
Privacy with Health Information Technologies: What Story Do Data
Breaches in US Tell Us?
Sylvestre Uwizeyemungu
1a
and Placide Poba-Nzaou
2b
1
Département des Sciences Comptables, Université du Québec à Trois-Rivières (UQTR),
3351, boul. des Forges, C.P. 500, Trois-Rivières (Québec), Canada
2
Département d’Organisation et Ressources Humaines, ÉSG – Université du Québec à Montréal (UQAM),
315, Ste-Catherine Est, Montréal (Québec), Canada
Keywords: Health Data Breach, Health Information Technology, Privacy.
Abstract: Over the last decades, health policy makers have encouraged healthcare organizations to leverage health
information technology (HIT) for improving the accessibility, the quality, and the efficiency of health service
delivery. The adoption of HIT has contributed to the digitization of health data, which has made these data
vulnerable to information technology (IT) related security breaches. Based on data published by the US
Department of Health and Human Services (DHHS), we analyze the portrait of health data breaches in the
USA from 2009 to 2018 in order to figure out whether there are clear patterns of breach that stand out. In
addition to descriptive statistics characterizing health data breaches, this study suggests three well-separated
patterns of these breaches: (1) breaches mainly related to hacking / IT incident, (2) breaches due to
unauthorized access / disclosure, and (3) breaches due to theft. All these patterns of breaches have different
implications regarding priorities for health IT security and privacy professionals. However, further
investigations with additional data are needed to fully comprehend the phenomenon of health data breaches
and their implications in terms of IT security and privacy.
1 INTRODUCTION
Over about the last three decades, health policy
makers have encouraged healthcare organizations to
intensively adopt health information technology
(HIT) (Blumenthal, 2009, 2011; Rozenblum et al.,
2011). The premise was that the leverage of
information technology (IT) in healthcare sector will
play a major role in improving the accessibility, the
quality, the safety, and the efficiency of healthcare
services (Daniel, 2018; McKenna, Dwyer, & Rizzo,
2018; Tubaishat, 2019; Wani & Malhotra, 2018).
Incentives for the “meaningful use” (Hogan &
Kissam, 2010b) of IT has led to higher rates of HIT
adoption and use among targeted hospitals (Adler-
Milstein & Jha, 2017; Jones & Furukawa, 2014). But,
at the same time, the increasingly digitized health
information has become vulnerable to IT-related
security breaches, thus exposing healthcare
organizations to “the mixed blessing of the digital
a
https://orcid.org/0000-0002-1532-8848
b
https://orcid.org/0000-0002-7007-764X
age” (Myers, Frieden, Bherwani, & Henning, 2008,
p. 794). Data breaches in healthcare sector have
become a common occurrence: the number of data
breaches is on the rise, as well as the number of
individuals affected (Koczkodaj, Mazurek, Strzałka,
Wolny-Dominiak, & Woodbury-Smith, 2019; Liu,
Musen, & Chou, 2015). Given the highly sensitive
nature of health information, the potential impacts of
health data breaches may be disastrous for patients,
healthcare providers, and the healthcare system as a
whole. Therefore, there is a pressing need to reinforce
measures aiming at shielding health data from
IT-enabled privacy breaches. One of the first steps in
this endeavour is for researchers and practitioners to
understand the nature and the patterns underlying the
health data breaches. The premise here is that
different data breach patterns would require security
measures that may vary from one pattern to another.
In this study, we analyze the reported health data
breaches affecting at least 500 individuals published
Uwizeyemungu, S. and Poba-Nzaou, P.
Privacy with Health Information Technologies: What Story Do Data Breaches in US Tell Us?.
DOI: 10.5220/0008977301310141
In Proceedings of the 6th International Conference on Information Systems Security and Privacy (ICISSP 2020), pages 131-141
ISBN: 978-989-758-399-5; ISSN: 2184-4356
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
131

by the US Department of Health and Human Services
(DHHS). Our first aim is to examine the main
characteristics of health data breaches: what is the
nature of breaches, and where are they likely to occur.
Otherwise stated, we want to outline in which form,
and where patient’s protected health information is
most vulnerable. Our second aim is to assess to what
extent meaningful patterns can be drawn from US
health data breaches based on their type and location.
2 BACKGROUND
2.1 The Meaningful Use of HIT
In the United States (U.S.), the federal legislation
encourages the meaningful use of electronic health
records (EHRs), through notably the 1996 Health
Insurance Portability and Accountability Act
(HIPAA) and the 2009 Health Information
Technology for Economic and Clinical Health
(HITECH) Act. The “meaningful use” criteria
intended to encourage hospitals to achieve a
significant level of IT in healthcare processes capable
of spurring the improvement of quality, safety, and
efficiency of patient health information.
The financial incentives for eligible healthcare
services providers were intended to alleviate the cost
burden associated with the EHR implementation
considered as a major impediment to EHR adoption
and use (Hogan & Kissam, 2010a). It seems that this
legislation has attained its objective of spurring EHR
adoption, at least for hospital settings. Different
studies (Adler-Milstein & Jha, 2017; Walker, Mora,
Demosthenidy, Menachemi, & Diana, 2016; Wolf,
Harvell, & Jha, 2012) comparing HITECH-eligible
hospitals with non eligible hospitals noted higher
adoption rates of electronic health records (EHR) for
eligible hospitals following the HITECH incentives’
implementation. According to the Office of the
National Coordinator for Health Information
Technology, as of 2016, “over 95% of hospitals
eligible for the Medicare and Medicaid EHR
Incentive Program have achieved meaningful use of
certified health IT” (ONC, 2018). Even though this
rate indicates a high adoption rate of health IT, it
should be interpreted with caution. First of all, that
rate accounts for only eligible hospitals. It thus
excludes a large part of the U.S. healthcare sector that
comprises inpatient rehabilitation hospitals, inpatient
psychiatric hospitals, long-term acute care hospitals,
3
https://www.hipaajournal.com/what-is-protected-health-
information/
and other healthcare services providers such as
nursing homes, and home health agencies (Wolf et al.,
2012). Secondly, the ONC statistic does not include
small and independent practitioners whose HIT
adoption rates remain significantly lower even when
they are eligible for the meaningful use incentive
program (Hsiao, Decker, Hing, & Sisk, 2012). In spite
of discrepancies in HIT adoption rates and in HIT’s
meaningfulness use, overall, statistics show trends of
increasing adoption in US hospitals (Adler-Milstein
et al., 2015; Adler-Milstein et al., 2017).
The meaningful use of HIT leads to the
digitization of healthcare, which has to be
accompanied by IT-security measures. However,
experts agree that the implementation of IT security
measures is not keeping pace with the
computerization of the health sector (Kruse,
Frederick, Jacobson, & Monticone, 2017). Many
small-and medium-sized healthcare organizations
tend to not undertake significant IT security programs
due to limited human and financial resources; and
implementing security and privacy measures in large
healthcare organizations may take a lot of time due to
managerial and structural rigidity of large systems
(Uwizeyemungu, Poba-Nzaou, & Cantinotti, 2019).
The absence, the insufficiency, and/or the inadequacy
of IT-related security and privacy practices in
healthcare organizations, despite increasing HIT
adoption, may explain the data breaches that are
occurring.
These IT-related security and privacy practices
cover a wide range of measures: access control, data
storage, data anonymization, data encryption, IT
security training, etc. IT security training of all human
resources is particularly important, as data breach is
also a human issue: the majority (58%) of recent data
breaches are due to internal actors whose actions
encompass both human error and misuse
(Chernyshev, Zeadally, & Baig, 2019). Training
helps increase awareness, promote secure behaviour,
and avoid or limit human errors.
2.2 HIT and Privacy Breaches
The notion of “protected health information” (PHI) is
key to ensuring the privacy in the context of
healthcare delivery. It refers to “health data created,
received, stored, or transmitted by HIPAA-covered
entities and their business associates in relation to the
provision of healthcare, healthcare operations and
payment for healthcare services”
3
. The definition
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
132

goes on to precise that PHI “includes all individually
identifiable health information” and gives some
details of that information: “demographic data,
medical histories, test results, insurance information,
and other information used to identify a patient or
provide healthcare services or healthcare coverage”.
Although the definition provides details that reflect
the scope of the information covered, it is at the same
time limiting in its very essence by its insistence on
“individually identifiable health information”. This
qualification refers to the notion of “personally
identifiable information” (PII) that experts argue it has
become meaningless (Hiller, 2016; Milne, Pettinico,
Hajjat, & Markos, 2017): the availability of powerful
IT-enabled algorithms allow to accurately identify
people by combining multiple seemingly harmless data
and / or by tapping multiple sources. In addition, health
information is a potential target for collection by an
array of organizations not subject to stringent
regulation or oversight (Libert, 2015). These
organizations include businesses in data broker
industry, retailers that would gather some health
information indirectly through the customer’s
purchases of health-related products, or even
healthcare organizations whose activities do not place
them under the HIPAA jurisdiction or under similar
rules.
The nature of PHI makes it very sensitive and
very attractive for marketing or criminal purposes.
Different practitioners in the healthcare sector
(physicians, hospitals, pharmacies, insurers) and
outside (such as advertising agencies) are interested
in harvesting health information for marketing
purposes, and in spite of an apparent stringent
legislation, “loopholes exist where consumers’
private health information is ‘up for sale’” (Levy &
Royne, 2009, p. 466).
In addition to this interest for marketing purposes,
health data are particularly attractive to
cybercriminals. In the underground market,
healthcare records are generally more valuable than
other types of data including financial data (Ablon,
2018; McNeal, 2014). The attractiveness of health
information on black markets is justified by the
multiple types of crime that are possible with such
data (Chernyshev et al., 2019): financial fraud,
identity theft, access to healthcare services for non-
insured patients, access to drug prescription,
vindication, extortion, etc. In 2013, health data
accounted for 44% of all identity thefts reported in the
US, and were far costlier than breaches in retail or
financial sectors (McNeal, 2014).
Consequences of health data breaches cover a
wide range of effects of various gravity and may
affect all the stakeholders in the healthcare system.
The most disastrous consequence is arguably the
compromission of patient safety (e.g. Sametinger,
Rozenblit, Lysecky, & Ott, 2015). Patients may also
suffer consequences due to identity theft (then used
for fraudulent activities for instance), they could be
exposed to financial losses, to psychological
discomforts like mental anguish or embarrassment,
loss of trust, etc. Statistics from 2017 show that two
thirds of patients (66%) express concerns about the
safety of their medical records in the context of
electronic health information exchange (ONC, 2018).
According to the same statistics, these concerns lead
10% of individuals to withhold information from their
healthcare providers.
For healthcare providers, they may experience
damages to their reputation that would result in loss
of patients’ trust, confidence, and loyalty, in addition
to being subject to liabilities (damages and fines) that
would put their operational capabilities under duress.
For the healthcare system and public health, if health
data breaches lead patients and healthcare providers
to turn away from HIT usage, the advantages related
to the meaningful use of HIT represent missed
opportunities (Agno & Guo, 2013). This means that
the healthcare system would deliver services of sub-
optimal quality, with less effectiveness, less
efficiency. There are also some risks with regard to
public health: in addition to patients avoiding care,
the contagious disease reporting and treatment system
would be affected, as well as the sharing of data for
health surveillance and for research and education
(Myers et al., 2008): stringent restrictions and
impediments to the sharing of health data may come
as a reaction to the spread of data breaches.
In the US, the same legislation that promotes the
meaningful use of health IT contains provisions
meant to uphold the privacy of “protected health
information” (PHI). This legislation makes it
mandatory to report any privacy breach that affect
500 or more persons. Data gathered following this
legislation can give us valuable insights on the nature
and patterns of health data breaches.
3 METHODS
3.1 Data Source and Sample
Following the requirements of the HITECH Act, the
Office of Civil Rights (OCR) of the US Department
of Health and Human Services (DHHS) maintains an
online database on “breaches of unsecured protected
health information affecting 500 or more individuals”
Privacy with Health Information Technologies: What Story Do Data Breaches in US Tell Us?
133

(HHS Office for Civil Rights, 2018). The database
recorded its first reported breaches in October 2009.
We gathered these data from the OCR website and
used them as our main material. As of December 31,
2018, the database reported a total of 2530 cases of
breach comprised of two categories: 402 breaches
reported within the preceding 24 months and that
were still under investigation by the OCR, and 2128
archived cases of breach, that is all resolved breach
reports and/or reports that were older than 24 months.
In order to better assess the extent of breaches in
terms of the number of incidents and the number of
individuals affected, we took into account data on the
number of hospitals and the size of the population by
state. For the data on the number of hospitals by state,
we used statistics from the 2016 annual survey
database of the American Hospital Association
(AHA). For the population estimates we used the
2017 statistics from the US Census bureau.
In addition to providing information about the
name and the type of the health organization breached
and the state to which it belongs, the OCR data
characterize each breach in terms of type, location (or
mode), the number of individuals affected, as well as
the date of breach submission. The type of breach
refers to the nature of the event that caused the
exposure of the protected health information, and
includes 7 categories, namely 1) hacking/IT incident,
2) improper disposal, 3) loss, 4) theft, 5) unauthorized
access/disclosure, 6) unknown, and 7) other. The
location of breach refers to the tool from which
originated the unauthorized disclosure of the PHI, and
includes 8 following categories: 1) desktop computer,
2) electronic medical record, 3) email, 4) laptop, 5)
network server, 6) other portable electronic device, 7)
paper/films, and 8) other. There are 4 types of health
organizations considered: 1) health plan (335;
13.2%), 2) healthcare clearing house (4; 0.2%), 3)
healthcare provider (1828; 72.3%), and 4) business
associate (363; 14.3%).
3.2 Data Analysis
In order to present a portrait of health data breaches,
we analyze descriptive statistics of breaches. We also
performed a cluster analysis using as clustering
variables a combination of different types and
locations of breaches. However, in order to avoid
meaningless results, we excluded from clustering
variables some under-specified types or locations of
breaches. From the 7 categories of the type of breach,
we excluded categories 6) “unknown”, and 7)
“other”. From the 8 categories of the location of
breach, we excluded categories 7) “paper/films” and
8 “other”. The paper/films” category was excluded as
our study is about IT-related breaches. The other
categories (unknown, other) were excluded
considering that they do not bring about any
exploitable information. Considering the data at hand,
we used the two-step clustering algorithm. This
clustering algorithm is applicable for large data sets,
accepts continuous and categorical variables, and
moreover, it can automatically suggest the optimal
number of clusters (Bittmann & Gelbard, 2007).
Besides, when compared to other clustering
algorithms, the two-step algorithm was the top-
ranked (Gelbard, Goldman, & Spiegler, 2007). The
algorithm suggests a three-cluster solution, which
was confirmed by a discriminant analysis.
4 RESULTS
4.1 The Overall Portrait of Breaches
Overall, we analyzed 2530 breaches reported between
October 2009 and December 2018, affecting
approximatively 261.9 million records. As illustrated
in Figure 1, the number of breaches is globally on the
rise, as well as the number of individuals affected. If
one excludes the incomplete year of 2009, 2,512
breaches are recorded over a 9-year period and over
194.5 million records are affected, that is an average
number of 279 breaches per year, with 21.6 million
individuals annually affected.
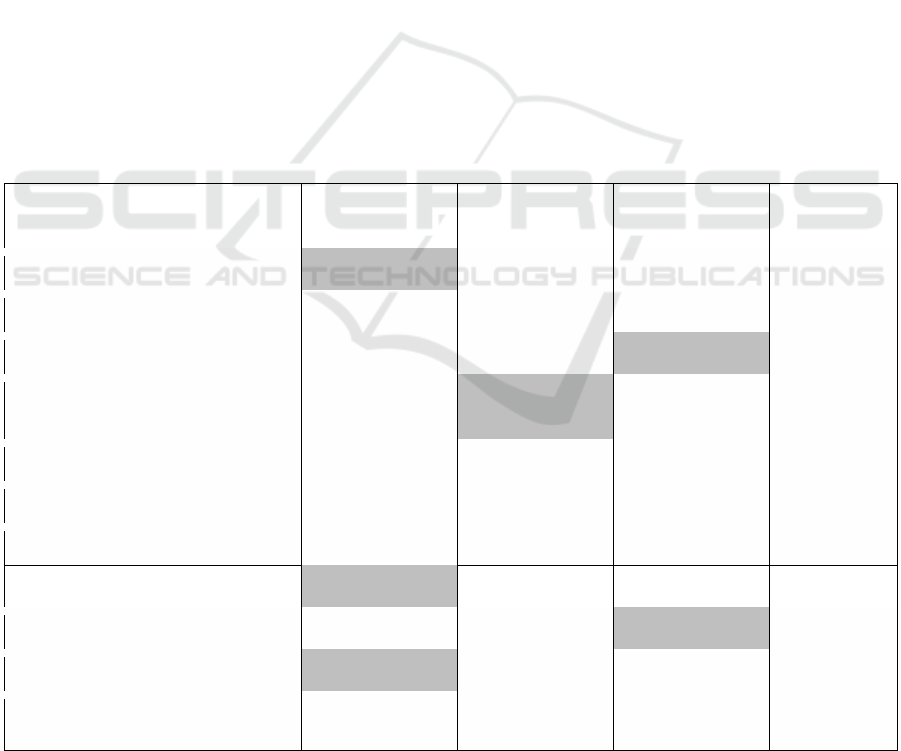
We present in Figure 2 the overall number of
breaches and the overall number of individuals
affected by type of breach. In some cases, a breach
can combine more than one type. For example, a theft
may occur following an improper disposal of a device
containing sensitive healthcare information. Thus, the
total number of breaches by type of breach is 2,642
instead of 2,530 breaches recorded in figure 1. From
Figure 2, it appears that theft is the most frequent cause
of health data breaches (905; 34.3%), closely followed
by unauthorized access/disclosure (769; 29.1%), and
hacking/IT incident (580; 22.0%). However, when one
considers the number of individual records affected by
breaches, the type of breach that has affected so far the
highest number of individuals is by far the hacking/IT
incident (145.6 million; 74.3%).
With regard to the location of breach, Figure 3
shows that the three most prevalent breaches occur
from paper/films (608; 20.5%), network server (511;
17.3%), and laptops (430; 14.5%). The most
significant breaches regarding the number of
individuals affected occur from network servers
(150.3 millions; 68.4%).
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
134

The distribution of breaches according to
affected entities (Figure 4)
shows
that
if
most
breaches
occur
at healthcare provider level (1825;
72.2%),
breaches
occurring
from
health
plans
are
the ones that involve the higher numbers of
individuals affected: health plan related incidents
represent 13.3% of all breaches but they represent
58.2% of individuals affected.
Figure 1: Evolution of Health Data Breaches (Numbers of Breaches and Individuals Affected).
Figure 2: Number of Breaches and Number of Individuals Affected by Type of Breach.
18
199
200
218
278
314
268
327
359
349
134,773
5,932,276
13,162,158
2,854,525
7,022,786
17,452,393
113,269,510
16,655,090
5,138,179
13,020,821
0
100
200
300
400
0
30,000,000
60,000,000
90,000,000
120,000,000
2009 2010 2011 2012 2013 2014 2015 2016 2017 2018
NumberofBreaches
NumberofIndividualsAffected
NumberofBreaches NumberofIndividualsAffected
18
82
98
190
580
769
905
2,253,197
1,332,666
1,482,662
8,143,212
145,621,322
11,734,547
25,452,051
0
40,000,000
80,000,000
120,000,000
160,000,000
0
250
500
750
1000
Unknown
Improper
Disposal
Other
Loss
Hacking/
ITIncident
Unauthorized
Access/Disclosure
Theft
NumberofIndividualsAffected
NumberofBreaches
NumberofBreaches IndividualsAffected
Privacy with Health Information Technologies: What Story Do Data Breaches in US Tell Us?
135
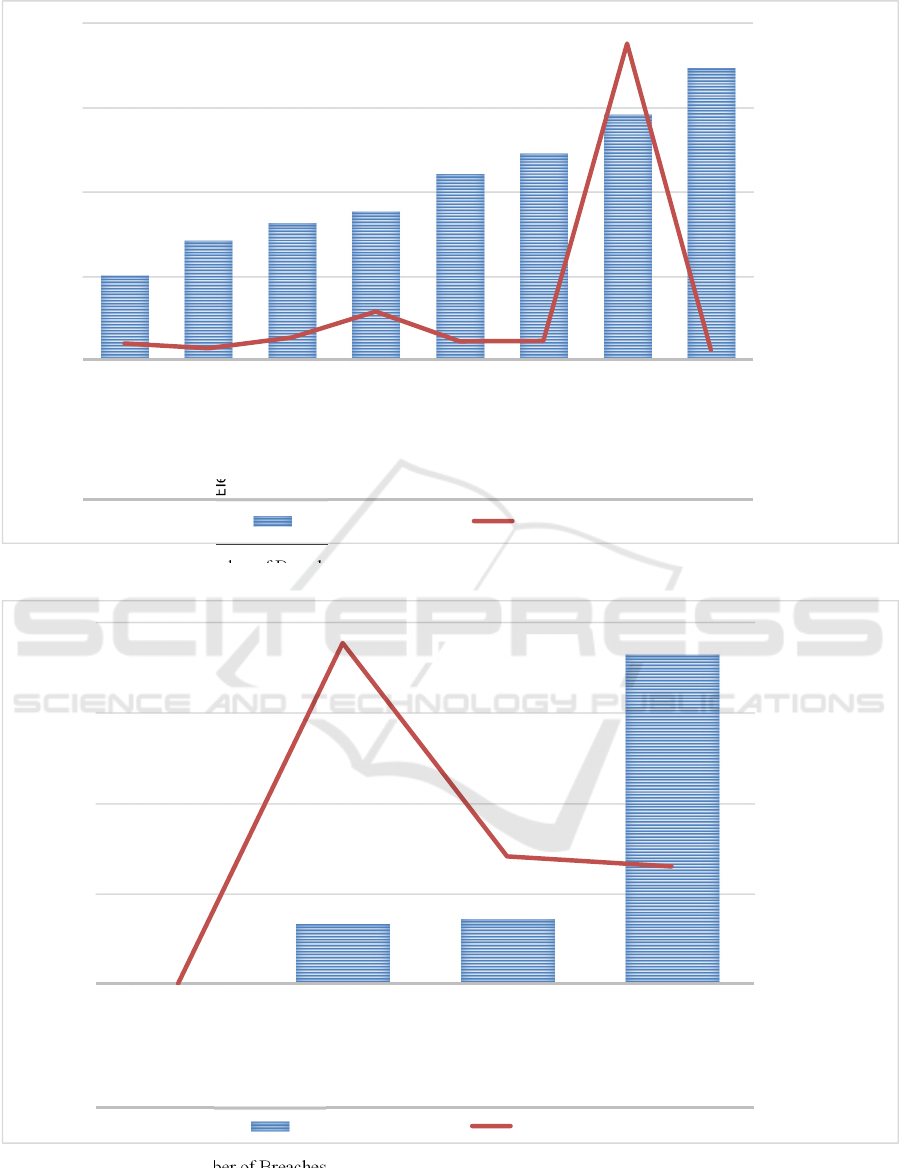
Figure 3: Number of Breaches and Number of Individuals Affected by Location of Breach.
Figure 4: Number of Breaches and Number of Individuals Affected by Type of Covered Entity.
178
249
286
310
388
430
511
608
7,767,041
5,506,102
10,642,612
22,951,685
8,796,507
8,988,573
150,340,496
4,781,501
0
40,000,000
80,000,000
120,000,000
160,000,000
0
175
350
525
700
EMR
OtherPortable
ElectronicDevice
Desktop
Computer
Other
Email
Laptop
Network
Server
Paper
/Film
NumberofIndividualsAffected
NumberofBreaches
NumberofBreaches IndividualsAffected
4
335
363
1,825
17,754
113,315,826
42,318,695
38,969,455
0
30,000,000
60,000,000
90,000,000
120,000,000
0
500
1,000
1,500
2,000
Healthcare
ClearingHouse
HealthPlan
Business
Associate
Healthcare
Provider
NumberofIndividualsAffected
NumberofBreaches
NumberofBreaches IndividualsAffected
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
136

4.2 Most Severe Breaches
The year 2015 has set a record of over 113 millions
records breached. The severest single breaches with
regard to the number of individuals affected occurred
in 2015 at Anthem Inc. from Indiana (78.8 millions), at
Premera Blue Cross in Washington (11 millions), and
at Excellus Health Plan Inc. in New York State (10
millions).
4.3 Breaches by State
Analyzing health data breaches by state, one notes
that the states that come ahead in terms of the number
of breaches are California (286), Texas (213), Florida
(164), New York (140), and Illinois (125). In terms of
individuals affected, the states that registered more
than ten million of individuals affected are Indiana
(84.7 millions), New York (17.3 millions),
Washington (11.8 millions), Tennessee (11.5
millions), and California (10.1 millions).
However, it is worth noting that these numbers may
depict an “unfair” portrait of each state, considering
that (1) the different state healthcare systems are not of
the same size, and (2) the US population is not evenly
distributed across all the US states. Thus, all other
things remaining equal, one would expect much more
data breaches in states with larger healthcare systems,
and more individuals affected in states with more
people. To alleviate discrepancies stemming from the
variation in the size of healthcare systems and
population across states, we weighted the number of
breaches by the number of registered hospitals (a proxy
measure for the size of healthcare system), and we
weighted the number of individuals affected by the
population census (base 2017). Figure 5 presents the 15
states that come ahead in number of data breaches
when one takes into account the size of each state’s
healthcare system. Rhode Island comes ahead with
more than one breach by registered hospital.
Figure 6 presents the 15 states that come ahead in
number of individuals affected by breaches when one
considers each state’s population size. In this case, the
state of Indiana comes far ahead of the other states.
4.4 Results of Clustering Analysis
We present in Table 1 the results of the clustering
procedure described in the method section. As we used
dichotomous measures (1/0) to determine the type or
location of each breach, the means presented in Table
1 give us at the same time the percentages of breaches
for each type or location. We have highlighted
characteristics that stand out (represented in more than
30% of the cases) for each cluster. The results in Table
1 are graphically depicted in Figure 7.
Figure 5: 15 States with Higher Number of Breaches by
Registered Hospital.
Figure 6: 15 States with Higher Number of Individuals
Affected by Breaches (Weighted by Population Census).
From Table 1 and Figure 7, we can see that there
are three well-separated patterns of health data
breaches (3 clusters). In the first cluster (22.9% of all
breaches), we find breaches that are mainly related to
hacking / IT incident (99.7%), either through network
server (59.2%) or e-mail (32.1%) compromission. The
main characteristic of breaches in cluster 2 (29.6% of
all breaches) is that they are all due to unauthorized
access / disclosure (100%). The largest cluster, cluster
3 (47.5% of all breaches) groups breaches whose
characteristic is that they are mainly due to theft
(73.1%). It is not surprising that it is in this last cluster
Privacy with Health Information Technologies: What Story Do Data Breaches in US Tell Us?
137
that we find the relatively higher proportion of
breaches of data on laptops (32.3%).
In Table 2, we breakdown the breaches in our
different clusters according to the type of covered
entities. Otherwise stated, we used the type of
covered entity as control variable. We can infer from
this figure that compared to other clusters, cluster 2
distinguishes itself by the fact that the portion of
health plan entities in that cluster is statistically more
present. The other two clusters have statistically
comparable portions of healthcare provider entities.
5 IMPLICATIONS AND
CONCLUSION
In this study, we present a portrait of health data
breaches in the United States of America, based on
public data published by the US Department of
Health and Human Services (DHHS) in compliance
with the requirements of the 2009 Health Information
Technology for Economic and Clinical Health
(HITECH) Act.
It is preoccupying to note that health data breaches
are not diminishing, and that individuals affected are
counted in millions every year. Given the gravity of
consequences that health data breaches entail, it is
important to understand their characteristics and the
context in which they occur. This study contributes to
this endeavour.
From a practical standpoint, our study will likely
help IT security professionals in healthcare settings to
prioritize their actions. Our results highlight the most
prevalent events (types of breaches) that cause the
exposure of the protected health information (PHI),
as well as the vehicles (locations of breaches) through
which the PHI is most likely to be breached. As our
results show that the highest number of health data
breaches is due to theft, it would be sensible to
prioritize IT security practices aiming at avoiding
theft in order to reduce the occurrence of data
breaches. And, not surprisingly, our cluster analysis
shows that theft is somehow related to laptops. Hence
IT security practices aiming at securing laptops (and
other portable electronic devices) and data they
contain should be prioritized. As it would be naïve to
expect that health data thieves will be less active in
Table 1: Patterns of Health Data Breaches in the US.
Cluster 1
(n=579; 22.9%)
Cluster 2
(n=749; 29.6%)
Cluster 3
(n=1202; 47.5%)
Anova
F
TB - Hacking / IT Incident 0.997
a
0.003
b
0.001
b
111,998.703*
TB - Loss 0.002
b
0.004
b
0.155
a
113.861*
TB - Theft 0.007
c
0.029
b
0.731
a
1,544.746*
TB - Unauthorized Access /
Disclosure
0.016
b
1.000
a
0.009
b
32,963.263*
TB - Improper Disposal 0.000
b
0.003
b
0.067
a
44.035*
LB - Desktop Computer 0.150
a
0.059
b
0.129
a
16.727*
LB - EMR 0.069
b
0.131
a
0.033
c
34.463*
LB - Email 0.321
a
0.215
b
0.034
c
156.742*
LB - Laptop 0.036
b
0.028
b
0.323
a
222.846*
LB - Network Server 0.592
a
0.146
b
0.049
c
519.051*
LB - Other Portable Electronic
Devices
0.007
c
0.044
b
0.176
a
86.385*
*
: p < 0.001
a, b, c: Within rows, different subscripts indicate significant (p < 0.05) pair-wise differences between means on Tamhane’s
T2 (post hoc) test.
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
138

Figure 7: Graphic Representation of the Patterns of Data Breaches Resulting from the Cluster Analysis.
Table 2: Breakdown of Clusters According to the Covered
Entity Type.
Cluster 1
(n=579;
22.9%)
Cluster 2
(n=749;
29.6%)
Cluster 3
(n=1202;
47.5%)
Anova
F
Business
Associate
0.126 0.139 0.155 1.40
Health
Plan
0.121
b
0.219
a
0.084
b
38.07*
Health-
care
Clearing
House
0.000 0.001 0.003 0.79
Health-
care
Provider
0.753
a
0.641
b
0.759
a
17.96*
*: p < 0.001
a, b : Within rows, different subscripts indicate significant (p <
0.05) pair-wise differences between means on Tamhane’s T2 (post
hoc) test.
the years ahead, healthcare organizations have the
responsibility to be proactive, either by minimizing
the opportunities available to thieves or by taking
measures that would limit the damage in the event of
successful theft. One way to reduce theft
opportunities, for example, would be to reduce to a
strict minimum the backup of health data on portable
and mobile devices, which are easy to steal. One way
to limit the damage in the event of a successful theft
is to encrypt all health data stored on hard drives. If
healthcare organizations encrypt all sensitive records,
thieves do not get anything of value from the stolen
data, and the privacy of patients is preserved.
Our results also suggest that in order to reduce the
number of individuals affected by health data
breaches, healthcare organizations should prioritize
IT security practices aiming at preventing hacking /
IT incidents, notably by implementing measures
related to the protection of network servers and to the
elimination of unauthorized access / disclosure. The
encryption of records in storage or being transmitted
would limit the damage in case of hacking / IT
incident. Although these measures are important for
all covered entities, health plans should be prioritized
as they are the main source of breaches that affect
more individuals.
There are some limitations that affect the scope of
our study. Obviously, the first limitation comes from
our dataset itself that accounts only for breaches
involving at least 500 individuals, which is the lower
limit fixed by the law for mandatory reporting of the
breach. Breaches under that limit go unreported,
which prevent us from visualizing the whole picture
of health data breaches. Another limitation is that we
Privacy with Health Information Technologies: What Story Do Data Breaches in US Tell Us?
139

did not gather data on individual healthcare
organizations to analyze whether there are some
characteristics of that organizations that can be
correlated with the patterns of data breaches. This is
an interesting research avenue that would allow one
to go further in explaining our results. In the same
vein, in order to better contextualize the breaches
reported from different states, it would be interesting
to complement data from the US DHHS with data on
the states from other sources. For example, it would
be worthwhile to gather data on the specificities of
states with regard to health information exchange
regulations, or with regard to the rates of health IT
adoption; all data that would probably help explain,
or at least contextualize the levels of health data
breaches.
In spite of the limitations stated above, we hope
that this study contributes to a better understanding of
health data breaches related to the use of health IT,
which is a first step to devise IT security and privacy
practices to prevent data breaches from happening.
REFERENCES
Ablon, L. (2018). Data thieves. The motivations of cyber
threat actors and their use and monetization of stolen
data. Santa Monica, Ca: Rand Corporation.
Adler-Milstein, J., DesRoches, C. M., Kralovec, P., Foster,
G., Worzala, C., Charles, D., . . . Jha, A. K. (2015).
Electronic health record adoption in US hospitals:
Progress continues, but challenges persist. Health
Affairs, 34(12), 2174-2180.
Adler-Milstein, J., Holmgren, A. J., Kralovec, P., Worzala,
C., Searcy, T., & Patel, V. (2017). Electronic health
record adoption in US hospitals: The emergence of a
digital “advanced use” divide. Journal of the American
Medical Informatics Association, 24(6), 1142-1148.
Adler-Milstein, J., & Jha, A. K. (2017). HITECH Act drove
large gains in hospital electronic health record
adoption. Health Affairs, 36(8), 1416-1422.
Agno, C. F., & Guo, K. L. (2013). Electronic health
systems: Challenges faced by hospital-based providers.
The Health Care Manager, 32(3), 246-252.
Bittmann, R. M., & Gelbard, R. M. (2007). Decision-
making method using a visual approach for cluster
analysis problems; indicative classification algorithms
and grouping scope. Expert Systems, 24(3), 171-187.
Blumenthal, D. (2009). Stimulating the adoption of health
information technology. The New England Journal of
Medicine, 360(15), 1477-1479.
Blumenthal, D. (2011). Implementation of the federal
health information technology initiative. The New
England Journal of Medicine, 365(25), 2426-2431.
Chernyshev, M., Zeadally, S., & Baig, Z. (2019). Healthcare
data breaches: Implications for digital forensic readiness.
Journal of Medical Systems, 43(1), 1-12.
Daniel, O. U. (2018). Effects of health information
technology and health information exchanges on
readmissions and length of stay. Health Policy and
Technology, 7(3), 281-286.
Gelbard, R., Goldman, O., & Spiegler, I. (2007).
Investigating diversity of clustering methods: An
empirical comparison. Data & Knowledge
Engineering, 63(1), 155-166.
HHS Office for Civil Rights. (2018). Breach portal: Notice
to the secretary of HHS breach of unsecured protected
health information. Retrieved from
https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
Hiller, J. S. (2016). Healthy predictions? Questions for data
analytics in health care. American Business Law
Journal, 53(2), 251-314.
Hogan, S. O., & Kissam, S. M. (2010). Measuring
meaningful use Health affairs (Project Hope), April
2010, Vol.29 (4), pp.601-6. Health Affairs, 29(4), 601-
606.
Hsiao, C.-J., Decker, S. L., Hing, E., & Sisk, J. E. (2012).
Most physicians were eligible for federal incentives in
2011, but few had EHR systems that met meaningful-
use criteria. Health Affairs, 31(5), 1100-1007.
Jones, E. B., & Furukawa, M. F. (2014). Adoption and use
of electronic health records among federally qualified
health centers grew substantially during 2010-12.
Health Affairs, 33(7), 1254-1261.
Koczkodaj, W. W., Mazurek, M., Strzałka, D., Wolny-
Dominiak, A., & Woodbury-Smith, M. (2019).
Electronic health record breaches as social indicators.
Social Indicators Research, 141(2), 861–871.
Kruse, C. S., Frederick, B., Jacobson, T., & Monticone, D.
K. (2017). Cybersecurity in healthcare: A systematic
review of modern threats and trends. Technology and
Health Care, 25(1), 1-10.
Levy, M., & Royne, M. B. (2009). Up for sale: Consumer
medical information. Journal of Consumer Marketing,
26(7), 465-467.
Libert, T. (2015). Privacy implications of health
information seeking on the web. Communications of the
ACM, 58(3), 68-77.
Liu, V., Musen, M. A., & Chou, T. (2015). Data breaches
of protected health information in the United States.
Journal of the American Medical Association, 313(14),
1471-1473.
McKenna, R. M., Dwyer, D., & Rizzo, J. A. (2018). Is HIT
a hit? The impact of health information technology on
inpatient hospital outcomes. Applied Economics,
50(27), 3016-3028.
McNeal, M. (2014). Hacking health care. Marketing Health
Services, 34(3), 16-21.
Milne, G. R., Pettinico, G., Hajjat, F. M., & Markos, E.
(2017). Information sensitivity typology: Mapping the
degree and type of risk consumers perceive in personal
data sharing. The Journal of Consumer Affairs, 51(1),
133-161.
Myers, J., Frieden, T. R., Bherwani, K. M., & Henning, K.
J. (2008). Privacy and public health at risk: Public
health confidentiality in the digital age. American
Journal of Public Health, 98(5), 793-801.
ICISSP 2020 - 6th International Conference on Information Systems Security and Privacy
140

ONC. (2018). Health IT dashboard - Quick stats.
Retrieved from https://dashboard.healthit.gov/
quickstats/quickstats.php
Rozenblum, R., Jang, Y., Zimlichman, E., Salzberg, C.,
Tamblyn, M., Buckeridge, D., . . . Tamblyn, R. (2011).
A qualitative study of Canada’s experience with the
implementation of electronic health information
technology. Canadian Medical Association Journal,
183(5), E281-E288.
Sametinger, J., Rozenblit, J., Lysecky, R., & Ott, P. (2015).
Security challenges for medical devices.
Communications of the ACM, 58(4), 74-82.
Tubaishat, A. (2019). The effect of electronic health records
on patient safety: A qualitative exploratory study.
Informatics for Health and Social Care, 44(1), 79-91.
Uwizeyemungu, S., Poba-Nzaou, P., & Cantinotti, M.
(2019). European hospitals' transition toward fully
electronic-based systems: Do IT security and privacy
practices follow? JMIR Medical Informatics, 7(1), 1-
16.
Walker, D., Mora, A., Demosthenidy, M. M., Menachemi,
N., & Diana, M. L. (2016). Meaningful use of EHRs
among hospitals ineligible for incentives lags behind
that of other hospitals, 2009-13. Health Affairs, 35(3),
495-501E.
Wani, D., & Malhotra, M. (2018). Does the meaningful use
of electronic health records improve patient outcomes?
Journal of Operations Management, 60(4), 1-18.
Wolf, L., Harvell, J., & Jha, A. K. (2012). Hospitals
ineligible for federal meaningful-use incentives have
dismally low rates of adoption of electronic health
records. Health Affairs, 31(3), 505-5013.
Privacy with Health Information Technologies: What Story Do Data Breaches in US Tell Us?
141
