
The Renal Protective Potential Effect of Infusion of Anti-urolithiasis
Formula in Urolithiasis Patients: A Randomized Clinical Study
Ulfatun Nisa
1a
, Peristiwan Ridha Widhi Astana
1b
, Saryanto
1c
, Tyas Friska Dewi
1d
and Enggar Wijayanti
1e
1
Medicinal Plant and Traditional Medicine Research and Development Center, Ministry of Health, Tawangmangu,
Indonesia
Keywords: Renoprotective, Anti–urolithiasis Formula, Urolithiasis Disease
Abstract: Kidney stones and related urological procedures can lead to chronic kidney disease (CKD). The constituent
plants of an anti-urolithiasis formula developed by B2P2TOOT have a potential renoprotective effect, thus
preventing CKD progression. This randomized open-label clinical study with end-blinded observation was
aimed to evaluate the possible renoprotective effect of anti-urolithiasis formula infusions in urolithiasis
patients. Two hundred volunteer subjects were randomly allocated into two groups: anti-urolithiasis herbal
formula (AHF) and commercial polyextract lithotripsy (CPL). Urine tests were performed, and the estimated
glomerular filtration rate (eGFR) was calculated using a CKD-EPI equation at baseline (day 0) and after the
intervention (day 56). The analysis was done within each group and between both groups using paired sample
T-test and independent T-tests. An increase in the eGFR of subjects in the AHF group was found, although it
was not statistically significant (p=0.35). The mean of the eGFR of subjects in the CPL group after the
intervention was lower, also statistically insignificant (p=0.56). Nevertheless, there were significant
differences in the eGFR after intervention between both groups (p=0.044, 95% CI 0.16–12.4). Our findings
suggest that AHF has a slight potential effect on renal function preservation in urolithiasis patients.
1 INTRODUCTION
Urolithiasis has become a worldwide health burden.
Its incidence rates are 10% for men and 5% for
women (D'Costa et al., 2016). The high recurrence
rate of urolithiasis results in health financing issues
and considerable morbidity (Lee et al., 2015). Also,
several studies have revealed that the formation of
stones in the urinary tract has a strong correlation with
adverse renal outcomes. However, the mechanism
underlying kidney stones and diminished kidney
function is likely multifactorial (Alexander et al.,
2012; Coe et al., 2010). Urolithiasis plays a
significant role in influencing the risk of adverse renal
outcomes and prior history of recurrent symptomatic
episodes. Accordingly, it might produce an increased
risk of end-stage renal disease (ESRD). For example,
a
https://orcid.org/0000-0001-8743-3121
b
https://orcid.org/0000-0002-7341-4330
c
https://orcid.org/0000-0002-0442-8261
d
https://orcid.org/0000-0002-4467-9372
e
https://orcid.org/0000-0002-1322-6784
the progressive calcification of calcium kidney stones
at the tubular basement membrane and the ducts of
Bellini causes renal damage through progressive
scarring, leading to ESRD (Coe et al., 2010; Evan,
2010).
Urolithiasis management has recently played an
essential role in preventing several future health
complications—one of the standard procedures in the
management of nephrolithiasis is extracorporeal
shock wave lithotripsy (ESWL). ESWL had been
regularly utilized in the management of urolithiasis.
Nevertheless, it might significantly contribute to the
increased risk of recurring stones and result in greater
difficulty when comminuting stones with ESWL
(Evan, 2010). Moreover, it can result in several
complications, leading to kidney function loss
(Shekar Kumaran and Patki, 2011). This hypothesis
Nisa, U., Widhi Astana, P., Saryanto, ., Dewi, T. and Wijayanti, E.
The Renal Protective Potential Effect of Infusion of Anti-urolithiasis Formula in Urolithiasis Patients: A Randomized Clinical Study.
DOI: 10.5220/0010488300910097
In Proceedings of the 1st Jenderal Soedirman International Medical Conference in conjunction with the 5th Annual Scientific Meeting (Temilnas) Consortium of Biomedical Science Indonesia
(JIMC 2020), pages 91-97
ISBN: 978-989-758-499-2
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
91

has suggested a decrease in renal function by
vasoconstriction, and its persistent stone fragments
may induce acute renal injury (Agawane et al., 2019;
Khan et al., 2011; Nizami et al., 2012; Srisubat et al.,
2014). By contrast, another study found no
correlation between ESWL and CKD development
(D'Costa et al., 2016; E. et al., 2008). The
retrospective study revealed that urological
procedures could significantly increase the risk of
developing elevated serum creatinin but were not
significant in progressing CKD itself (D'Costa et al.,
2016). There is no appropriate drug for the treatment
of urolithiasis despite technological advances in the
field of medicine. However, it is worthwhile to
explore the potential benefits of medicinal plants,
which may affect anti-urolithiasis and restore renal
impairments.
Polyherbal treatment can be considered an
alternative approach to treating urolithiasis. The
investigation of phytotherapy for urolithiasis has been
reported in an ethnopharmacology study, in vitro, and
in vivo models (Ahmed et al., 2016; Akanae et al.,
2010; Nisa and Astana, 2018; Patankar et al., 2020;
Yadav, RD., Jain, SK., Alok, Shashi., Mahor, Alok.,
Bharti, JP., Jaiswal et al., 2011). The diuretic activity
of Orthosiphon stamineus is different when combined
with hydrochlorothiazide and furosemide (Adam et
al., 2009). It takes a longer time to produce effects
than synthetic diuretics but, notably, does not include
any side effects (Tiwari et al., 2017). Meanwhile,
Phyllanthus niruri can inhibit lithiasis' growth in rats
(Morán et al., 2013). The administration of
Phyllanthus niruri can decrease mRNA p65NF-κB
and mRNA IL-6 levels in the kidneys of diabetic rats
(Giribabu et al., 2017). Jonnel B.P. et al. revealed that
an increase in Imperata cylindraca extract
concentration is related to decreased serum creatinine
and blood urea nitrogen (BUN) levels. Thus, several
medicinal plants appear to have distinct mechanisms
for urolithiasis that generate synergetic effects to
facilitate stones' passage.
The constituent plants of the anti-urolithiasis
formula developed by the Medicinal Plant and
Traditional Medicine Research and Development
Center (B2P2TOOT-in Bahasa) have a potential
renoprotective effect, which suggests they can serve
as an alternative method of preventing CKD
progression. This method's safety and efficacy have
been proven in clinical trials (Nisa and Astana, 2019).
Several compositions of the AHF had been reported
to have a potential renoprotective effect in a single-
use form. This study aims to evaluate the possible
renoprotective effect of an anti-urolithiasis herbal
formula in urolithiasis patients.
2 MATERIALS AND METHODS
The study was conducted by the Traditional Plant and
Traditional Medicine Research and Development
Center at the Ministry of Health Indonesian and
involved191 urolithiasis patients. The design of the
study was a purposive randomized open-label study
design, with end-blinded observation. We involved
70 physicians, who all have Saintifikasi Jamu (SJ)
certifications as investigators. The ethics committee
approved the study protocol of the National Institute
of Research and Development (LB.02.01/5.2/KE
063/2016) on March 13
th
, 2017. The principal
investigator was qualified in traditional and allopathic
medicine and clinical trials, in accordance with Good
Clinical Practices (GCP).
Volunteer patients who fulfilled the inclusion
criteria participated in this study. Before participating
in the study, each subject was requested to read and
sign an informed consent form. The inclusion criteria
were: an age of 17-60 years old, a history of
urolithiasis, the presence of a stone<2 cm in diameter,
serum creatinine levels of<2 g/dl, and liver and
kidney function within a normal range. Patients with
complications from severe diseases and those
requiring surgical intervention were excluded from
the study. Eligible subjects were randomized by
computer software into two groups: the AHF and the
CPL group.
In the AHF group, each subject was given an
herbal formula, which consisted of a dried simplisia
of 10 g of S. arvensis, 6 g of O. stamineus, 4 g of
Strobilanthes crispus, 5 g of Imperata cylindrica, 5 g
of C. xanthorrhiza, 4 g of Curcuma domestica, and 3
g of P. niruri. Each subject was requested to prepare
an infusion from the formula. The AHFwas prepared
by boiling 1 L of water, adding the simplisia into the
boiling water, and letting the mixture boil for 15
minutes. Subjects were instructed to drink the filtered
water twice a day for 56 days, after breakfast and
dinner. Meanwhile, in the CPL group, subjects
consumed CPL, which consisted of an extract of 18
mg of O. stamineus, 6 mg of S. crispa, 24 mg of S.
arvensis L., 2.4 mg of P. niruri, and 100 mg of
Plantago major. They took one capsule of CPL four
times daily, also for 56 days.
Demographic data such as age, sex, BMI, history
of stone recurrence, and stone size were recorded at
day 0 of the study. Urine tests (routine and
microscopic), including tests of urine turbidity, pH,
specific gravity, LE, Nitrit, RBC, and albuminuria,
were performed on days 0, 28, and 56 to observe the
fluctuation of urine quality. The kidney's biochemical
parameters
(creatinine and BUN) were measured on
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
92

Figure 1: Enrollment, randomization, allocation, follow-up, and analysis
day 0 and day 56, followed by a calculation of the
estimated glomerular filtration rate (eGFR) using a
CKD-EPI equation.
The data were analyzed statistically using a
GraphPad Prism program for statistical analysis
version 8.0. Descriptive data were calculated and
presented in Table 1. To determine differences before
and after treatment, we performed a paired T-test. An
independent T-test was also conducted to determine
the differences between the two groups.
Alternatively, the Wilcoxon test and Mann–Whitney
U-test were used when there was an abnormal data
distribution in the Kolmogorov–Smirnov test results.
3 RESULTS
Based on Figure 1, the total number of patients
recruited in this studywas191 patients. As many as97
and 94 subjects were analyzed in the AHF and CPL
group, respectively. Each group had subjects who
could not continue the intervention because of a
failure to follow up. The baseline characteristics of
patients are summarized in Table 1.
Table 1: Demographic data of patients.
Parameters AHF
(N=97)
CPL
(N=94)
Mean a
g
e45-55
yr
45-55
yr
Male:female 1.9:1 1.7:1
BMI
(Overweight:normoweight)
1.18:1 1.38:1
History of recurrent
urolithiasis
1 yr
(34%)
1 yr
(33%)
Avera
g
e size of stone
10.82±8.19 8.07±5.19
Comparing male and female participants between
the two groups were 1.9:1 and 1.7:1 in the AHF and
CPL group, respectively. Each group also had a
similar BMI ratio between overweight and
normoweight participants. The majority of patients
were in the range of 45-55 years old. About 30% of
patients had a history of stone recurrence within one
year before the study started. The mean of the size of
the stone was similar between the two groups. Figure
2A shows information about the mean of the eGFR for
pre-treatment(day 0) and post-treatment(day 56).
There was no significant difference in the eGFR
between the two groups on day 0. However, after 56
days of treatment, there were significant differences in
the eGFR between the AHF group and the CPL group
(p=0.044, 95% CI 0.16 – 12.4).
The Renal Protective Potential Effect of Infusion of Anti-urolithiasis Formula in Urolithiasis Patients: A Randomized Clinical Study
93
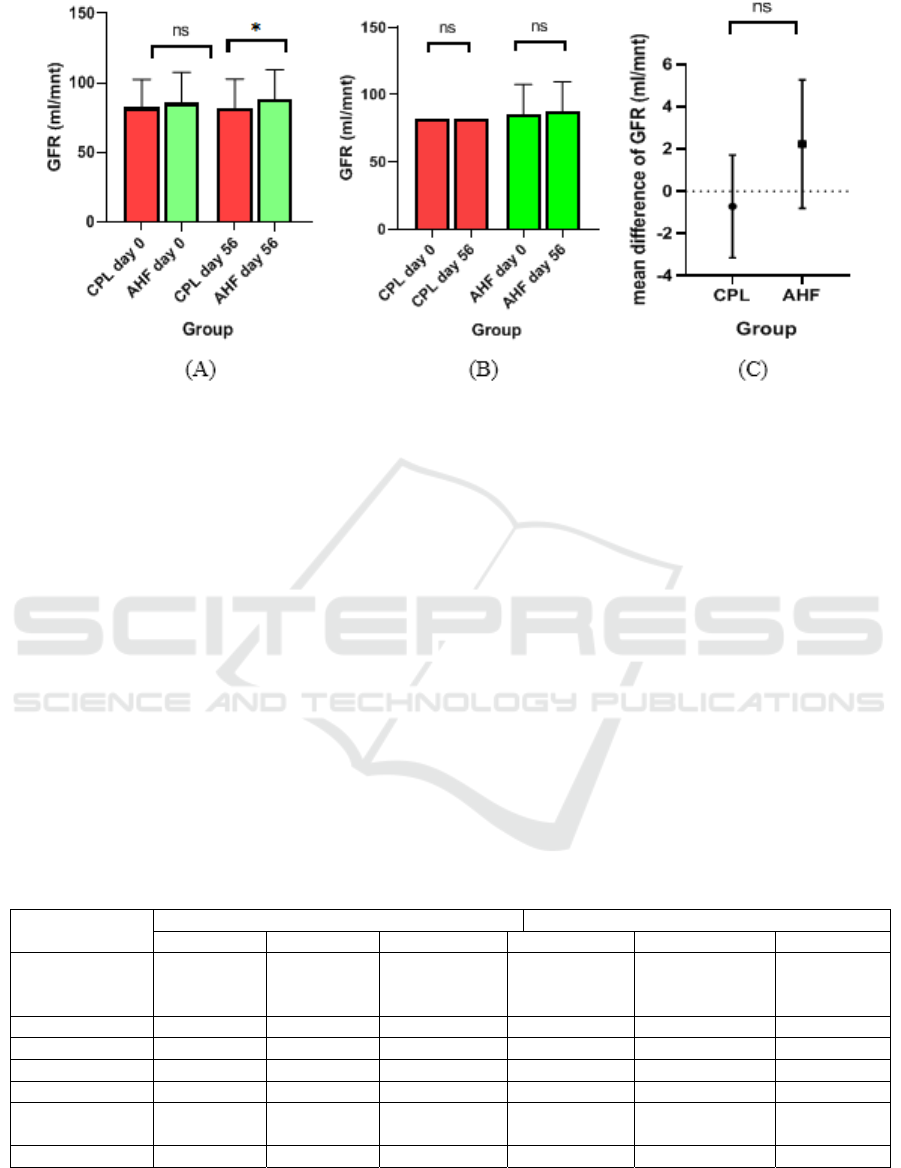
Figure 2: (A) Mean of eGFRfor pre- and post-treatment between the two groups.(B)Mean difference between AHF and CPL
groups. (C)Mean of eGFR before and after treatment in each group.
An increase in subjects' eGFR was found in the
AHF group on day 56 compared with day 0 (2.24
mL/min per 1.73 m2). However, this was not
statistically significant (p=0.35). In the CPL group,
the average eGFR of subjects on day 56 was lower
than on day 0, though this was also not statistically
significant (p=0.56) (Figure 2B). We calculated the
difference in theeGFR value between day 0 and day
56 in each group, as represented in figure 2C. The
difference in the eGFR in the AHF group showed a
positive value, while in the CPL group, it showed a
negative one.
However, the independent T-test analysis showed
no significant differences. Table 2 shows the urine test
parameters of subjects. These results demonstrate that
both groups' urine turbidity had lower scores at the end
of treatment than in the middle or baseline. There was
a statistically significant difference during treatment
compared to the baseline.
Furthermore, the CPL group's urine turbidity had
substantial differences in the middle of treatment
compared to the baseline. From the table, we can also
see that there is no change in any other urine test
parameter (pH, specific gravity, LE, Nitrite, RBC, or
albuminuria).
4 DISCUSSION
This study was conducted to the potential
renoprotective effect of an anti-urolithiasis herbal
formula in urolithiasis patients. The eGFR Anti-
urolithiasis Herbal Formula's group has a significant
Table 2: Effect of treatment on urine test parameters.
Parameters
AHF CPL
da
y
0 da
y
28 da
y
56 da
y
0 da
y
28 da
y
56
Urine turbidity 1.95 ± 0.08 1.80 ± 0.08
a
1.62±0.0
a
p<0.05
b
p
<0.05
1.88 ± 0.08 1.73 ± 0.07
a
p<0.05
1.68±0.07
b
p<0.05
Urine pH 5.90 ± 0.09 6.74 ± 0.76 6.47 ± 0.57 5.97±0.096 6.02 ± 0.09 6.01 ± 0,09
Specific gravit
y
1.014±0.001 1.016±0.002 1.013±0.001 1.000±0.02 1.015±0.02 1.014±0.02
LE 82.55±16.41 74.64±15.85 72.73±15.90 92.02±17.95 91.76±18.06 87.04±18.09
Nitrite 0.04±0.02 0.03±0.02 0.04 ±0.02 0.08 ±0.03 0.05 ± 0.02 0.03 ± 0.02
No.of RBC’s
p
erHPF
59.10± 9.65 51.01±8.96 53.19±9.42 48.39±8.55 36.83±7.49 36.94±7.66
Albuminuria 20.57 ±3.75 16.94±3.71 17.89±4.05 16.40±2.52 14.84±2.50 12.83±2.20
Mean±SEM, Statistical analysis performed using independent T-test
a
As compared to day0
b
As compared to day 28
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
94

difference in day 56 after treatment compared to the
CPL group. However, other parameters have not a
significant difference in both groups. Furthermore,
after urolithiasis formation, the hindrance of urine
flow can cause a decrease in the Glomerular Filtration
Rate (GFR). Therefore, waste material, especially
BUN (Blood Urea Nitrogen), creatinine, and uric
acid, can be collected in the blood(Kaleeswaran et al.,
2019). This study showed that the AHF and CPL had
diuretic activity, preventing the elevation of these
parameters. Following a previously published report,
the improvement of the eGFR in the AHF group
compared to the CPL group was correlated to
decreased urinary stones size (Nisa and Astana,
2019).
Orthosiphon stamineus and Phyllanthus niruri L
are indigenous medicines widely used in
Indonesia(Nisa and Astana, 2018). Meanwhile,
previous studies reported that the content of
rosmarinic acid in Orthosiphon stamineus had
nephroprotective effects in diabetic nephropathy. It
may have conserved glomerular number loss(Almatar
et al., 2014; Tavafi et al., 2011). However, this
complex mechanism remains unclear, and the
antioxidant properties of Orthosiphon stamineus may
play a significant role in this process. The activation
of s cellular oxidation process was associated with
urolithiasis and chronic calculus
pyelonephritis(Boonla, 2018; Ceban et al., 2016).
The potential anti-urolithiasis activity of Phyllantus
niruri plays an essential role in the early stages of
stone formation. Phyllanthus nirurican makes stones
smoother and more fragile, facilitating the dissolution
of calculi (Lee et al., 2016).
On the other hand, most of the AHF's constituents'
main activity is as a diuretic agent. In terms of diuretic
action, various phytoconstituents may interact with a
synergistic effect, leading to enhanced renal output.
The AHF treatment was revealed to increase the GFR
by dual effects of controlling the growth of stones and
may also have a nephroprotective effect. The
renoprotective strategies of the AHF are based on
several mechanisms and are exceedingly complex.
Meanwhile, the antioxidant and anti-inflammatory
effects of AHF may contribute to the preservative
effects of microcirculation.
The present study results show the proportion of
subjects who had a history of recurrence, the rate of
which was 33%. Meanwhile, the ordinary recurrence
rate of kidney stone disease within one year is only
10%(Patankar et al., 2020). Indeed, the high
recurrency of urolithiasis disease was closely
correlated with side effects, leading to renal function
loss progression. Various degrees of renal
insufficiency is associated with urolithiasis as well.
This phenomenon suggests that a combination of
frequent stone episode recurrence, urinary tract
reinfection, and frequent urological interventions
may initiate renal insufficiency. Many studies have
found that urine parameters could serve as predictive
factors for estimating renal function. One of the key
biomarkers of renal damage is albuminuria. Several
studies have reported that this decreases the risk of
renal damage and urine albumin levels(Abebe et al.,
2019). Albuminuria is a dysfunctional endothelial
marker in the renal region, brain, and heart (Mardiana
et al., 2012). Thus, anti-albuminuria was a target for
the renoprotective agent. Remuzi and Bertani
suggested that albuminuria was a severity marker for
renal injury, indicating that an increase in leak plasma
protein is associated with an increase in kidney
damage severity (De Zeeuw et al., 2004). Several
theories attempt to explain how urolithiasis can
induce renal progression. Several mechanisms
underlying nephrolithiasis can lead to CKD
development through scarring and the deterioration of
renal function. This phenomenon may also cause
direct damage to post-calcifications and
crystallization of the tubular lumen, resulting from
recurrent stone obstruction (D'Costa et al
., 2016).
The limitation of this study is the parameters of
renal function, which used an estimated calculation.
It still needs further research for real renal function
parameters.
5 CONCLUSIONS
Our findings suggest that AHF has a slight potential
effect on renal function preservation in urolithiasis
patients.
ACKNOWLEDGEMENTS
This study was a part of the Saintifikasi Jamu formula
(SJ) program that was carried out with the Ministry of
Health's financial support of the Republic of
Indonesia. We would like to thank the Head of
B2P2TOOT in Tawangmangu, Indonesia, and all
staff.
REFERENCES
Abebe, M., Adane, T., Kefyalew, K., Munduno, T., Fasil,
A., Biadgo, B., et al., 2019. Variation of Urine
The Renal Protective Potential Effect of Infusion of Anti-urolithiasis Formula in Urolithiasis Patients: A Randomized Clinical Study
95

Parameters among Diabetic Patients: A Cross-Sectional
Study. Ethiop. J. Health Sci. 29, 877–86.
doi:10.4314/ejhs.v29i1.9
Adam, Y., Somchit, M.N., Sulaiman, M.R., Nasaruddin,
A.A., Zuraini, A., Bustamam, A.A., et al., 2009.
Diuretic properties of Orthosiphon stamineus Benth. J.
Ethnopharmacol. doi:10.1016/j.jep.2009.04.014
Agawane, S.B., Gupta, V.S., Kulkarni, M.J., Bhattacharya,
A.K., Koratkar, S.S., Rao, V.K., 2019. Patho-
physiological evaluation of Duranta erecta for the
treatment of urolithiasis. J. Ayurveda Integr. Med. 10,
4–11. doi:10.1016/j.jaim.2017.08.001
Ahmed, S., Hasan, M.M., Alam, Z., 2016. Antiurolithiasis
plants in different countries and cultures. J.
Pharmacogn. Phytochem. 5, 102–15.
Akane, W., Tsujihata, M., Yoshioka, I., Nonomura, N.,
Okuyama, A., 2010. Orthosiphon grandiflorum has a
protective effect in a calcium oxalate stone-forming rat
model. Urol. Res. 38, 89–96. doi:10.1007/s00240-010-
0265-6
Alexander, R.T., Hemmelgarn, B.R., Wiebe, N., Bello, A.,
Morgan, C., Samuel, S., et al., 2012. Kidney stones and
kidney function loss: a cohort study. BMJ 345, e5287.
doi:10.1136/bmj.e5287
Almatar, M., Ekal, H., Rahmat, Z., 2014. A Glance on
Medical Applications of Orthosiphon stamineus and
Some of its Oxidative Compounds. Int. J. Pharm. Sci.
Rev. Res. 24, 83–8.
Boonla, C., 2018. Oxidative Stress in Urolithiasis, in:
Reactive Oxygen Species (ROS) in Living Cells. pp.
129–58. doi:10.5772/intechopen.75366
Ceban, E., Banov, P., Galescu, A., Botnari, V., 2016.
Oxidative stress and antioxidant status in patients with
complicated urolithiasis. J. Med. Life 9, 259–62.
Coe, F.L., Evan, A.P., Worcester, E.M., Lingeman, J.E.,
2010. Three pathways for human kidney stone
formation. Urol. Res. 38, 147–60. doi:10.1007/s00240-
010-0271-8
D'Costa, M., Savcic-Kos, R., Huang, J., Rule, A.D., Murali,
N., 2016. Urological procedures in urolithiasis and their
association with chronic kidney disease. Clin. Med.
Res. 14, 75–82. doi:10.3121/cmr.2016.1261
De Zeeuw, D., Remuzzi, G., Parving, H.H., Keane, W.F.,
Zhang, Z., Shahinfar, S., et al., 2004. Proteinuria, a
target for renoprotection in patients with type 2 diabetic
nephropathy: Lessons from RENAAL. Kidney Int. 65,
2309–20. doi:10.1111/j.1523-1755.2004.00653.x
E., K.A., J., L.A., E., P.D., T., G.M., 2008. Long-Term
Outcomes of Percutaneous Nephrolithotomy Compared
to Shock Wave Lithotripsy and Conservative
Management. J. Urol. 179, 2233–7.
doi:10.1016/j.juro.2008.01.115
Evan, A.P., 2010. Physiopathology and etiology of stone
formation in the kidney and the urinary tract. Pediatr.
Nephrol. 25, 831–41. doi:10.1007/s00467-009-1116-y
Giribabu, N., Karim, K., Kilari, E.K., Salleh, N., 2017.
Phyllanthus niruri leaves aqueous extract improves
kidney functions, ameliorates kidney oxidative stress,
inflammation, fibrosis and apoptosis and enhances
kidney cell proliferation in adult male rats with diabetes
mellitus. J. Ethnopharmacol. 205, 123–37.
doi:10.1016/j.jep.2017.05.002
Kaleeswaran, B., Ramadevi, S., Murugesan, R.,
Srigopalram, S., Suman, T., Balasubramanian, T.,
2019. Evaluation of anti-urolithiasis potential of ethyl
acetate extract of Pedalium murex L. on struvite crystal
(kidney stone). J. Tradit. Complement. Med. 9, 24–37.
doi:10.1016/j.jtcme.2017.08.003
Khan, A., Bashir, S., Khan, S.R., Gilani, A.H., 2011.
Antiurolithic activity of Origanum vulgare is mediated
through multiple pathways. BMC Complement. Altern.
Med. doi:10.1186/1472-6882-11-96
Lee, N.Y.S., Khoo, W.K.S., Adnan, M.A., Mahalingam,
T.P., Fernandez, A.R., Jeevaratnam, K., 2016. The
pharmacological potential of Phyllanthus niruri. J.
Pharm. Pharmacol. 68, 953–69.
doi:10.1111/jphp.12565
Lee, S.K., Kim, Y., Kang, H.W., Kim, W.T., Kim, Y., Yun,
S., et al., 2015. Age and gender-associated metabolic
characteristics of urinary stone patients. J. Biomed Res.
16, 172–6.
Mardiana, Kartini, A., Widjasena, B., 2012. Media Medika.
Pemberian Cairan Karbohidrat Elektrolit, Status
Hidrasi dan Kelelahan pada Pekerja Wan. 46, 6–11.
Morán, E., Budía, A., Broseta, E., Boronat, F., 2013.
Phytotherapy in urology. Current scientific evidence of
its application in urolithiasis, chronic pelvic pain,
erectile dysfunction and urinary tract infections. Actas
Urológicas Españolas (English Ed. 37, 174–80.
doi:10.1016/j.acuroe.2012.07.016
Nisa, U., Astana, P.R.W., 2019. Evaluation of Antiurolithic
Herbal Formula for Urolithiasis: a Randomized Open-
Label Clinical Study. Asian J. Pharm. Clin. Res. 12,
88–93. doi:10.22159/ajpcr.2019.v12i4.30232
Nisa, U., Astana, P.R.W., 2018. Studi Etnofarmakologi
Tumbuhan obat untuk Mengobati Gangguan Batu
Saluran Kemih di Sumatera Indonesia. Bul. Penelit.
Kesehat. 46, 275–86.
Nizami, A.N., Rahman, M.A., Ahmed, N.U., Islam, M.S.,
2012. Whole Leea macrophylla ethanolic extract
normalizes kidney deposits and recovers renal
impairments in an ethylene glycol-induced urolithiasis
model of rats. Asian Pac. J. Trop. Med. 5, 533–8.
doi:10.1016/S1995-7645(12)60094-7
Patankar, S.B., Mujumdar, A.M., Bernard, F., Supriya, P.,
2020. Safety and efficacy of an herbal formulation in
patients with renal calculi - A 28 week, randomized,
double-blind, placebo-controlled, parallel-group study.
J. Ayurveda Integr. Med. 11, 62–7.
doi:10.1016/j.jaim.2018.08.001
Shekar Kumaran, M.G., Patki, P.S., 2011. Evaluation of an
Ayurvedic formulation (Cystone), in urolithiasis: A
double-blind, placebo-controlled study. Eur. J. Integr.
Med. 3, 23–8. doi:10.1016/j.eujim.2011.02.003
Srisubat, A., Potisat, S., Lojanapiwat, B., Setthawong, V.,
Laopaiboon, M., 2014. Extracorporeal shock wave
lithotripsy (ESWL) versus percutaneous
nephrolithotomy (PCNL) or retrograde intrarenal
surgery (RIRS) for kidney stones. Cochrane Database
JIMC 2020 - 1’s t Jenderal Soedirman International Medical Conference (JIMC) in conjunction with the Annual Scientific Meeting
(Temilnas) Consortium of Biomedical Science Indonesia (KIBI )
96

Syst. Rev. 2014.
doi:10.1002/14651858.CD007044.pub3
Tavafi, M., Ahmadvand, H., Khalatbari, A., Tamjidipoor,
A., 2011. Rosmarinic acid ameliorates diabetic
nephropathy in uninephrectomized diabetic rats. Iran.
J. Basic Med. Sci. 14, 275–83.
doi:10.22038/ijbms.2011.5006
Tiwari, P., Kothiyal, P., Ratan, P., 2017. Antiurolithiasis
Effect of Some Polyherbal Formulations Used in
Experimentally Induced Urolithiasis: a Review. Int.
Res. J. Pharm. 8, 14–22. doi:10.7897/2230-8407.08566
Yadav, RD., Jain, SK., Alok, Shashi., Mahor, Alok., Bharti,
JP., Jaiswal, M., Yadav D, R., Jain S, K., Alok, S.,
Mahor, A., Bharti P, J., et al., 2011. Herbal Plants Used
in The Treatment of Urolithiasis: A Review. Int. J.
Pharm. Sci. Res. 2, 1412–20.
The Renal Protective Potential Effect of Infusion of Anti-urolithiasis Formula in Urolithiasis Patients: A Randomized Clinical Study
97
