney
injury induced by cisplatin that suppressed oxidative
stress, apoptosis, and autophagy by increasing kidney
regeneration (Domitrović et al., 2014). Research on
the role and utilization of chlorogenic acid to prevent
chronic renal disease was still not widely carried out.
The existing studies have not explained the various
pathways for preventing fibrosis in the incidence of
Chronic renal kidney, so this study needs to be done
to assess chlorogenic acid's role on the degree of renal
tubular injury used the UUO mice model so that it
could be considered as a new therapeutic agent.
Based on the above background, this study's
formulation problem was as follows: How is the
effect of chlorogenic acid on tubular injury scores at
the UUO mice model? General-purpose of this
research is to assess the role of administration
chlorogenic acid in preventing tubular injury in the
UUO mice model.
2 METHODS
This research was true experimental research used
post-test only controlled group design. Consists of
control and treatment groups. The subjects were 25
mature male Swiss Webster mice which were divided
into 5 groups, SO (Sham Operation/Control) group,
U7 (day-7 UUO + aquadest), U14 (day-14 UUO +
aquadest), UC7 (day-7 UUO + chlorogenic acid), and
UC14 (day-14 UUO + chlorogenic acid).
This study has obtained permission from the
Medical and Health Research Ethics Committee
Faculty of Medicine, Universitas Tadulako based on
the ethics feasibility certificate number
B.0941/UN28.1.30/KL/2018 on February 26, 2018.
2.1 Animal Model of Unilateral
Ureteral Obstruction (UUO)
Mice were anaesthetized using pentobarbital with a
dose of 0.1ml/10gBW/ times. After the anaesthesia
effect was achieved, the mice were placed on the
operating table with a pronation position. Mice hair
on the right-back was shaved then disinfected used
povidone-iodine, clamped with tweezers, then cut the
skin for ± 1.5 cm parallel to the body axis lumbar
region to the right lateral vertebrae region (region
flank). Cutting was done until the peritoneum visible.
Pinch the peritoneum with tweezers and then scissors
± 1 cm until the organs were visceral visible. Identify
the kidneys first, then used tweezers twisted over the
inferior pole and then pull the ureter up. Perform a
double ligation of the ureter in the inferior polus using
0.4 silk thread in the proximal area. The peritoneum
and skin were seen layer by layer using silk 0.4, then
gave povidone-iodine as an antiseptic.
2.2 Chlorogenic Acid Administration
Chlorogenic acid (Sigma-Aldrich C3878-1G) was
injected in mice with a dose of 14 mg/kg BW/day
intraperitoneally. A total of 25 mice of swiss webster
strains weighing 20-30 grams, 2-3 months old were
used in this study. Mice were divided into 5 groups.
The distribution for each group as follows: sham
operation (SO) group, intraperitoneal distilled water
injection for 14 days as a control; mice with UUO
injected with distilled water intraperitoneally for 7
days called group U7; mice with UUO injected with
chlorogenic acid for 7 days called UC7 group; mice
with UUO injected with distilled water
intraperitoneally for 14 days called group U14; mice
with UUO injected with chlorogenic acid for 14 days
group UC14.
2.3 Histopathological Examination
with Staining of Periodic Acid
Schiff (PAS)
Mice kidney would make by paraffin blocks and cut
to 4μm thickness. The tissue slides were halarized and
drained with flow water, followed by oxidation with
periodic acid 0.5%for 5 minutes. The slides were
washed with flow water. The slides were soaked in
the reagent Schiff for 15 minutes and washed with
flow water. Counterstained with haematoxylin for 1
minute and then washed with flow water. The slide
was then dehydrated and mounted.
The Role of Chlorogenic Acid on Mice with Unilateral Ureteral Obstruction Model: A Study toward Tubular Injury
59
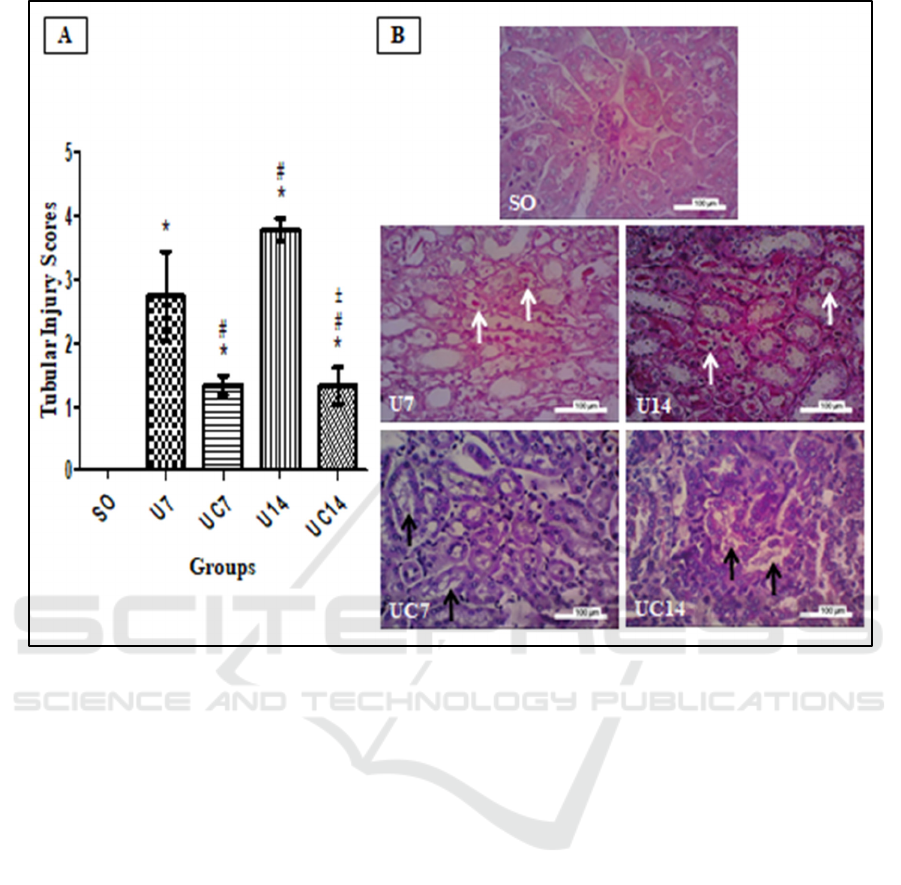
Figure 1: (A) Kruskal Wallis test p=0,000. *=p<0,05 vs SO, #=p<0,05 vs U7, ±=p<0,05 vs U14. (B) Microscopic findings of
the kidney with PAS staining. Description: White arrows show intraluminal cast in renal tubules that had atrophy. The black
arrow shows the brush border.
2.4 Statistical Analysis
Tubular injury scores classified from 0 to 4 (0 =
normal, 1 = tubular injury < 25% visual field, 2 =
tubular injury involving 25% -50% visual field, 3 =
tubular injury involving more than 51% -75% field
view, 4 = tubular injury involving > 75% visual field).
The assessment used a magnification of 400 times
and counted as many as 15 fields of view randomly
and did not overlap. This research variable has a ratio
scale.
Data were analyzed using the statistical
programme. Normality test used Shapiro-Wilk and
homogeneity test used the Levene Test. The
normality test for tubular injury scores was not
normally distributed, then used the Kruskal Wallis
test.
3 RESULTS
Histopathological examination of this study found
that there was good tubular appearance in the SO
group, with cuboidal epithelial cells in the proximal
tubule and distal, and the tubule's lumen still wide.
Besides that, the brush border was still intact, and no
protein was found cast in the lumen of the tubules.
While in the U7 and U14 groups tubular appearance
was found with various signs of injury such as the
presence of inflammatory areas, atrophic tubules, loss
of brush border in the proximal renal tubules, and
tubular dilatation with formation cast intraluminal.
Protein cast could be formed from podocyte damage,
resulting in protein escaping from glomerular
filtration, tissue hypoxia causes epithelial cell
apoptosis. Finally, together with the brush border, it
is released into the lumen. Compared to the UC7 and
UC14 groups that received chlorogenic acid, this
group clearly saw improvements in injury, namely the
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
60

brush border still attached to the epithelium with
intact epithelial cells and an inflammatory cell also
appear to be reduced. Tubular dilation in some
regions was still found with protein cast in the lumen,
but in small amounts when compared to the U7 and
U14 groups.
The tubular injury score results in the five sample
groups found that the U7 and U14 groups had a higher
tubular injury score compared to tubular injury scores
in the SO group. Simultaneously, tubular injury
scores in the UC7 and UC14 groups who received
chlorogenic acid were lower than those in the tubular
injury scores in the U7 and U14 groups who did not
get chlorogenic acid. This result shows that the UUO
model could cause a tubular injury that ends with
renal fibrosis. Kidney fibrosis occurs due to
obstruction, which causes an increased in intratubular
pressure and vasoconstriction in the kidneys, thus
ending with tissue ischemia. Also, in this study, it was
found that chlorogenic acid administration in the
UUO model can inhibit tubular injury, thereby
preventing renal fibrosis.
Statistical analysis results showed that there were
significant differences in tubular injury scores in the
U7 group (2,73±0,7) and U14 (3,77±0,18) compared
to the tubular injury scores in the SO (0) group. This
result shows that UUO was able to induce tubular
injury, which could end with renal fibrosis.
Comparison of tubular injury scores between the UC7
groups (1,33±0,15) and UC14 (1,32±0,29) showed a
significant difference compared to tubular injury
scores in the U7 and U14 groups. Tubular injury
scores indicated this result in the UC7 and UC14
groups given lower chlorogenic acid than tubular
injury scores in the U7 and U14 groups who were not
given chlorogenic acid.
4 DISCUSSION
In this study, it was found that chlorogenic acid had
roles in preventing tubular injury in laboratory UUO
mice to prevent renal fibrosis. This phenomenon
could be seen because the tubular injury score in
laboratory mice given chlorogenic acid was lower
than the tubular injury score in laboratory mice that
were not given chlorogenic acid.
According to the result, it was found that
unilateral ureter ligation in experimental animals
could cause kidney tubular injury, which resulted in
renal fibrosis. UUO method created a higher degree
of obstruction because ligation of one ureter caused a
total obstruction, increasing intratubular pressure and
causing secondary vasocontriction to the kidney,
leading to decreased GFR and tissue ischemia. This
condition caused further damage to kidney tubules so
that most tubular epithelial cells would undergo
apoptosis, resulting in atrophy (Ucero et al., 2013).
In this study, the tubular injury score was higher
in U7 and U14 groups which received UUO than in
SO group. An increased tubular injury score was
observed in exeperimental animals with longer UUO
(Tateishi et al., 2015). This result showed that UUO
was a representative model to create renal fibrosis
(Ucero et al., 2013). Other studies also explained
tubular injury caused by UUO by providing an
overview of tubular damage, tubular epithelial cells
apoptosis, fibrosis, and interstitial inflammation.
Increasing cell death could be seen in day-3 to day-14
after UUO, and specific histologic marker of chronic
kidney disease could be obtained after 1-2 weeks of
UUO. Cell death was started by an increased
hydrostatic tubular pressure accompanied by
increased free radical reactions and oxidative injuries
in proximal tubules (Xu et al., 2013). Moreover, the
tubular injury score was significantly higher in UC7
and UC14 groups which underwent UUO than in SO
group. Therefore, further study about the roles of
chlorogenic acid to tubular injury should be
conducted.
In this study, the tubular injury score was lower
in UUO groups, UC7 and UC14, which were given
chlorogenic acid than in UUO groups, U7 and U14,
which were not given chlorogenic acid. This result is
consistent with the previous study, which stated that
there were decreased tubular necrosis, intraluminal
cast, and tubular dilatation in laboratory mice given
chlorogenic acid (Domitrović et al., 2014). The
decrease in tubular injury score in groups given
chlorogenic acid was due to antioxidant, anti-
inflammatory, antibacterial, and anticarcinogenic
properties of chlorogenic acid (Naveed et al., 2018;
Tajik et al., 2017).
The limitation in this study is that it has not
investigated the role of chlorogenic acid in renal
fibrosis on epithelial cell markers and mesenchymal
cell markers that affect the occurrence of tubular
injury, therefore further research is needed in this
regard.
5 CONCLUSION
Tubular injury score in the UUO mice model given
chlorogenic acid was lower than the UUO mice
model without chlorogenic acid. Further research can
be sharpened by researching the role of chlorogenic
acid in the tubular injury and the analysis of the role
The Role of Chlorogenic Acid on Mice with Unilateral Ureteral Obstruction Model: A Study toward Tubular Injury
61

of chlorogenic acid in renal fibrosis by examining
other epithelial cell markers and other mesenchymal
cell markers.
ACKNOWLEDGEMENT
The authors are grateful to Wiwit Ananda, Cynthia,
Maulida, Yuyun and Mulyana in Anatomy
Departement Faculty of Medicine, Public Health, and
Nursing Universitas Gadjah Mada, which has helped
a lot in this research.
REFERENCES
Neuen, B.L., Chadban, S.J., Demaio, A.R., Johnson, D.W.
and Perkovic, V., 2017. Chronic kidney disease and the
global NCDs agenda. BMJ Global Health, 2(2):
e000380.
Kemenkes, R.I., 2017. Situasi penyakit ginjal
kronis. InfoDATIN. Pusat Data dan Informasi
Kementrian Kesehatan RI. Jakarta. ISSN, pp.2442-
7659.
Kemenkes, R.I., 2013. Riset Kesehatan Dasar
2013. Jakarta: Badan Penelitian dan Pengembangan
Kesehatan.
Ucero, A.C., Benito-Martin, A., Izquierdo, M.C., Sanchez-
Nino, M.D., Sanz, A.B., Ramos, A.M., Berzal, S., Ruiz-
Ortega, M., Egido, J. and Ortiz, A., 2014. Unilateral
ureteral obstruction: beyond obstruction. International
urology and nephrology, 46(4), pp.765-776.
Guarino, M., Tosoni, A. and Nebuloni, M., 2009. Direct
contribution of epithelium to organ fibrosis: epithelial-
mesenchymal transition. Human pathology, 40(10),
pp.1365-1376.
Chauhan, P.S., Satti, N.K., Sharma, P., Sharma, V.K., Suri,
K.A. and Bani, S., 2012. Differential effects of
chlorogenic acid on various immunological parameters
relevant to rheumatoid arthritis. Phytotherapy
Research, 26(8), pp.1156-1165.
Domitrović, R., Cvijanović, O., Šušnić, V. and Katalinić,
N., 2014. Renoprotective mechanisms of chlorogenic
acid in cisplatin-induced kidney
injury. Toxicology, 324, pp.98-107.
Tateishi, Y., Osada-Oka, M., Tanaka, M., Shiota, M.,
Izumi, Y., Ishimura, E., Motoyama, K., Inaba, M. and
Miura, K., 2015. Myeloid HIF-1 attenuates the
progression of renal fibrosis in murine obstructive
nephropathy. Journal of Pharmacological
Sciences, 127(2), pp.181-189.
Xu, Y., Ruan, S., Wu, X., Chen, H., Zheng, K. and Fu, B.,
2013. Autophagy and apoptosis in tubular cells
following unilateral ureteral obstruction are associated
with mitochondrial oxidative stress. International
Journal of Molecular Medicine, 31(3), pp.628-636.
Naveed, M., Hejazi, V., Abbas, M., Kamboh, A.A., Khan,
G.J., Shumzaid, M., Ahmad, F., Babazadeh, D.,
FangFang, X., Modarresi-Ghazani, F. and WenHua, L.,
2018. Chlorogenic acid (CGA): A pharmacological
review and call for further research. Biomedicine &
Pharmacotherapy, 97, pp.67-74.
Tajik, N., Tajik, M., Mack, I. and Enck, P., 2017. The
potential effects of chlorogenic acid, the main phenolic
components in coffee, on health: a comprehensive
review of the literature. European Journal of
Nutrition, 56(7), pp.2215-2244.
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
62
