
The Data Quality Index:
Improving Data Quality in Irish Healthcare Records
David Hickey
1a
, Rita O Connor
1b
, Pauline McCormack
1c
, Peter Kearney
1d
, Roosa Rosti
1e
and Rob Brennan
1,2 f
1
School of Computing, Dublin City University, Dublin, Ireland
2
ADAPT Centre, Dublin City University, Dublin, Ireland
Keywords: Data Governance, Data Quality, Healthcare, Data Management.
Abstract: This paper describes the Data Quality Index (DQI), a new data quality governance method to improve data
quality in both paper and electronic healthcare records. This is an important use case as digital transformation
is a slow process in healthcare and hybrid systems exist in many countries such as Ireland. First a baseline
study of the nature and extent of data quality issues in Irish healthcare records was conducted. The DQI model
and tools were then developed, based on established data quality and data governance principles. Evaluation
of the model and tools showed a significant improvement in data quality was achieved in a healthcare setting.
This initial evaluation of the model was against paper healthcare records, but the model can also be used as
part of an electronic healthcare record system.
1 MOTIVATION
In the Irish healthcare system, the patient Healthcare
Record (HCR) is, for the most part, a paper file that
contains all aspects of the patient journey, in as
structured a form as paper will allow. However, by its
very nature, this paper record is hard to manage and
control, varies in the quality of the data therein, and it
is often difficult to follow and to easily understand
(Health Service Executive, 2011). This lack of
governance in paper records can give rise to problems
in providing the best level of care for the patient. It
has been shown that the data quality of healthcare
records has a direct impact on the quality of care
administered (Urquhart et al., 2018) and the time
spent with patients (Fennelly et al., 2020).
Improving patient outcomes is a key driver of
digital transformation of healthcare and these are
based on the introduction of Electronic Healthcare
Records (EHR). These are a longitudinal electronic
record of patient health information generated by one
a
https://orcid.org/0000-0002-9999-5583
b
https://orcid.org/0000-0001-6222-4702
c
https://orcid.org/0000-0001-6502-9996
d
https://orcid.org/0000-0002-9243-3297
e
https://orcid.org/0000-0002-8341-6153
f
https://orcid.org/0000-0001-8236-362X
or more encounters in any care delivery setting
(HIMSS). Advantages of electronic health records are
the closing of gaps present in paper HCRs, and
utilizing standardized data entry controls. A number
of studies on patient medical records (Greenhalgh et
al., 2010) and informatics in patient care over the past
decade suggest a need to ensure that measures are put
in place to safeguard the quality of data in electronic
health records, and include a warning of the potential
for a ‘landslide of poor quality data’ to negatively
impact clinical outcomes (Hussey & Kennedy, 2016).
Others on this journey of digital transformation have
made mistakes which are well reported (Bowman,
2013), and the promise of improvements in data
quality are often not realized (Charnock, 2019). The
most common mistake in digitisation seems to be the
digitalization of the existing analogue process,
leading to embedding of the same data quality
problems into the electronic HCR (EHR). This a key
component of successful EHR deployment is a robust
design for data quality from the architecture phase
Hickey, D., Connor, R., McCormack, P., Kearney, P., Rosti, R. and Brennan, R.
The Data Quality Index: Improving Data Quality in Irish Healthcare Records.
DOI: 10.5220/0010441906250636
In Proceedings of the 23rd International Conference on Enterprise Information Systems (ICEIS 2021) - Volume 2, pages 625-636
ISBN: 978-989-758-509-8
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
625

that takes into account paper record quality as well as
electronic record quality. There is currently a lack of
common frameworks to support the healthcare
industry to achieve this.
The research question studied in this paper is: To
what extent can the introduction of a data quality
governance process for both paper and electronic
healthcare records improve data quality in
healthcare organisations undergoing digital
transformation? Here data quality refers to the quality
dimensions of completeness, validity, accuracy,
consistency, availability and timeliness of the data
(ISO/IEC 25012). Data governance is defined as ‘the
exercise of authority and control (planning,
monitoring and enforcement) over the management
of data assets’ a collection of practices and processes
which help to ensure the formal management of data
assets within an organization (DAMA DMBOK).
The technical approach has been to develop a set
of requirements for joint paper-HCR quality
governance; to validate the nature and extent of the
data quality issues of healthcare records in a typical
Irish healthcare setting; to develop a model for use
with the Healthcare Record that will improve data
quality based on sound data quality governance
methodologies; to build and evaluate tools based on
the model; to iterate the design, based on real-world
testing using a design science approach.
The contribution of this paper is a new framework
for data quality governance in both paper-based and
electronic healthcare records that is suitable for
organisations undergoing digital transformation and
that supports building in quality processes from the
start into the EHR-based system.
The rest of this paper is organised as follows:
section 2 discusses related work, section 3 specifies
our research methodology, section 4 derives system
requirements and discusses a baseline data quality
study, section 5 describes the design of the data
quality index method, section 6 evaluates the system
and section 7 provides conclusions.
2 RELATED WORK
This section discusses electronic healthcare records,
data governance and data quality in the context of
digital transformation of healthcare systems.
2.1 The Electronic Healthcare Record
As technology has become more prevalent people and
organisations have inevitably moved from paper-
based forms of data collection to electronic means.
This is no different in the healthcare sector where a
big push towards the development of electronic
healthcare records has been seen throughout the
world (Stone, 2014). An Electronic Healthcare
Record (EHR) is a digital version of a patient’s paper
file and can be best described as “a longitudinal
collection of electronic health information about
individual patients and populations” (Gunter & Terry,
2005).
Following in the footsteps of many other
countries, Ireland has already begun to digitise the
paper patient healthcare into electronic form (Grogan,
2020). This is recognised in the 2013 Department of
Health & HSE's eHealth Strategy (Health Service
Executive & Dept of Health, 2013) along with the
2017 Committee on the Future of Healthcare
Sláintecare Report (Houses of the Oireachtas, 2017),
which note the potential of eHealth to be the biggest
and most effective driver of change and improvement
of patient outcomes across the health system. The
ability for healthcare professionals and patients to
have access to up-to-date clinical records at the point
of care, can lead to improved decision making,
reduction in errors and higher quality of patient care.
While there has been much research and
associated literature on the topic of the Electronic
Healthcare Record, most of the focus has been on the
technology challenges, data sharing, security
concerns, privacy, decision support, and
improvements in clinical outcomes. Data governance
and data management are themes that were rarely
discussed in relation to the electronic healthcare
record, and data quality is even less frequently
discussed in the literature. Below we provide
highlights of relevant work to date.
2.2 Data Governance
As organisations hold more and more data,
particularly the huge amounts held in electronic
healthcare systems (Fenton et al., 2017), data
governance is an important consideration in deriving
value from the data and in assuring the quality of data.
The data governance quality domain is central in
Khatri and Brown’s data governance model (Khatri &
Brown, 2010). Having reviewed literature related to
designing data governance within an organisation the
Nagle, Sammon and Cleary model of the
“information supply chain (ISC)” (Nagle et al., 2019)
was found to be the most relevant for Irish healthcare
records. This model produced an easy-to-use artefact
(the ISC card) and drove data governance best
practice throughout the information supply chain.
ICEIS 2021 - 23rd International Conference on Enterprise Information Systems
626
The importance of a data governance framework
for electronic healthcare records cannot be
understated. The OECD recommends that
governments should establish a “national health data
governance framework” (Recommendation of OECD
Council on Health Data Governance, 2016) and that
organisations processing personal health data
demonstrate that they meet national expectations for
health data governance. The OECD also set out a
number of recommendations for nations for
establishing this.
A “Guidance for Information Governance” report
produced by the Health Information and Quality
Authority of Ireland (HIQA) (Guidance on
Information Governance, 2012) for healthcare
providers in Ireland highlights the need for data
governance within the healthcare environment.
Interestingly no revisions have been made to the
document since 2012, which again strengthens the
need for further activity in this area and the Irish need
to develop a model in line with our research question
that considers the current state of art, legislation and
practices, which inevitably have developed and
changed in the last eight years.
2.3 Data Quality
The OECD recommendations mention data quality as
an important consideration in implementing
electronic healthcare records and data governance in
relation to this. HIQA in their guidance document
also recognise the importance of data quality and the
effect it has on quality of care and improved
outcomes. This impact on patient outcomes
highlights the importance of data quality to enable the
electronic health record to achieve its aim in
improving quality of care. For example, true system
interoperability in an electronic health record require
data to be of high quality to ensure reliability of the
inter-system communications.
The importance of data quality is also stressed in
an earlier report by Gordon and Greene (Gordon &
Greene, 2014) which argues that healthcare
organisations may be facing “faster incorrect
information” generation through the implementation
of different systems and applications using
inconsistent metrics and generating data in different
formats. This has the potential to create poor quality
data (lack of consistency, understandability,
portability) and data errors where data is shared. If
data is poor quality it has been shown to lead to
inadequate care being provided and therefore worse
patient outcomes. (Guidance on Information
Governance, 2012).
Data quality as presented in the electronic
healthcare record literature has identified specifically
the data quality dimensions of, ‘accuracy,
completeness, consistency, credibility and timeliness
of data’ (Parsons et al., 2012). The importance of
accuracy and completeness show how HCR can
deliver clear advantages through the implementation
of EHRs as forms or schemata with standardised data
entry controls. The traditional paper-based healthcare
record where data is entered manually has been seen
to contribute to data quality issues (Charnock, 2019).
This also contributes to the issue of lower quality
patient care as identified throughout the literature.
The importance of high-quality data in EHRs can also
have legal, social and care impacts as patients’ lives
are at risk where a lack of data accuracy or
completeness presents itself.
Thus it can be seen that there is a deep need for
data quality models that can be used for both the
paper-based and electronic healthcare records. As
digital transformation of healthcare proceeds these
needs are growing due to the increased dependence
on algorithmic IT supports.
3 METHODOLOGY
We took an Agile approach to project management in
order to allow the project team the flexibility to work
within a structured framework, while providing the
flexibility to iterate as the model requirements,
design, testing and evaluation evolved.
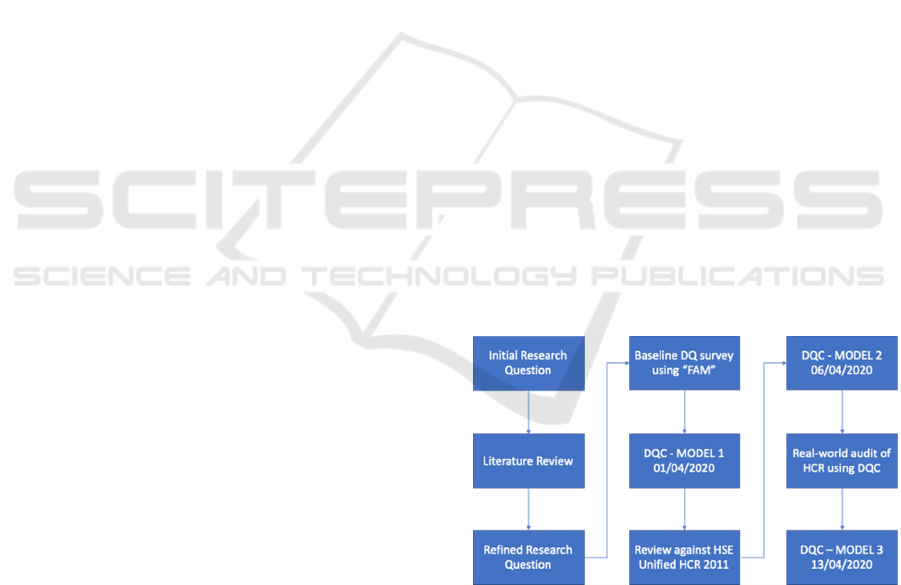
Figure 1: Project management approach.
The main steps were (Figure 1):
Review of previous work and literature;
Identification of Governance Model identified–
‘Decision Domains for Data Governance’
(Khatri and Brown, 2010);
Project focus on Data Quality within the five
domains in that model;
The Data Quality Index: Improving Data Quality in Irish Healthcare Records
627
‘Information Supply Chain’ (Nagle et al.,
2019) used to as the stimulus for our own
model development;
Baseline review of paper HCR using ‘Friday
Afternoon Measurement’ methodology;
(Redman, 2016)
Initial development of Data Quality Card
(DQC) and Data Quality Index (DQI) Model;
Alignment of entities and attributes with HSE
standard led to revised DQI Model (v2);
Simulated Healthcare Record evaluation and
revision of attribute definitions;
Finalisation of DQI Model (v3).
Stakeholder involvement involved a hospital Data
Protection Officer and an Electronic Healthcare
Record Privacy Lead with clinical expertise, a Project
Manager, a Legal expert and Innovation and Design-
Thinking expert. The evaluation methodology used
concepts from the Design Science/Design Thinking
discipline. The Experimental design evaluation
method (Hevner et al., 2004), was applied so that we
could analyse the artefact (our DQI model) in a
controlled environment for utility with regard to data
quality levels.
4 REQUIREMENTS
The target of our study was a robust design for a data
quality governance framework from the architecture
phase of the Irish healthcare HCR that takes into
account paper record quality as well as electronic
record quality. From our evaluation of the state of the
art in data quality for paper-electronic healthcare
records (section 2), we determined that none of this
met the requirements of the current digital
transformation of the Irish healthcare system, and so
we set about developing a new model to address these
issues. The requirements for this data quality
governance model are:
An easy-to-use artefact for non-IT staff;
Applicable to paper and electronic records;
Can be applied historically to provide a quality
score;
Can be used on new records to ensure high
quality;
Capable of being developed into a software
solution for the electronic record;
Ideally applicable to other domains;
Support the Irish Unified Healthcare Record
standard (Table 1);
Addresses the most frequent errors identified in
Irish Healthcare records (Table 2).
Table 1: Unified Healthcare Record (HSE Ireland).
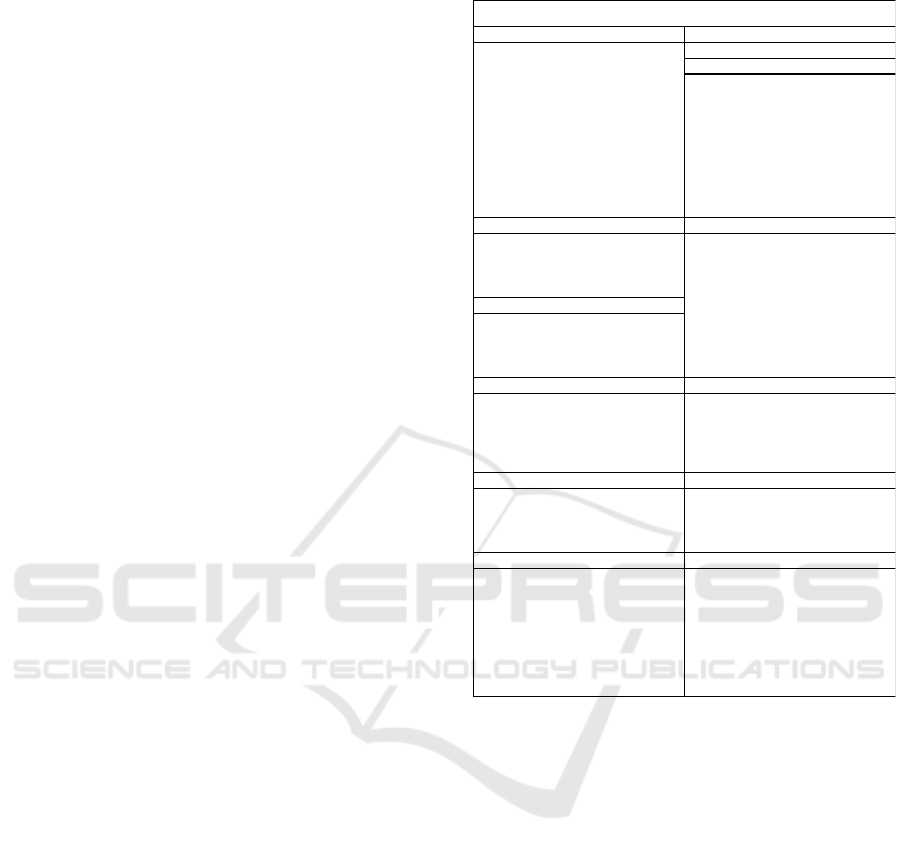
4.1 Baseline Data Quality Study
To quantify the extent of data quality problems to
solve, and to measure its extent, we applied an
approach known as the Friday Afternoon
Measurement (FAM) (Redman, 2016) methodology.
This approach involves reviewing the last 100 data
records created and looking at no more than 10-15
data attributes for each record, and marking obvious
errors. Then counting up the number of error-free
records gives a number from 0 – 100 called the data
quality or “DQ” score.
Our baseline FAM review was carried out based
on a single reference hospital’s HealthCare Record
(HCR). In our baseline review, we got a DQ score of
11 (Figure 2) indicating that there would be only 11
perfect records out of the 100 reviewed. This
confirmed the extent of data quality issues in the
paper healthcare record. This is a low score as 33-67
would be typical scores in baseline studies according
to Redman.
1. Registration 7. Consent
Patient name Consent Forms
DOB 8. Clinical
MRN Cardiovascular
Contact Details Vascular
Gender Neurophysiology
Marital Status Pulmonary
GP Name GIT
Medical Card Urology
Next of Kin Audiology
Admission details EEG
Discharge details
2. Administrative 9. Laboratory
Patient labels Biochemistry
Front sheets Haematology
Relevant Billing Microbiology
Private Insurance Forms Histopathology
3. Correspond ence Immunology
Referral Letters Molecular Diagnosis
Discharge Communications
Ambulance Transfer Sheets
Other Correspondence
4. Clinical Notes 10. Radiology
All clinical not es Diagnostic Imaging Reports
Integrated Care X-Ray
Intensive Care MRI
Emergency Dept PET
Treatment Notes Ultrasound
5. Nursing 11. Medicines
Temp and Obs Sheets Drug Prescribing Sheets
Nursing Care plans Prescriptions
Intensive Care Nursing Nutritional Supplements
Evaluations Blood Transfusion
6. Proced ures 12. Social Care
Procedure Forms Assessment Forms
Anaesthetic R ecords Care Cards
Epidural Records Food Diari es
Implant Records Dietary
Blood Loss Sheets
Instrument Count Sheets
Theatre C hecklists
Theatre Nursing
CATEGORY
ICEIS 2021 - 23rd International Conference on Enterprise Information Systems
628
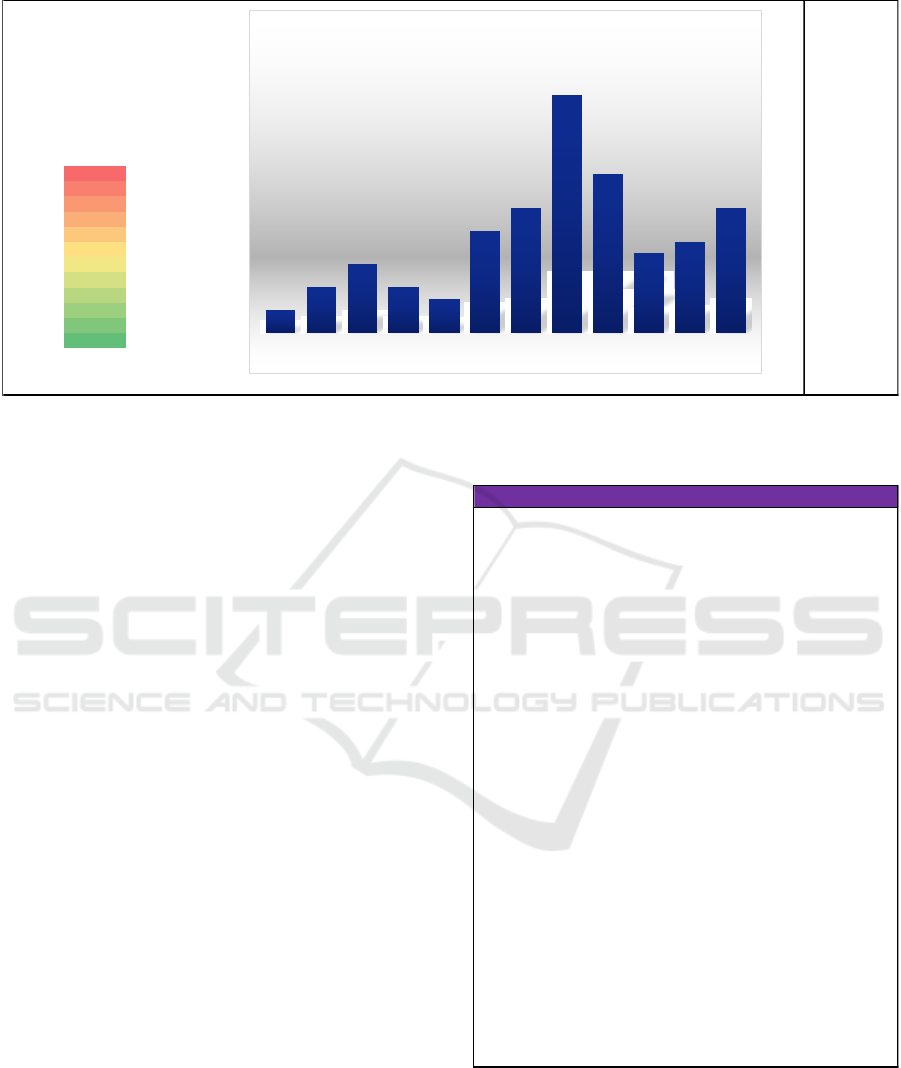
Figure 2: Baseline measurement of data quality in HCR.
We extracted the typical errors from our baseline, and
then compared these with errors that had previously
been identified by the HSE in their review of
Standards for healthcare records management (Health
Service Executive, 2011). This allowed us to arrive at
a “Top 20” of most common data quality issues in the
healthcare record (Table 2). A key requirement for
any data quality method would be to mitigate the
frequency of these types of errors.
5 DATA QUALITY INDEX
METHOD DESIGN
The starting point for our quality method
development was the ISC Card developed by Nagle,
Sammon and Cleary (Nagle et al., 2019). Their
concept provided a Data Governance framework for
people, process and technology covering all stages in
the Information Supply chain.
The basic building block of our model is the
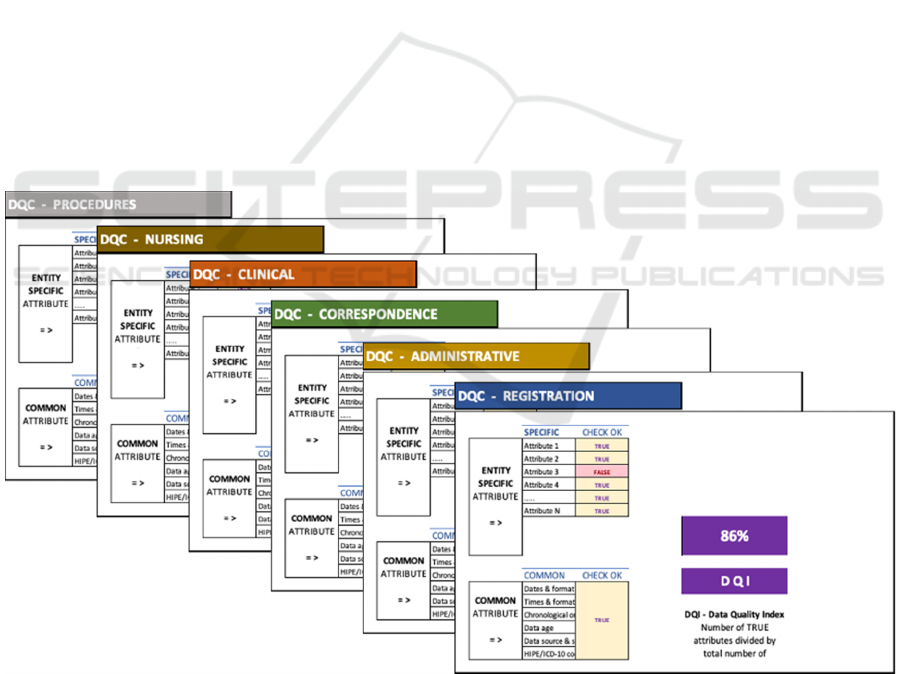
“Data Quality Card” or DQC (Figure 4). The DQC
measures the quality of one entity with many
attributes. Each entity may have a number of
specific attributes which relate only to that entity,
and attributes in common with other entities. Each
attribute on a data quality card is evaluated to see if
it is present and accurate, which gives a “true”
result. Our model then provides a “Data Quality
Index” or DQI for each entity. The DQI is the
percentage of attributes with perfect quality (in
keeping with the FAM methodology).
Table 2: Top 20 errors in Irish HCR.
Our scenario relates to the Healthcare Record. As we
have seen earlier (Table 1), each healthcare record has
a number of discrete sections or entities. In Ireland,
the Unified Healthcare Record (Health Service
Executive, 2011) has 12 standard sections or entities
defined. Applying our DQI Model, one Data Quality
Attributes
Correct % of Paper Records
02%
14%
26%
34%
43%
59%
611%
721%
814%
97%
10 8%
11 11%
DQ
11
2%
4%
6%
4%
3%
9%
11%
21%
14%
7%
8%
11%
01234567891011
Number of Correct Attributes
% of Paper Records
PAPER HCR
1Name o
2DOB o
3MRN o
4 Missing patient label X
5 Address (physical or email) X
6Phone No X
7 Dates & format X
8 Times & format X
9 Chronology X
10 Stale data X
11 Clinical data missing X
12 Inacessible at Point of Care X
13 Lost record X
14 Forms missing X
15 Transcription error X
16 Illegibility error X
17 Source not identified X
18 Signature missing X
19 Missing "media" X
20 Fragmented record error X
X = Likely to occur
o = Unlikely to occur
TOP DATA QUALITY ISSUES IN PATIENT RECORD
The Data Quality Index: Improving Data Quality in Irish Healthcare Records
629
Card (DQC) is thus created for each entity (or section)
in the healthcare record (Figure 3).
The overall DQI model is then made up of a number
of Data Quality Cards, with each DQC representing
one entity in the scenario being examined – giving 12
cards in our Healthcare Records scenario.
Each DQC has its own DQI score, which allows easy
identification of quality issues at entity and attribute
level. Combining all Data Quality Cards then
provides the overall model with a single Data Quality
Index.
DQI =
sum(DQCattributes=true)
(1)
sum(DQCattributes)
In the DQI model, the number of cards, the
number of entities, the entity-specific attributes and
the common attributes are all flexible, which
potentially allows the model to be applied to any data
quality scenario for any sector.
It is intended that a DQC can be used as an artefact
or tool (either printed or electronic) to calculate the
DQI of any individual entity. We have also developed
a simple data entry form for the model, which can be
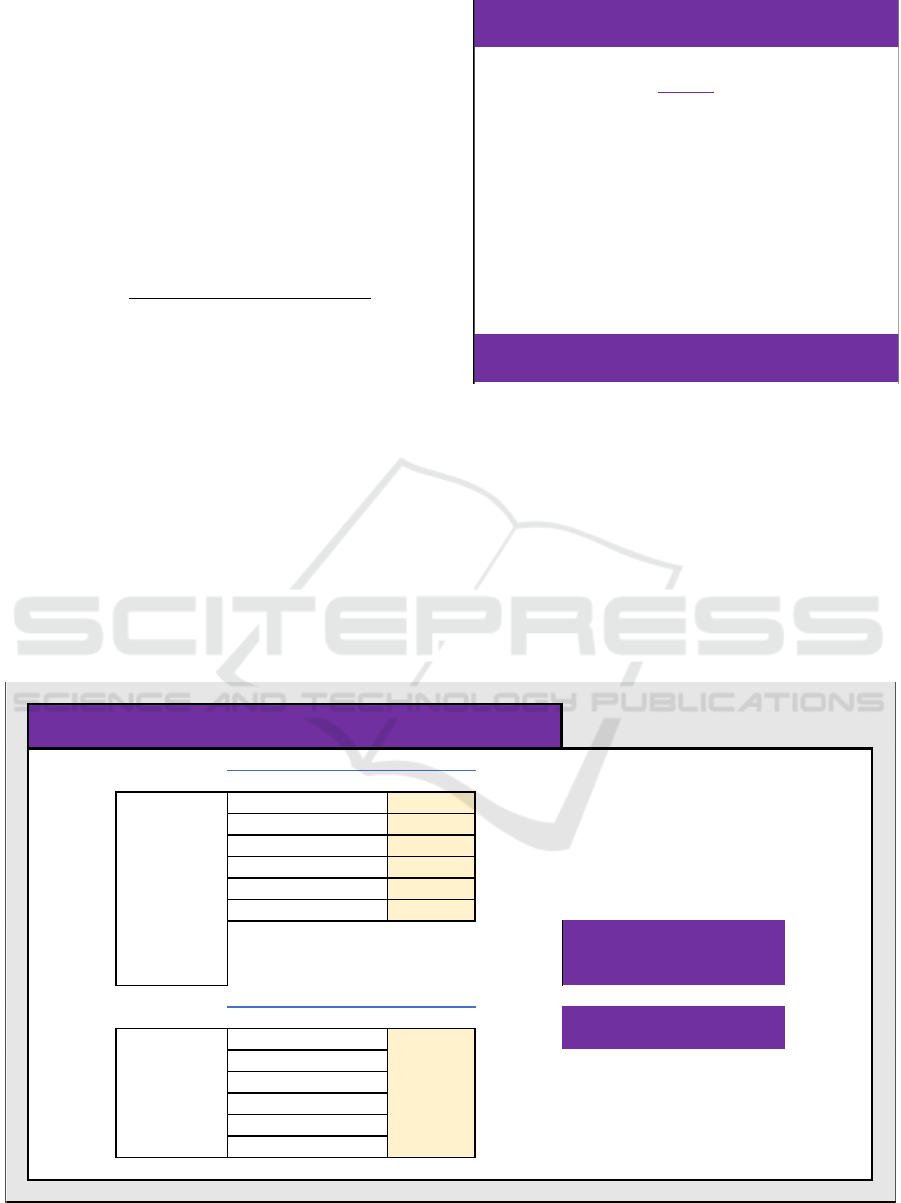
printed or completed electronically (Figure 6).
We envisage this simple data entry form being
used in different ways: firstly, it can be printed out on
a single sheet and used as an audit tool on paper
records; secondly, it can be included as a checklist for
Figure 3: DQI model rules.
new records; finally, it can be used as an interactive
(electronic) checklist to be completed and directly
drive the model giving individual DQI scores for each
entity as well as an overall DQI score for the record.
Finally, the complete DQI Model rolls up the data
from all the constituent Data Quality Cards, into a
single aggregated view (see Figure 7 below). The
complete Model is linked to each underlying DQC
and to the Data Entry Form.
Figure 4: The Data Quality Card (DQC).
RULES
MUTLIPLE ENTITIES PER SCENARIO
MULTIPLE ATTRIBUTES PER ENTIT
Y
SPECIFIC ATTRIBUTES VAR
Y
PER ENTIT
Y
COMMON ATTRIBUTES
F
IXED PER ENTIT
Y
ONE DQC CARD PER ENTITY
MULTIPLE DQC CARDS PER SCENARIO
SPECIFIC CHECK OK
Attribute 1
TRUE
Attribute 2
TRUE
Atrribute 3
TRUE
Attribute 4
TRUE
…..
TRUE
Attribute N
TRUE
COMMON CHECK OK
Dates & format
Times & format
Chronological order
Data age
Data source & signature
HIPE/ICD-10 coding
DQI - Data Quality Index
Number of TRUE attributes
divided by total number of
attributes, as a %
DQC (Data Quality Card) - [ENTITY NAME]
ENTITY
SPECIFIC
ATTRIBUTES
= >
100%
D Q I
COMMON
ATTRIBUTES
= >
TRUE
ICEIS 2021 - 23rd International Conference on Enterprise Information Systems
630
A simple software model was developed for the
project, that allowed the user to see the DQI of each
DQC change in real time as data quality was
evaluated using the data entry form. At the same time,
an overall DQI score was displayed.
This allowed the model to be evaluated, but also
gives users an immediate visualisation of where data
quality issues exist in the underlying record, to an
entity and attribute level.
5.1 DQI Design for the Irish Unified
Healthcare Record
We developed a first version of the DQI Model based
on the individual hospital HCR studied in our data
quality baseline, and it had 11 entities and 80
attributes. We then reviewed the model to include all
entities in the Unified Healthcare Record. This
resulted in Version 2 of the DQI model which has 12
entities corresponding to the sections in the Unified
HCR, and 100 attributes specified by the HSE. This
now makes the model usable in any healthcare setting
in Ireland. During evaluations (Section 6), we found
a number of form attributes were ambiguous or
lacked clarity and so we redefined these and created
a new (Version 3) of the DQI model.
6 EVALUATION
6.1 Deployment Case Study
First, we consider the impact of deploying data
quality cards (DQC) and the data quality index (DQI)
into manual workflows in the Irish healthcare system.
Manual (paper) Healthcare records are created on an
ad-hoc basis over the duration of a patient’s treatment
lifecycle by different healthcare professionals. These
records are created with varying attention to detail,
regarding the data quality recorded and the format
used. The resultant anomalies and poor data quality
in the healthcare records negatively impacts the
decision-making capabilities of medical staff when
treating patients.
The DQC and DQI Data Entry Form allow (a) a
health care auditor who is assigned the task of
reviewing the data quality of paper-based healthcare
records, to easily generate a Data Quality Index (DQI)
score or measurement for the records on file in an
automated manner; and (b) a health care user to
ensure data quality at the point of entry of the data by
generating a DQI score using either a paper checklist
or an electronic data entry form.
Figure 5: multiple Data Quality Cards make up the DQI model.
The Data Quality Index: Improving Data Quality in Irish Healthcare Records
631
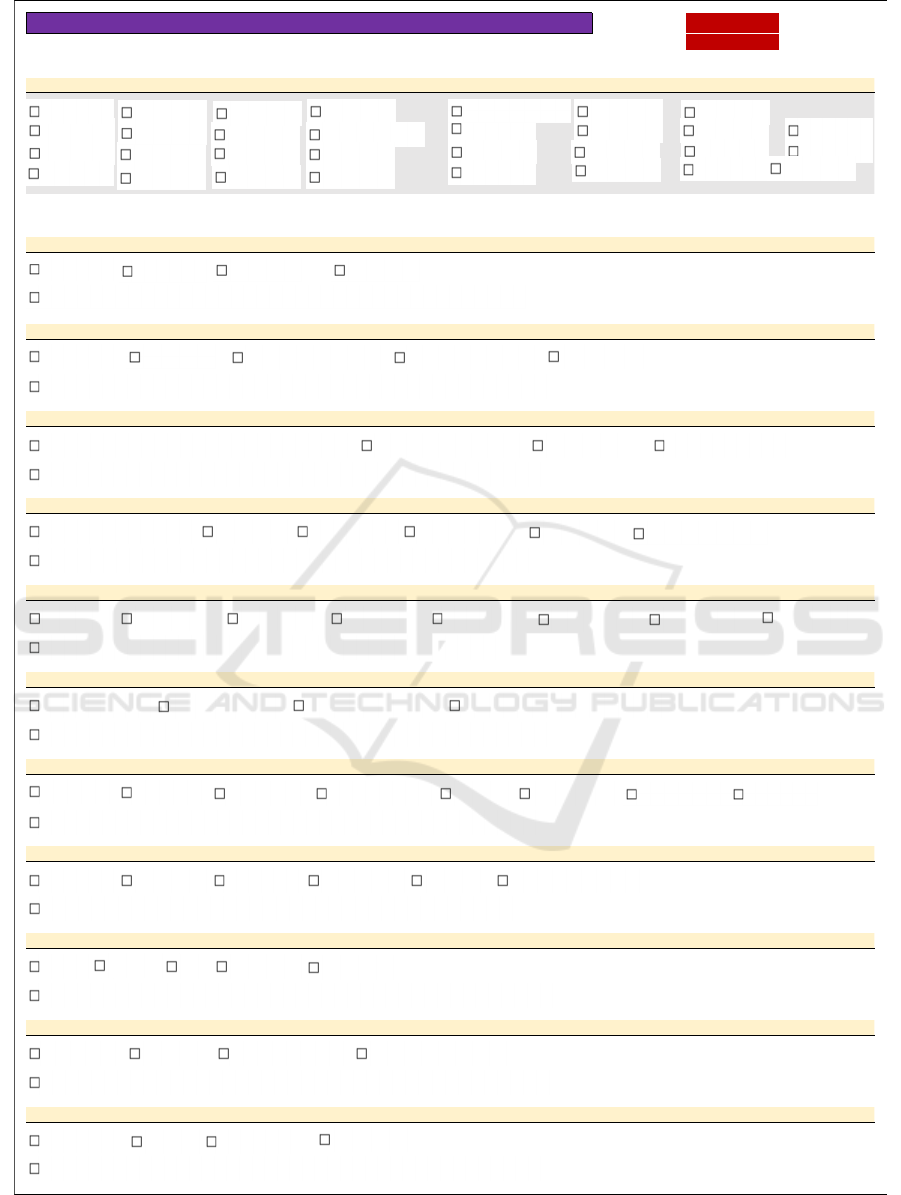
Figure 6: Data entry checklist for the DQI model.
Please check the following (MASTER) Patient Record Details and if accurate or not required, tick the relevant box(es):
MASTER PATIENT RECORD
Please check that the following are present (or not required) and accurate in the patient record, and if so, tick the relevant box(es):
ADMINISTRATIVE SECTION
CORRESPONDENCE SECTION
CLINICAL NOTES SECTION
NURSING NOTES SECTION
PROCEDURES SECTION
CONSENT SECTION
CLINICAL MEASUREMENTS SECTION
LABORATORY RESULTS SECTION
RADIOLOGY AND DIAGNOSTIC IMAGING RESULTS SECTION
PRESCRIBED MEDICINES SECTION
HEALTH & SOCIAL CARE PROFESSIONALS SECTION
DATA QUALITY CARD (DQC) - CHECKLIST FOR PATIENT HEALTHCARE RECORDS DATA ENTRY
12X100
Patient Label
Front Sheet (s)
Billing Information Pr i vate Insurance
Referral Letter(s)
Discharge Communications Ambulance Transfer Sheets
Living Wills
All Clinical Notes including Integrated Care Pathways and ICU notes
Emergency Department Notes Heal t h Care Not es Nurse Specialist Notes
Common attributes (source, retention date, date & time formats, chronological order, signature)
Common attributes (source, retention date, date & time formats, chronological order, signature)
Common attributes (source, retention date, date & time formats, chronological order, signature)
Vital Signs Observations Fluid Balance Nursing Care Plans Intensive Care Notes
Evaluations
Common attributes (source, retention date, date & time formats, chronological order, signature)
Procedure Form s Anaesthetic Forms Epidural Infusion Implant Records Blood Loss Sheets
Swab Count Sh eet s Instrument Count
Theatre Check l ist
Common attributes (source, retention date, date & time formats, chronological order, signature )
Con s en t f orm - Adu l t
Consent form - child
Consent form - research
Common attributes (source, retention date, date & time formats, chronological order, signature)
Cardiovascular
Haemodynamic
Neurophysiology Pulmonary Function GIT Rep o rt s Urology Reports
Audiology Reports EEG Reports
Common attributes (source, retention date, date & time formats, chronological order, signature)
Bi o c h e m i s t r y Haem at o l ogy Microbiology Histopathology Immunology Molecular Diagnostic
Common attributes (source, retention date, date & time formats, chronological order, signature)
X- Ray
CT Scan
MRI Ultrasound
PET Sc a n
Common attributes (source, retention date, date & time formats, chronological order, signature)
Drug Prescribing Prescriptions Nutritional Supplements Blood Transfusions
Common attributes (source, retention date, date & time formats, chronological order, signature)
Assessment
Care Cards Dietary Form
Psychology Report
Common attributes (source, retention date, date & time formats, chronological order, signature)
DOB
MRN
Home address
Phone - mobile
Phone - home
Ph o ne - ot her
Em ai l ad d ress
Next of kin name
Next of kin address
Next of kin phone
Next of kin mobile
PA T I EN T N A M E
Date of admission
Referral source
Date of discharge
Discharged to
Previous address
Gen d er
Marital st atus
Mode of arrival
GP n am e
GP contact details
Medical insurance
Medical card
Mother's maiden name
Religion
Ethnicity
CLINICIAN
Language
School
Accompanied by
Disch arge against medi cal ad vi ce form
Admission Notes
Nat i onal Earl y- w ar n i ng Sco r e
ICEIS 2021 - 23rd International Conference on Enterprise Information Systems
632
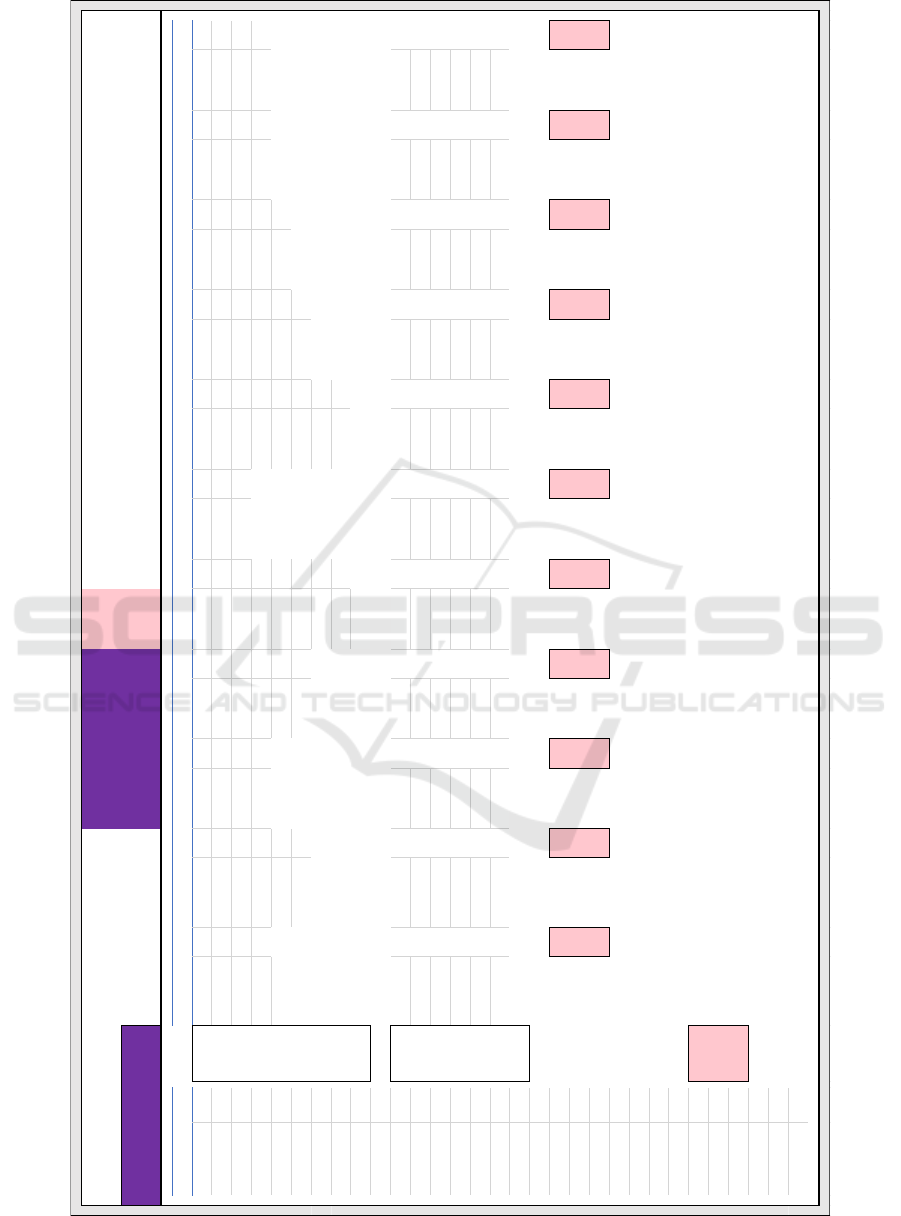
Figure 7: The complete DQI model dashboard for the Irish Unified Healthcare Record (aggregated view).
DATA QUALITY MODEL FOR PAPER RECORDS - DQC (Data Quality Card)
CALCULATION OF DQI (Data Quality Index)
REGISTRATION
< CHECKED
ADMINISTRATIVE
< CHECKED
CORRESPONDENCE
< CHECKED
CLINICAL
< CHECKED
NURSING
< CHECKED
PROCEDURES
< CHECKED
CONSENT
< CHECKED
MEASUREMENT
< CHECKED
LAB RESULTS
< CHECKED
IMAGING
< CHECKED
MEDICINES
< CHECKED
SOCIAL CARE
< CHECKED
Patient Name FALSE
Patient Label FALSE Referral Letters FALSE All Clinical Notes FALSE Vital Signs Obs FALSE Procedure Forms FALSE Consent - Adult FALSE Cardiovascular FALSE Biochemistry FALSE X-R ay FALSE Drug Prescribing FALSE Assessment Forms FALSE
DOB FALSE
Front Sheet FALSE Admission Notes FALSE E mergency Dept FALSE Fluid Balance FALSE Anaesthetic Forms FALSE Consent - Child FALSE Haemodynamic FALSE Haematol ogy FALSE CT S can FALSE Prescriptions FALSE Ca re Cards FALSE
MRN FALSE
Relevant Billing FALSE Discha rge Notes FALSE Health & Social Care FALSE Nursing Care Plan FALSE Epidural Infusion FALSE Consent - R esearch FALSE Neurophysiology FALSE Microbiology FALSE MR I FALSE Nutrional Supl'ment FALSE Dietary FALSE
Gender FALSE
Private Insurance FALSE Am bulance Transfer FALSE Nurse Specialist FALSE ICU Notes FALSE Implant Records FALSE Unadvised discharge FALSE Pulmonary F unction FALSE Hi stopa thology FALSE Ultrasound FALSE Blood Transfusion FALSE Psychology FALSE
Marital Status FALSE
Living Wills FALSE Evaluations
FALSE Blood Loss Sheets FALSE GIT Reports FALSE Immunology FALSE PET Scan FALSE
Home Address FALSE
Early Warning Score FALSE Swab Count Sheets FALSE Urology Reports FALSE MolecularDiagnostic FALSE
Prev ious Addres s FALSE
Instrument Count FALSE Audiology Reports FALSE
Phone - Mobile FALSE
Theatre Checklist FALSE EEG Reports FALSE
Phone - Home FALSE
Phone - Other FALSE
Email Address FALSE
Dates & format Dates & format Dates & format Dates & f ormat Dates & form at Dates & format Dates & form at Dates & form at Dates & format Dates & format Dates & format
Next of Kin Name FALSE
Times & format Times & format Times & format Times & format Times & format Times & format Times & format Times & format Times & format Times & format Times & format
Next of Kin Address FALSE
Chronological order Chronological order Chronological order Chronologi cal order Chronological order Chronological order Chronolog ical order Chronolog ical order Chronological order Chronological orderChronological order
Next of Kin Phone FALSE
Data ag e Data ag e Data ag e Data ag e Data age Data age Data a ge Data age Data age Data age Data age
Next of Kin Mobile FALSE
Data source/signed Data source/signed Data source/signed Data source/signed Data source/signed Data source/signed Data source/signed Data source/signed Data source/signed Data source/signed Data source/signed
Date of Admission FALSE
HIPE/ICD-10 coding HIPE/ICD-10 codi ng HIPE/ ICD-10 coding HIPE/ICD-10 coding HIPE/ ICD-10 coding HIPE/ICD-10 coding HIPE/ICD-10 coding HIPE/ICD-10 coding HIPE/ICD-10 coding HIPE/ICD-10 coding HIPE/ICD-10 coding
Referral source FALSE
Mode of arrival FALSE
Date of Discharge FALSE
Discharged to FALSE
GP Name FALSE
GP Contact details FALSE
Medical Insurance FALSE
Medical Card FALSE
Mothers maiden name FALSE
Religion FALSE
Ethnicity FALSE
Language FALSE
Accompanied by FALSE
School FALSE
Clinician Responsible FALSE
SECTION
SPECIFIC
ATTRIBUTES
= >
COMMON
ATTRIBUTES
= >
FALSE FALSE FALSE
0%
FALSE FALSEFALSE FALSE FALSE FALSE FALSE FALSE
DQC Model (V1.0) based on single Reference-Hospital Healthcare Record
OVERALL DATA QUALITY INDEX
0%0% 0%
DQI 1
0%
DQI 2 DQI 3 DQI 4 DQI 5 DQI 6 DQI 7 DQI 8 DQI 9 DQI 1
0
DQI 11 DQI 1
2
0%
DATA QUALITY CARD (DQC) - 12X100
D
QC Model (V2.0) added 21 attributes from HSE Unified Healthcare Record (Ireland)
DQC Model (V3.0) based on field evaluation of V2.0 and clarification of attributes
0%
0% 0%0% 0%0% 0%
The Data Quality Index: Improving Data Quality in Irish Healthcare Records
633

The benefits are:
Quick identification of the entity / attribute(s)
within the healthcare record where data quality
is a problem;
Automation of the count of erroneous records
which can be cleansed;
Identification of trends in poor data quality can
be easily identified (and recommendations can
be made with regard to how they are readily
fixed);
Creators of new paper healthcare records may
take greater care when completing records, due
to regular data quality audits.
6.2 Domain Expert Validation
In order to quantify the value of the DQC/DQI, a
clinical expert user assessed the utility of them with
regard to the data quality of all components of the
patient record i.e. Registration, Administrative,
Correspondence, Clinical, Nursing, Procedures,
Consent, Measurement etc).
The data quality was measured by using the
Conceptual Framework of Data Quality (Wang &
Strong, 1996) with quality dimensions as follows:
Intrinsic Data Quality refers to the accuracy or
believability of the data;
Contextual Data Quality refers to the data
quality associated with the user’s task and must
be assessed in relation to the purpose of the
work, thereby ensuring that whatever the user
needs is readily available when it is needed;
Representational Data Quality includes aspects
related to the format of the data (concise and
consistent representation) and the meaning of
data (interpretability and ease of
understanding);
Accessibility Data Quality relates to the fact
that a user has access to, and knows how to
retrieve what he/she needs when required to
complete a specific task.
The evaluation methodology was inspired by concepts
from the Design Science/Design Thinking discipline.
The Experimental design evaluation method (Hevner
et al., 2004), was applied so that we could analyse the
artefact in a controlled environment for usability with
regard to data qualities. We evaluated the data quality
of manual health care records regarding the “Top 20”
data quality errors as outlined in Table 2.
The first evaluation of our DQI Model was
conducted by creating new HealthCare Records and
looking for an improvement in data quality. In
creating these records, we used the DQCs to focus on
the “Top 20” errors identified in our FAM review
(See Table 2 above). Using DQI Model V2 at the
point of data entry provided a DQI score of 37%.
We had expected a greater improvement in data
quality, and so we revisited the language and
definitions of each of the (100) attributes used to
measure the DQI index on the form used by the
assessor. When we applied this final version of the
DQI Model, again focussing on checking for the “Top
20” errors, we now found we achieved a significant
improvement in data quality with a DQI of 81%.
The data quality results are outlined in Table 2
below. In transitioning from Iteration 1 (DQI Model
V2) to Iteration 2 of the evaluation (DQI Model V3),
the data quality score improved from 37% of records
being error free to 81% of the records evaluated being
error free. This was achieved by improving the
labelling of fields on the assessment form. One
attribute of contextual data quality, ‘Missing data’
was relabelled to become more accurate and relevant
as ‘Clinical data missing’. From a representational
data quality perspective, three attributes were made
more meaningful and interpretable. These are:
‘Address’ edited to become ‘Address - physical or
email’, ‘Fragmented’ edited to ‘Forms missing’ and
‘Linked Record Error’ edited to become ‘Fragmented
record error’. Finally, one attribute was refined to
highlight the point at which accessibility became an
issue regarding the patient’s treatment, i.e. from
‘record inaccessible’ to ‘inaccessible at point of care’.
Table 3: Summary of evaluation results.
Evaluation DQ
Type
Iteration 1 Iteration 2
Intrinsic
DQI = 31% from
Model v2
DQI = 81% from
Model v3
Contextual
1 x DQ attribute
incomplete
Rename item 11
Representational
3 x DQ attributes
vague for user
Identify item 14
forms missing.
Rename items 5 & 20
Accessibility
1 x DQ attribute
incomplete
Identify item 12
record unavailable
These findings are consistent with our understanding
that high-quality data should be intrinsically good,
contextually appropriate for the task, clearly
represented, and accessible to the user of Healthcare
records. It has also shown that the structured formal
approach of Wang et al. has allowed us to achieve our
goal of measuring data quality in addition to
transforming the data quality facilitated by the use of
DQC/DQI in auditing health care records.
ICEIS 2021 - 23rd International Conference on Enterprise Information Systems
634

6.3 Data Protection/GDPR Benefits
While the focus of the project was not on data
protection and privacy per-se, we do note some
GDPR-related benefits that accrue due to the
introduction of the model. These include accuracy
(Art 5.1(d)), integrity and confidentiality (Art 5.1.(f)),
accountability (Art 5.2) and tracking consent (Art 7
and Art 8).
7 CONCLUSIONS
We set out to determine to what extent can the
introduction of a data quality governance process for
both paper and electronic healthcare records improve
data quality in healthcare organisations undergoing
digital transformation. This led us to develop the
DQC/DQI model and easy-to-use checklist (Figure 6)
and tool, which can be applied to both the paper and
electronic records. We applied the DQC/DQI model
to the Irish Unified Healthcare Record and developed
a simple dashboard (Figure 7). The DQC/DQI model
forms the basis for validation rules or prompts for
embedding into an electronic healthcare record
(EHR) application.
Application of the DQI Model showed a
significant improvement in data quality scores during
implementation and testing against paper healthcare
records. We consistently achieved DQI scores in
excess of 80% when only focusing on the most
common quality errors in healthcare records. This
suggests the model could also provide improved data
quality within EHR’s, and form the basis for
integrated data quality governance in the roll-out of
EHRs in Ireland.
The DQI Model requires further testing in a
hospital and healthcare environment to demonstrate
the effectiveness of the approach in a wider variety of
applications and with a larger number of users.
It is hoped that the DQI model can effectively
support the transition of paper to electronic healthcare
record solutions in Ireland and in other jurisdictions.
REFERENCES
Bowman, S. (2013). Impact of electronic health record
systems on information integrity: Quality and safety
implications. Perspectives in Health Information
Management, 10, 1c.
Charnock, V. (2019). Electronic healthcare records and data
quality. Health Information & Libraries Journal, 36(1),
91–95. https://doi.org/10.1111/hir.12249
Fennelly, O., Cunningham, C., Grogan, L., Cronin, H.,
O’Shea, C., Roche, M., Lawlor, F., & O’Hare, N.
(2020). Successfully implementing a national
electronic health record: A rapid umbrella review.
International Journal of Medical Informatics, 144,
104281.
https://doi.org/10.1016/j.ijmedinf.2020.104281
Fenton, S., Low, S., Abrams, K., & Butler-Henderson, K.
(2017). Health Information Management: Changing
with Time. Yearbook of Medical Informatics, 26, 72–
77. https://doi.org/10.15265/IY-2017-021
Gordon, L., & Greene, J. (2014). Better data through IT
governance. Hospital & Health Network, 88, 38–39.
Greenhalgh, T., Stramer, K., Bratan, T., Byrne, E., Russell,
J., & Potts, H. W. W. (2010). Adoption and non-
adoption of a shared electronic summary record in
England: A mixed-method case study. BMJ, 340(jun16
4), c3111–c3111. https://doi.org/10.1136/bmj.c3111
Grogan, L. (2020). Paperless Healthcare. World of Irish
Nursing & Midwifery, 28(3), 44–45.
Guidance on Information Governance (p. 68). (2012).
Health Information and Quality Authority.
Gunter, T. D., & Terry, N. P. (2005). The Emergence of
National Electronic Health Record Architectures in the
United States and Australia: Models, Costs, and
Questions. Journal of Medical Internet Research, 7(1),
e3. https://doi.org/10.2196/jmir.7.1.e3
Health Service Executive. (2011). Standards and
Recommended Practices for Healthcare Records
Management. HSE Ireland.
Health Service Executive, & Dept of Health. (2013).
EHealth Strategy for Ireland (p. 80).
Hevner, March, Park, & Ram. (2004). Design Science in
Information Systems Research. MIS Quarterly, 28(1),
75. https://doi.org/10.2307/25148625
Houses of the Oireachtas. (2017). Slaintecare Report (p.
192). Committee on the Future of Healthcare.
https://www.oireachtas.ie/en/committees/32/future-of-
healthcare/
Hussey, P. A., & Kennedy, M. A. (2016). Instantiating
informatics in nursing practice for integrated patient
centred holistic models of care: A discussion paper.
Journal of Advanced Nursing, 72(5), 1030–1041.
https://doi.org/10.1111/jan.12927
Khatri, V., & Brown, C. V. (2010). Designing data
governance. Communications of the ACM, 53(1), 148–
152. https://doi.org/10.1145/1629175.1629210
Nagle, T., Sammon, D., & Cleary, W. (2019). A New
Approach to Business Value Driven Planning for Data
Projects [Preprint]. Open Science Framework.
https://doi.org/10.31219/osf.io/jg4pr
Parsons, A., McCullough, C., Wang, J., & Shih, S. (2012).
Validity of electronic health record-derived quality
measurement for performance monitoring. Journal of
the American Medical Informatics Association, 19(4),
604–609. https://doi.org/10.1136/amiajnl-2011-000557
Recommendation of OECD Council on Health Data
Governance. (2016).
Redman, T. C. (2016, July 28). Assess Whether You Have
a Data Quality Problem. Harvard Business Review.
The Data Quality Index: Improving Data Quality in Irish Healthcare Records
635

https://hbr.org/2016/07/assess-whether-you-have-a-
data-quality-problem
Stone, C. P. (2014). A Glimpse at EHR Implementation
Around the World: The Lessons the US Can Learn.
Health Institute for E-Health Policy, 12.
Urquhart, C., Currell, R., Grant, M., & Hardiker, N. (2018).
Nursing record systems: Effects on nursing practice &
healthcare outcomes. Cochrane Database of Systematic
Reviews.
https://doi.org/10.1002/14651858.CD002099.pub3
Wang, R. Y., & Strong, D. M. (1996). Beyond Accuracy:
What Data Quality Means to Data Consumers. Journal
of Management Information Systems. https://doi.org/
10.1080/07421222.1996.11518099.
ICEIS 2021 - 23rd International Conference on Enterprise Information Systems
636
