
Determinants of Neonatal Mortality in Indonesia
Nur Asiah
1
, Yulia Setianingsih
1
, Ahman Sya
2
, Izza Suraya
1
1
Faculty of Health Sciences, Universitas Muhammadiyah Prof. DR. HAMKA (UHAMKA), Jakarta, Indonesia
2
Program Study Population and environmental education, Universitas Negeri Jakarta, Jakarta, Indonesia
Keywords: Neonatal Mortality, Low Birth Weight, Antenatal Care, Parity.
Abstract: The results of the SDKI 2017 study show that the infant mortality rate aged 0-28 days was 15/1,000 live births,
meaning that out of 67 babies, 1 infant died in the first month of life. This shows that the Infant Mortality
Rate aged 0-28 days, although the number has decreased, the figure is still above the SDG's target of 12/1,000
live births. This study aims to determine the factors associated with infant mortality 0-28 days in Indonesia.
This type of research is quantitative with a cross-sectional study design. The data source in this study is the
SDKI 2017. The sample includes infants who meet the criteria for the last child and were born single. Data
were analysed by Bivariate analysis with chi-square test. The sampling Method in this study uses total
sampling. Bivariate results show variables related to infant mortality, namely mother's work status, Mother's
age at delivery, and parity with P <0.05. Based on the results of the study, it is suggested that there is a need
for increased vigilance and preparation for women of childbearing age starting from the preparation period
for pregnancy to delivery.
1 INTRODUCTION
The Infant Mortality Rate (IMR) is an important
indicator to determine health status in measuring the
level of progress of a country in terms of services and
development in the health sector. Based on data SDKI
from 2002-2003, 2007, and 2012, the Neonatal
Mortality Rate (NMR) is 20/1000 live births, 19/1,000
live births, and 19/1000 live births (SDKI, 2017).
These data show that the infant mortality rate did not
show a significant decrease. The data shows that the
neonatal mortality rate has decreased by 15/1,000 live
birth, but this figure has not been able to reach the
SDG's target of 12/1,000 live births.
One of the goals of the SDGs is to ensure a healthy
life and promote well-being for all people of all ages
as stated in point 3 of the SDGs. In these goals, there
are 13 targets, one of which is ending preventable
infant and under-five mortality, by trying to reduce the
Neonatal Mortality Rate (NMR) to at least 12/1,000
live births and the under-five mortality rate of
25/1,000 live births by 2030 (Ministry of Health,
2015).
Globally, neonatal mortality accounts for 47% of
all under-five deaths. Several previous studies on
neonatal and perinatal mortality show that the factors
associated with neonatal mortality were low birth
weight (Abdullah, Naiem, & Mahmud, 2012),
pregnancy complications (Suraya, 2017), birth
spacing (Simbolon, 2012), maternal age (Titaley,
Christiana R; Dibley, Michael J; Roberts, Kingsley
Christine L; Hall, John, 2008), maternal education
(Mahcepat, et al, 2011), birth attendant (Noorhalimah,
2015), antenatal visits (Tyas & Notobroto, 2014),
antenatal care (Yani, 2013), parity (Sugiharto, et al,
2010), place of delivery (Suraya, et al, 2017).
Some of the obstacles in efforts to reduce the
Infant Mortality Rate (IMR) are the poor quality of
antenatal, delivery, and postnatal health services
(UNICEF, 2012). Based on the description of the
problems above, the researchers conducted a study on
Determinants of Neonatal Death in Indonesia.
2 METHODS
This type of research is quantitative analysis using a
cross-sectional design. The data used is the SDKI
2017 data, which was conducted from 24 July to 30
September 2017 and throughout Indonesia covering
34 provinces. The population in this study were all
live births of the last child of women aged 15-49 years
who were ever married, in the period 2013-2017 in
Indonesia based on SDKI 2017 sample. Selection of
210
Asiah, N., Setianingsih, Y., Sya, A. and Suraya, I.
Determinants of Neonatal Mortality in Indonesia.
DOI: 10.5220/0010760200003235
In Proceedings of the 3rd International Conference on Social Determinants of Health (ICSDH 2021), pages 210-213
ISBN: 978-989-758-542-5
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
samples from cleaning data Women aged 15-49 years
with ever-married status who successfully
interviewed and gave birth to their last child (live
birth) in the period 2013 – 2017 as many as 10,238
samples. The sampling method in this study is total
sampling, where all members of the population are
sampled.
Bivariate analysis was carried out using the chi-
square statistical test to test the research hypothesis,
namely the relationship between the independent
variable and the research dependent variable, namely
infant mortality.
3 RESULTS
The univariate analysis in this study included
descriptive analysis of data on neonatal mortality,
maternal education level, maternal employment
status, maternal age at delivery, and parity.
3.1 Univariate Analysis
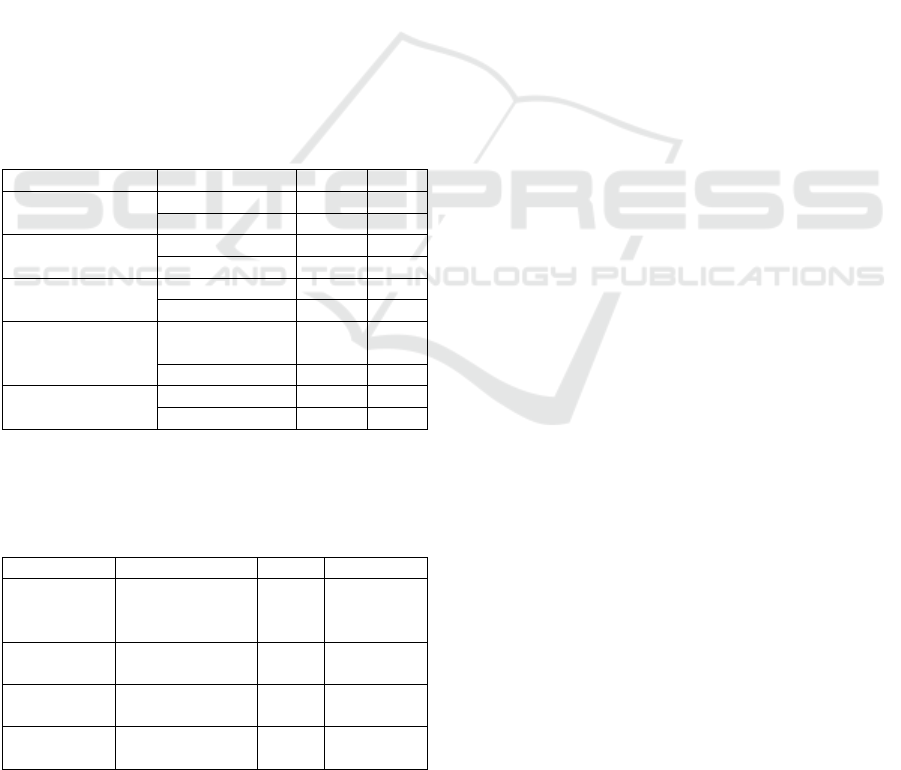
Table 1: Recapitulation of univariate test of neonatal
mortality in Indonesia 2013-2017.
Variable Cate
g
oric n %
Neonatal Death Yes 108 1.1
No 10,130 98.9
Mothers Education
Level
Low 3,190 31.2
High 7,048 68.8
Mother’s Work
Status
Worke
d
5,023 49.1
Didn’t Wor
k
5,215 50.9
Mother’s Age at
Delivery
At-Risk (<20 or
>35 years)
2,616 25.6
No-Risk
(
20-35
)
7,622 74.4
Parity At-Risk
(
>3
)
2,519 24.6
No-Risk
(
1-3
)
7,719 75.4
3.2 Bivariate Analysis
Table 2. Recapitulation of Bivariate analysis of neonatal
mortality in Indonesia 2013-2017.
Variable PR
(
95% CI
)
Pvalue Results
Mothers
education
level
1.300
(0.881-1.916)
0.185 No
Significant
Relationshi
p
Mother's
wor
k
status
1.631
(1.110-2.397)
0.012 Significant
Relationship
Mother's Age
at deliver
y
1.927
(1.315-2.826)
0.001 Significant
Relationship
Parity 1.875
(
1.275-2.759
)
0.001 Significant
Relationshi
p
3.2.1 Education
Respondents with a low level of maternal education
experienced more neonatal deaths, namely 1.3% than
respondents with a high level of maternal
education, namely 1.0%. The results of the Chi-
Square test showed that there was no relationship
between maternal education level and neonatal
mortality (P-value = 0.185). The results of the
calculation of the Prevalence Ratio (PR) show a value
of 1.3 (95% CI: 0.881-1.916), meaning that
respondents with a low level of maternal education
have a 1.3 times chance of experiencing neonatal
death than respondents with a high level of maternal
education.
3.2.2 Mother’s Work Status
Respondents with working mothers experienced
more neonatal deaths, namely 1.3% than mothers who
did not work, namely 0.8%. The results of the Chi-
Square test show that there was a relationship
between
maternal work status and neonatal mortality
(P-value =
0.012). The results of the Prevalence Ratio (PR)
calculation show a value of 1.631 (95% CI: 1.110-
2.397), meaning that respondents with working
mothers have a 1.613 times chance of experiencing
neonatal death than respondents with mothers who do
not work.
3.2.3 Mother's Age at Delivery
Maternal age at risk of giving birth (<20 or >35
years) experienced more neonatal deaths, namely
1.6% compared to the age of mother at risk of giving
birth (20-35 years) which was 0.9%. The results of
the Chi-Square test showed that there was a
relationship between maternal age at delivery and
neonatal mortality (P-value = 0.001). The results of
the calculation of the Prevalence Ratio (PR) showed
a value of 1.927 (95% CI: 1.315-2.826) maternal age
at risk (<20 or >35 years) 1.9 times experienced
neonatal death than respondents with maternal age at
delivery, not at risk (20 -35 years old).
3.2.4 Parity
Respondents with parity at risk (1 or 4 times)
experienced more neonatal deaths, namely 1.6% than
respondents with parity at no risk (2 – 3 times) which
was 0.9%. The results of the Chi-Square test showed
that there was a relationship between maternal age at
delivery and neonatal mortality (P- value = 0.001).
The results of the Prevalence Ratio (PR) calculation
show a value of 1.875 (95% CI: 1.275-2.759),
Determinants of Neonatal Mortality in Indonesia
211

meaning that respondents with parity at risk (1 or 4
times) have a 1.875 times chance of experiencing
neonatal death than respondents with parity at risk (2
– 3 times).
4 DISCUSSION
Mosley and Chen's theory explains that mortality and
child survival is influenced by sociodemographic
factors but are not able to directly affect child survival,
but require direct intermediaries called proxy
variables. The proxy variables consist of maternal
factors, environmental factors, malnutrition,
accidents, and personal illness control.
4.1 Education of Mothers with
Neonatal Mortality
Based on the results of the study, there were more
mothers with higher education (68.8%) than mothers
with lower education (31.2%).
Bivariate analysis using the Chi-Square test
obtained
a P-value of 0.185, which means that there is
no significant relationship between maternal
education level and neonatal mortality. With a
Prevalence Ratio (PR) value of 1.300 (95% CI: 0.881
– 1.916) this means that mothers with low education
are 1.3 times more likely to experience neonatal
death than mothers with higher education.
These results are in line with research conducted
by Sari and Syarif, (2016), Simbolon (2012), and
research conducted by Raharni (2011) which also
states that there is no significant difference between
reducing infant mortality.
Education is an effort to improve abilities and
develop a personality for life so that they can make
household decisions so that they can face various
problems including health problems to reduce the
risk of infant and toddler mortality. The level of
maternal education is closely related to the level of
understanding of health care, hygiene, the need for
prenatal care. (Septiana Dwi Susanti Aisyan et al,
2010).
4.2 Mothers Work Status with
Neonatal Mortality
The results of the univariate test show that there were
more working mothers (50.9%) than mothers who did
not work (49.1%).
The results of bivariate analysis using the Chi-
Square test obtained a P-value of 0.012, meaning that
there is a significant relationship between maternal
employment status and neonatal mortality. With a
Prevalence Ratio (PR) value of 1.631 (95% CI 1.110-
2.397), this means that working mothers are 1.6 times
more likely to experience neonatal death compared to
mothers who do not work.
This result is in line with the results of a study
conducted by Suparmi et al (2016) which shows that
children of working mothers had an 81% higher risk
of neonatal death when compared to neonatal death at
non-working mothers.
Working mothers tend to have less rest, less time
to take care of themselves, imbalance in eating, work
stress, tension due to fatigue. The severity of the
mother's work will affect the condition of the body
and ultimately affect the health status of the mother
which affects infant mortality. (Khomsan, 2010).
4.3 Mother's Age at Delivery with
Neonatal Death
The results of the bivariate analysis using the Chi-
Square test obtained a P-value of 0.001 which means
that there is a relationship between maternal age at
delivery and neonatal mortality. The results of the
Prevalence Ratio calculation obtained a value of 1.927
(95% CI 1.315 – 2.826) indicating that mothers who
gave birth at an age at risk had a 1.9 times chance of
experiencing neonatal death than mothers who gave
birth at an age, not at risk.
This is reinforced by research conducted by
Masitoh, et al (2014), Suparmi, etc (2016), and Sari &
Syarif (2016) showing that there is a significant
relationship between maternal age and neonatal
mortality.
Maternal age at delivery is one of the risk factors
for neonatal death. At the age that is considered safe,
namely 20-35 years, the mother is more physically and
psychologically prepared so that the risk of pregnancy
and childbirth disorders is relatively very low. At the
age of the motherless than 20 years, the risk of infant
mortality is higher because the mother has not finished
experiencing growth and development. The pelvis and
uterus are immature so there is a risk of jamming in
the birth canal resulting in prolonged labor and other
disorders. The risk of recurrence increases when the
mother's age is above
35 years, due to a decrease in
maternal health and the
process of changing
reproductive organs (Simbolon, 2012).
Education is an effort to improve abilities and
develop a personality for life so that they can make
household decisions so that they can face various
problems including health problems to reduce the risk
of infant and toddler mortality. The level of maternal
ICSDH 2021 - International Conference on Social Determinants of Health
212

education is closely related to the level of
understanding of health care, hygiene, the need for
prenatal care. (Septiana Dwi Susanti Aisyan et al,
2010).
4.4 Parity with Neonatal Mortality
Univariate results show that mothers with parity were
not at risk (75.4%) more than mothers with parity at
risk (24.6%).
The results of the bivariate analysis show a
significant relationship between parity and neonatal
mortality. Mothers with parity at risk are 1.875 times
more likely to experience neonatal death than
mothers with parity at risk. This is also reinforced by
previous research conducted by Masitoh, et al (2014),
Maheasy, et al (2011), Kurniawan and Melaniani
(2018) showing a relationship between parity and
infant mortality (P-value 0.000). Mothers who have
given birth to more than two children are 0.09 times
more likely to experience infant death in subsequent
births than mothers who have given birth to a second
child or less than two children. A positive relationship
with death status makes the higher the parity value or
the more children born, the higher the risk of the
mother giving birth to a dead baby. Parity is a variable
that has a relationship with infant mortality.
Health problems in pregnant women and childbirth
appear in mothers with parity at risk, namely giving
birth to more than 2 children. It is can make the uterine
broken and lead to abnormalities in the mother's
womb. This has an impact on the condition of the
location of the fetus or placenta in the mother which
can interfere with fetal growth. Disruption of fetal
growth in the mother's womb makes the mother give
birth to an unhealthy baby (Wiknjosastro, 2007).
5 CONCLUSION
Mothers with low education are more likely to
experience neonatal deaths than mothers with higher
education. Mothers who work experience more
neonatal deaths than mothers who do not work.
Mothers who gave birth at the age of <20 and >35
experienced more neonatal deaths than mothers who
gave birth at the age of 20-35. Mothers with parity at
risk had more chances of experiencing neonatal
deaths than mothers with non-risk parity. To reduce
the neonatal mortality rate, it is necessary to conduct
education or health promotion by related parties to
prospective mothers, especially teenagers, so that
they get married at the right age and plan their
pregnancy at an age that is not at risk. Women of
childbearing age are also advised to plan the number
of children they have. For working mothers who are
pregnant, pay attention to the type and workload they
do.
REFERENCES
Abdullah, A. Z., Naiem, M. F., & Mahmud, N. U. (2012).
Faktor Resiko Kematian Neonatal Dini di Rumah Sakit
Bersalin. Jurnal Kesehatan Masyarakat Nasional, Vol.
6 No. 6, 283 - 288.
Kemenkes R.I. (2015). Kesehatan Dalam Kerangka
Sustainable Development Goals (SDGs). Jakarta:
Kementerian Kesehatan RI.
Masitoh, S., EVK, T., & Karningsih. (2014). Asfiksia
Faktor Dominan Penyebab Kematian Neonatal. Jurnal
Ilmu dan Teknologi Kesehatan, Vol. 1 No. 2, 163 - 168.
Mekonnen, Y. (2013). Neonatal Mortality in Ethiopia:
Trends and Determinants. BMC Public Health.
Noorhalimah. (2015). Faktor-Faktor yang Berhubungan
dengan Kematian Neonatal di Kabupaten Tapin. Jurnal
Publikasi Kesehatan Masyarakat Idonesia, Vol. 2 No.
2, 64 - 71.
Raharni, Isakh, B. M., & Diana, I. (2011). Profil Kematian
Neonatal Berdasarkan Sosio Demografi dan Kondisi
Ibu saat Hamil di Indonesia. Buletin Penelitian Sistem
Kesehatan, Vol 14 no 4, 391 - 398.
Sari, T. W., & Syarif, S. (2016). Hubungan Prematuritas
dengan kematian Neonatal di Indonesia Tahun 2010
(Analisis Data Riskesdas 2010). Jurnal Epidemiologi
Kesehatan Indonesia, Vol 1 no 1, 9 - 14.
SDKI. (2017). Survei Demografi dan Kesehatan Indonesia
2017. Indonesia: Badan Kependudukan dan Keluarga
Berencana Indonesia.
Sugiharto, M., & Kusumawati, L. (2010, Oktober 4).
Analisis Perbedaan antar Paritas Ibu. Buletin Penelitian
Sistem Kesehatan, pp. 321-325.
Suraya, Izza. (2017). Determinan Kematian Neonatal Pada
Bayi Lahir Rendah di Indonesia (Analisis Data SDKI
2002-2003 dan 2007). ARKESMAS, Vol. 2 No.1, 126-
134.
Titaley, Christiana R; Dibley, Michael J; Roberts, Kingsley
Christine L; Hall, John. (2008). Determinants of
Neonatal Mortality in Indonesia. BMC Public Health,
8:232, 1-15.
Tyas, S. C., & Notobroto, H. B. (2014). Analisis Hubungan
Kunjungan Neonatal, Asfiksia dan BBLR dengan
Kematian Neonatal. Jurnal Biometrika dan
Kependudukan, Vol. 3, 168-174.
UNICEF. (2012). Ringkasan Kajian Kesehatan Ibu &
Anak. Indonesia: UNICEF Indonesia.
World Health Organization. (2006). Neonatal and
Perinatal Mortality. Prancis: WHO.
Wiknjosastro,H. 2007. Ilmu Kebidanan. Jakarta: Yayasan
Bina Pustaka
Yani, D. F., & Duarsa, A. B. (2013). Pelayanan Kesehatan
Ibu dan Kematian Neonatal. Jurnal Kesehatan
MAsyarakat Nasional.
Determinants of Neonatal Mortality in Indonesia
213
