
Information of the Population of the Chelyabinsk Region about HIV
Infection and the Need for Services Related to the Prevention of HIV
Infection
A. М. Romodina
1a
, D. V. Valko
1b
, Е. А. Skachkova
1c
and А. V. Tananin
2d
1
The South Ural University of Technology, Chelyabinsk, Russia
2
The Charitable Foundation “Istochnik Nadezhdy”, Chelyabinsk, Russia
Keywords: HIV infection, public awareness, Chelyabinsk region, HIV prevention.
Abstract: The article analyzes the data of a sociological study conducted by the authors on the territory of the
Chelyabinsk region among citizens who took part in social projects of the Charitable Foundation “Istochnik
Nadezhdy”. Based on the results obtained, the authors assessed the level of awareness of the population about
HIV infection and the demand for services related to the prevention of HIV infection. Based on the results of
the work, it was concluded that most of the respondents are sufficiently informed about what HIV infection
is, about the ways of infection and what methods of prevention of this disease exist. Based on the results of
the study, the authors proposed to conduct more active preventive work among the population of the
Chelyabinsk region, as well as to ensure that the population is informed on behalf of medical workers about
the level of morbidity in the region, about the main periods of the development of the disease, about the
mechanisms of infection and how HIV infection can be transmitted, and where to get free help.
1 INTRODUCTION
AIDS, as one of the most important social problems,
arose before humanity at the end of the 20th century.
There are currently more than 40 million HIV-
infected officially registered in the world (Hongfei et
al, 2017).
The very first death from AIDS was recorded by
scientists in 1959 in Central Africa.
Later, the conclusion of doctors who studied the
medical history of a deceased person recognized that
this was the first (zero) recorded case of death from
AIDS in the world.
By 1985, the ways of HIV infection were finally
identified and officially confirmed - through blood,
sperm, breast milk. In the same year, the very first
HIV test was created.
Based on this development, the United States of
America and Japan began testing all donated blood
for HIV for the first time.
a
https://orcid.org/0000-0001-7876-2572
b
https://orcid.org/0000-0002-8058-7539
c
https://orcid.org/0000-0001-6795-9695
d
https://orcid.org/0000-0001-7371-490X
In Russia, the first major outbreak of the disease
occurred in the capital of Kalmykia - Elista. A worker
who served in the navy in 1982 became patient zero.
He passed the virus to his wife, and during pregnancy
their child was also infected. Immediately after the
birth of the baby, they were hospitalized in the
hospital, where the baby died before the diagnosis
was made. A total of 75 children and 4 adult women
were infected in Elista.
In the USSR at the end of the 80s cases of
infection of children with the immunodeficiency
virus during medical examinations were registered
(Elista, Krasnodar, Rostov on Don, Volgograd). The
total number of infected people was about 255.
Today Russia ranks 46th among countries in
terms of the spread of HIV infection. According to
most doctors, the Russian Federation is practically
one step away from the HIV epidemic (exceeding the
threshold of 2%). In Russia, only according to official
data, from 250 to 300 thousand people die from AIDS
every year (Fadeeva, 2020).
12
Romodina, A., Valko, D., Skachkova, E. and Tananin, A.
Information of the Population of the Chelyabinsk Region about HIV Infection and the Need for Services Related to the Prevention of HIV Infection.
DOI: 10.5220/0010680900003169
In Proceedings of the International Scientific-Practical Conference "Ensuring the Stability and Security of Socio-Economic Systems: Overcoming the Threats of the Crisis Space" (SES 2021),
pages 12-16
ISBN: 978-989-758-546-3
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

The study is devoted to studying the level of
awareness of the population about HIV infection and
the demand for services related to the prevention of
HIV infection.
The purpose of the study is to assess the level of
awareness and demand for services related to the
prevention of the spread of HIV infection among
people who took part in the projects of the Charitable
Foundation “Istochnik Nadezhdy”.
Research objectives:
Studying and determining the level of
knowledge of the population about the HIV / AIDS
disease itself, modes of transmission and methods of
treatment.
Analysis of people's awareness of methods of
prevention of the spread of disease.
Analysis of the awareness of the population
about the services that can be obtained as part of
preventive measures or in case of detection of a
disease.
Development of recommendations to improve
the level of awareness of the population about HIV
infection and about services and activities related to
the prevention of the spread of HIV infection.
The object of the research is the persons who
took part in the projects of the Charitable Foundation
“Istochnik Nadezhdy”.
The subject of the research is the level of
awareness of the population about HIV infection and
the public demand for services related to measures to
prevent the spread of HIV infection.
2 MATERIALS AND METHODS
The research was carried out by the Charitable
Foundation “Istochnik Nadezhdy” in cooperation
with the South Ural University of Technology.
According to the developed questionnaire, in the
period June-August 2020, 2100 people who use
psychoactive substances and use the services of the
Charitable Foundation “Istochnik Nadezhdy” for
HIV prevention were interviewed within the
framework of the project “Responding to the HIV
epidemic in the Urals District, among key groups”.
The sample included 2,100 people living in the
Chelyabinsk region. Sample type - multistage, serial
(gender, age, education level, professional
affiliation).
The representativeness of the sample allows us to
consider the opinion of the respondents as the opinion
of all people who participated in the project of the
Charitable Foundation “Istochnik Nadezhdy”
"Response to the HIV epidemic in the Urals District,
among key groups" with a statistical error of up to
2.1%.
Questionnaire points of respondents:
1. Outreach exits in Chelyabinsk, Kopeisk and
Magnitogorsk. Pedestrian outreach and interviews of
respondents using the visits of the Mobile Point.
2. Stationary Prevention Points in Chelyabinsk,
Magnitogorsk. These are the branch offices of the
Charitable Foundation “Istochnik Nadezhdy”.
The methodological basis of the research is
modern approaches in the field of organizing
sociological research, supported by analytical
methods and advanced developments in this area.
3 RESULTS AND DISCUSSION
Today, despite the fact that information is available
“in one click”, it is very difficult for an ordinary
member of society to obtain the most relevant,
complete and competent data regarding HIV
infection. There is a lot of talk about the human
immunodeficiency virus, but most people prefer to
bypass this topic, as it causes fear and rejection.
In this regard, we conducted a study aimed at
assessing the level of awareness of HIV infection
among people who use psychoactive substances and
use the services of the Charitable Foundation
“Istochnik Nadezhdy” for HIV prevention within the
framework of the project “Responding to the HIV
epidemic in the Urals District, among key groups”.
The most part of the respondents (43%) are
between 30 and 39 years old, 24% are between 20 and
29 years old, and those who are between 40 and 49
years old are only 20%.
Men make up the overwhelming majority of 69%
of the total number of respondents, and women - 31%.
The main part of those who participated in the
projects 61% (1045 people) have secondary or
specialized secondary education, 283 people have
higher education, which is 13%.
Most of the men surveyed (90%) are aware that
HIV infection is a serious disease, 91% of the women
surveyed agree with them. Only 3% of men and
women, respectively, think HIV is a scam and not a
cause for concern. Educational activity of the
Charitable Foundation “Istochnik Nadezhdy” gave
such a high result among the project participants.
If we consider the age of men and women, then
the overwhelming majority of the working age of
both sexes consider HIV-dangerous disease.
Information of the Population of the Chelyabinsk Region about HIV Infection and the Need for Services Related to the Prevention of HIV
Infection
13

Figure 1: What is the effect of HIV infection on the human
body? (in % of the total number of responses).
The most common answer to the question of how
HIV infection affects human health was “destroys the
immune system” - 80.1% of the respondents chose it.
9% of the respondents found it difficult to answer,
and 5.8% named the option “destroys the blood
coagulation system”. In principle, the respondents are
fully aware of the main factors of HIV infection that
affect the human body (see Fig. 1).
Figure 2. Ways of HIV transmission (in % of the total
number of men's responses).
When answering the questions about the known
ways of HIV transmission, the opinions of men and
women practically coincided (see Fig. 2, 3).
Figure 3: Ways of HIV transmission (in% of the total
number of responses of women).
Men and women more often indicated such
options as “Use of shared (non-disposable or non-
sterile) needles and syringes for injection” - 19.2%
and 18.8%, “unprotected sex” - 18.2% and 19.07%,
“Use of non-sterile equipment for piercing and
tattoos” by 13.2%, respectively.
This fact indicates that most of those who took
part in the study are aware of the main ways of HIV
transmission. This also suggests that participation in
the project has increased the level of awareness of
people.
Figure 4: Respondents' answers to the question: “What
biological fluids are the most dangerous ones for HIV
transmission?” (in % of the number of respondents).
The wrong option "saliva" was chosen by only
2.5% of the respondents. It can be concluded that
people who use psychoactive substances and use the
services of the Charitable Foundation “Istochnik
Nadezhdy” have a fairly high level of awareness
about how to get infected with HIV.
Figure 5: Groups of people with high risk of HIV infection
and transmission (in % of the total number of respondents).
The survey participants believe that clients of nail
and pedicure salons (offices) (4%) and patients of
dental institutions (5%) are least at risk.
Most likely, this is because people do not wonder
how manicure instruments are sterilized, whether the
master uses professional equipment such as a
sterilizer (disinfector). Or they believe that all masters
apply the necessary measures, including those who
work at home or in small salons. As for dental
institutions, they are medical institutions and must
strictly observe all measures to comply with the rules
of sterility in order to minimize all possible risks of
any infections of clients, including HIV.
In our research, we also asked the respondents:
"How can HIV infection be detected in a person?"
SES 2021 - INTERNATIONAL SCIENTIFIC-PRACTICAL CONFERENCE "ENSURING THE STABILITY AND SECURITY OF
SOCIO - ECONOMIC SYSTEMS: OVERCOMING THE THREATS OF THE CRISIS SPACE"
14
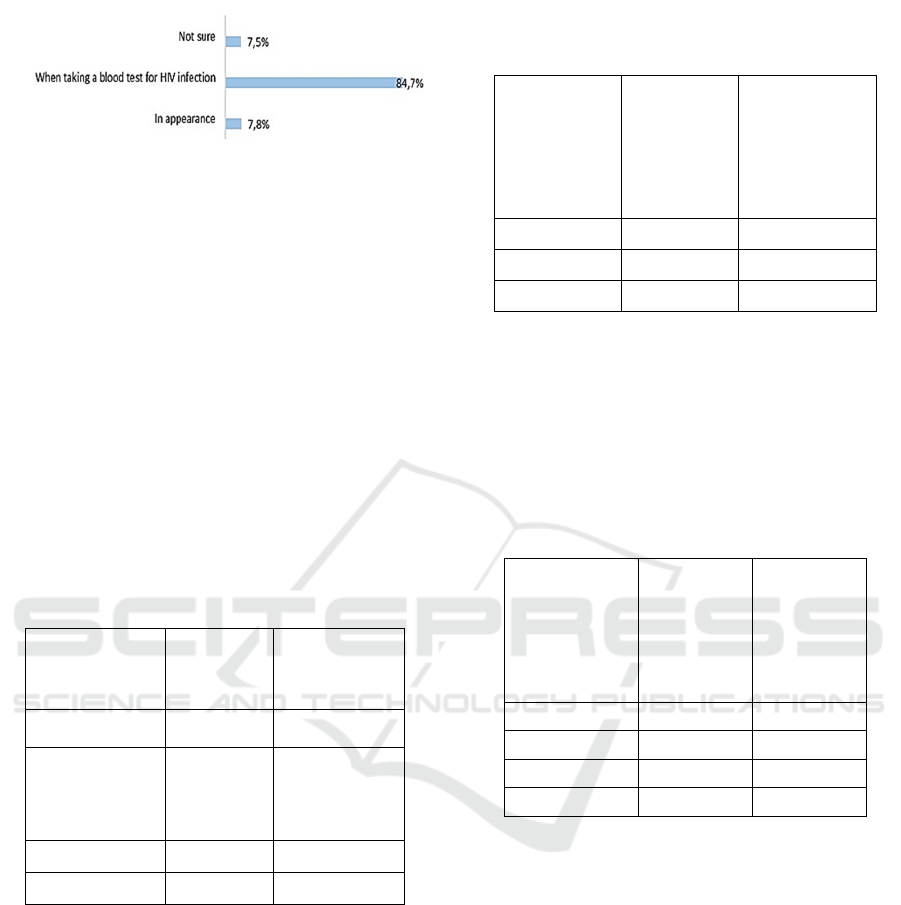
Figure 6: Methods for diagnosing HIV infection (in % of
the total number of respondents).
The overwhelming majority of the surveyed
project participants, 84.7%, know that in order to find
out their HIV status, it is necessary to take a blood
test. The special attention of the fund's projects is
aimed at informing people how to find out their HIV
status, where to turn for help and where they can get
free services for the treatment and prevention of
morbidity. And only 7.8% of respondents rely on
external signs. There is a prevailing stereotype that
HIV patients look emaciated or with signs of chronic
fatigue on their face, their hair falls out a lot, there are
abscesses and acne all over the body, and there is a
lack of body weight.
Table 1: Respondents' answers to the question: “Can an
HIV-infected woman give birth to a healthy child” (in % of
the total number of answers).
Can an HIV-
infected woman
give birth to a
healthy baby?
Number of
respondents,
people
Number, in%
No, under any
circumstances
203 10
Yes, if she takes
medications
regularly as
prescribed by her
docto
r
1426 68
Not sure 426 20
No answer 45 2
Thanks to participation in the project, most of the
respondents were able to answer this question
correctly. The majority of respondents, 68%, believe
that if a woman regularly takes medications, she can
give birth to an uninfected child. A pregnant woman
with a positive HIV status is monitored by a
gynecologist and an infectious disease specialist.
Doctors draw up an individual treatment regimen.
Medication prevents the development of the virus,
so that with full adherence to the treatment plan, a
woman with a positive HIV status can give birth to an
absolutely healthy baby.
Table 2: People's answers to the question: “Do you know
where, if necessary, you need to go to get tested for HIV?”
(in % of the total number of responses).
Do you
know where, if
necessary, you
need to go to
get tested for
HIV infection?
Number of
respondents,
people
Number, in%
Yes 1663
79
No 225
11
Not sure 192
10
Also, almost the majority of respondents know
where to go to get tested for HIV infection. Today,
almost all medical institutions (polyclinics,
laboratories, medical centers) can take a blood test for
HIV infection.
Table 3: Respondents' answers to the question: “If you
knew that your friend is HIV-positive, would you stop
communicating with him?” (in % of the total number of
responses).
If you found out
that your friend
is HIV positive,
would you stop
communicating
with him?
Number of
respondents,
people
Number, in%
Yes
304 14
No
1463 70
Not sure
313 15
No answer 20 1
HIV-infected people periodically face
discrimination, people, when they find out about their
diagnosis, stop communicating with them. Health
workers sometimes fail to comply with
confidentiality requirements and disclose HIV status
information. This problem is especially relevant in
small towns and villages, where people are afraid to
take the test, because the whole community can learn
about its results. Employers can force workers with
HIV diagnoses to leave.
The majority of those participating in our study,
70%, answered that they would not stop
communicating with a person if they found out about
his positive HIV status.
Only 14%, namely 304 people out of 2,100
respondents, said they would stop communicating.
Information of the Population of the Chelyabinsk Region about HIV Infection and the Need for Services Related to the Prevention of HIV
Infection
15

4 CONCLUSIONS
Based on the results of a survey of people who use
psychoactive substances and use the services of the
Charitable Foundation “Istochnik Nadezhdy” for
HIV prevention within the framework of the project
"Responding to the HIV epidemic in the Urals
District, among key groups" in July-August 2020, it
can be concluded that most of the respondents are
sufficiently informed about what HIV infection is,
about the ways of infection and about what methods
of prevention of this disease exist.
If we consider the age of men and women, then
the overwhelming majority of the working age of
both sexes consider HIV-dangerous disease.
Most of the respondents have an idea of how HIV
infection affects their health. Most often, the answer
to the question of how HIV infection affects human
health was the answer “destroys the immune system”
- 80.1% of the respondents chose it. 9% of the
respondents found it difficult to answer, and 5.8%
named the option “destroys the blood coagulation
system”. The population, in principle, does not fully
know all the factors of HIV infection that affect the
human body.
When answering the questions about the known
ways of HIV transmission, men and women were
more likely to mention “Use of shared (not disposable
or non-sterile) needles and syringes for injection” -
19.2% and 18.8%, “unprotected sex” - 18, 2% vs.
19.07%. “Use of non-sterile equipment for piercing
and tattoos” by 13.2%, respectively.
The majority of the respondents attributed people
who inject drugs and people who have casual sex to
risk groups, 22%, respectively. The third and fourth
places are taken by people with non-traditional sexual
orientation (16%) and persons providing commercial
sex services (15%).
72% of respondents know that there are drugs for
the treatment of HIV infection. Only 9% of the people
surveyed do not know about the existence of drugs for
this disease
Most of the respondents are aware that HIV
infection can be treated, and this disease cannot be
cured, but the body lends itself to long-term therapy
and, thanks to this, the risk of the infection becoming
AIDS is reduced.
Also, almost the majority of respondents know
where to go to get tested for HIV infection. Today,
almost all medical institutions (clinics, laboratories,
medical centers) can take a blood test.
62% of the respondents trust medical workers as
a source of information, 58% trust the AIDS Center
helpline employees, and 29% trust the media.
Based on the results of the study,
recommendations were made:
1. To carry out active preventive work among the
population of the Chelyabinsk region.
2. To ensure that the population is informed on
behalf of medical workers about the incidence rate in
the region, the main periods of the disease
development, the mechanisms of infection and how
HIV infection can be transmitted and where free
assistance can be obtained.
REFERENCES
Ajong, A. B., Njotang, P. N., Nghoniji, N. E., Essi, M. J.,
Yakum, M. N., Agbor, V. N. Kenfack, B.,
2018. Quantification and factors associated with HIV-
related stigma among persons living with HIV/AIDS on
antiretroviral therapy at the HIV-day care unit of the
Bamenda Regional Hospital, North West Region of
Cameroon. In Globalization and health. 14. 56.
Brinkley-Rubinstein, L., 2018. Jail and Prison Populations,
Epidemiology of HIV/AIDS. Encyclopedia of AIDS.
Fadeeva, E.V., 2020. Availability of free medical care in
Russia: status and issues. In Sociological Studies. 4. pp.
94-104.
Hongfei, D., Chi, P., Li, X., 2017. High HIV prevalence
predicts less HIV stigma: a cross-national investigation.
In AIDS Care. 30(6). pp. 714-721.
Louchet, M., Didelot, H., Mandelbrot, L., 2021. Frequency
of differential placental transfer to twins of maternal
antiretroviral medications. In European J. of Obstetrics
& Gynecology and Reproductive Biology. 256. pp. 405-
411.
Romodina, A. M., 2018. HIV / AIDS: Social aspects of the
problem. In Bulletin of the Council of young scientists
and specialists of the Chelyabinsk region. 2(21). pp. 67-
70.
Thapa, S., Hannes, K., Buve, A., Bhattarai, S., & Mathei,
C., 2018. Theorizing the complexity of HIV disclosure
in vulnerable populations: a grounded theory study. In
BMC Public Health. 18(1). pp. 162-167.
Thapa, S., Hannes, K., Cargo, M., Buve, A., Peters, S.,
Dauphin, S., & Mathei, C., 2018. Stigma reduction in
relation to HIV test uptake in low- and middle-income
countries: a realist review. In BMC Public Health. 18.
p. 1277.
SES 2021 - INTERNATIONAL SCIENTIFIC-PRACTICAL CONFERENCE "ENSURING THE STABILITY AND SECURITY OF
SOCIO - ECONOMIC SYSTEMS: OVERCOMING THE THREATS OF THE CRISIS SPACE"
16
