
Outpatient Diversion using Real-time Length-of-Stay Predictions
Najiya Fatma
a
and Varun Ramamohan
b
Department of Mechanical Engineering, Indian Institute of Technology Delhi, Delhi, India
Keywords:
Length-of-stay, Patient Diversion, Delay Prediction, Primary Health Centers.
Abstract:
In this work, we show how real-time length-of-stay (LOS) predictions can be used to divert outpatients from
their assigned facility to other facilities with lesser congestion. We illustrate the implementation of this diver-
sion mechanism for two primary health centers (PHCs), wherein we divert patients from their assigned PHC to
the other PHC based on their predicted LOSs in both facilities. We develop a discrete-event simulation model
of patient flow operations at these two PHCs in an Indian district and observe significantly longer LOSs at one
of the PHCs due to disparities in the patient loads across both PHCs. We first determine the expected LOS of
the patient at the point in time at which they are expected to arrive at a PHC using system state information
recorded at the current time at the PHC in question. The real-time LOS predictions are generated by estimat-
ing patient wait times on a real-time basis at the queueing subsystems within the PHC. We then divert the
patient to the appropriate PHC on the basis of the predicted LOS estimates at both PHCs, and show through
simulation that the proposed framework leads to more equitable utilization of resources involved in provision
of outpatient care.
1 INTRODUCTION
Patient length-of-stay (LOS) is an important indi-
cator of the efficiency of hospital management sys-
tems (Ayyoubzadeh et al., 2020). Long LOSs and
overcrowding are important operational issues fac-
ing healthcare facilities around the world (Wachtel
and Elalouf, 2020), including in India (Sharma et al.,
2021). This in turn leads to both operational and clini-
cal issues, such as denial of hospital admissions, can-
cellation of surgeries, and higher likelihoods of de-
veloping healthcare acquired infections (Zhou et al.,
2019; Arefian et al., 2019).
Congestion and longer LOSs at specific facilities
within a healthcare facility network, which in turn
lead to inequitable utilization of facilities across the
network, may occur due to patient perceptions of
better quality of care at certain facilities within the
network (Liu et al., 2018). Healthcare administrators
may adopt different strategies to relieve congestion
such as capacity replanning (Whiteside et al., 2020),
patient diversion (Marquinez et al., 2021), and early
discharges for medically stable patients. However,
increasing resource capacity is often difficult due
to the capital investment required and the attendant
a
https://orcid.org/0000-0001-7790-3679
b
https://orcid.org/0000-0001-6517-9142
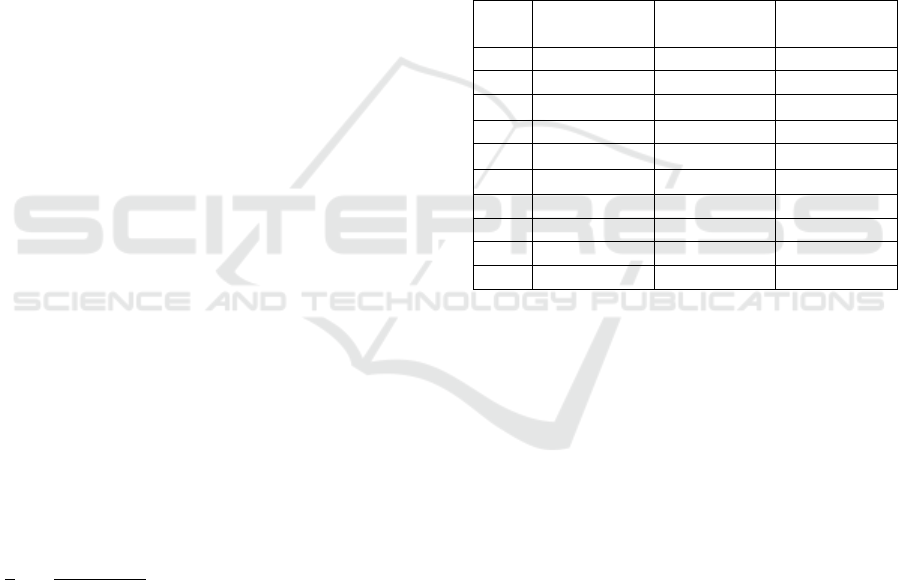
Table 1: Key acronyms and notation.
Acronyms /
Notation
Corresponding constituent words
LOS Length-of-stay
PHC Primary health center
DES Discrete event simulation
δ
x
Travel time to reach PHC x
ρ Resource utilization
∆
ρ
Change in resource utilization
w Wait time in a queue
∆
w
Change in queue wait time
G(.) Queueing system service time cd f
medical training required when personnel numbers
are increased. Hence, patient diversion is often the
preferred alternative to mitigate overcrowding. In
this study, we describe an approach towards using
real-time LOS predictions to facilitate diversion
of outpatients across primary healthcare facilities.
While we demonstrate our approach via the diversion
of outpatients across two primary healthcare centers
(PHCs) in the Indian context, our approach can be
used in any setting where patient diversion is being
considered due to high LOSs, or more generally,
where significant disparities in resource utilization in
a healthcare network is observed.
56
Fatma, N. and Ramamohan, V.
Outpatient Diversion using Real-time Length-of-Stay Predictions.
DOI: 10.5220/0010837400003117
In Proceedings of the 11th International Conference on Operations Research and Enterprise Systems (ICORES 2022), pages 56-66
ISBN: 978-989-758-548-7; ISSN: 2184-4372
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

In India, PHCs are the first point of contact for
the patients with a formally trained doctor and pro-
vide outpatient care, and limited emergency and in-
patient care (Shoaib and Ramamohan, 2021). The
Indian government has recently undertaken an initia-
tive to expand and upgrade existing PHCs (Blanchard
et al., 2021), and hence it is reasonable to assume
an increase in the patient load at these PHCs given
the established link between increased quality of care,
improved infrastructure and higher demand (Rao and
Sheffel, 2018). Based on previous work regarding
modeling PHC operations (Fatma et al., 2020; Shoaib
and Ramamohan, 2021), we developed a discrete-
event simulation (DES) of medical care operations
of two PHCs in an Indian district. Under conditions
of high outpatient demand, the DES outcomes indi-
cated signifcant disparity in outpatient LOSs across
both facilities, and this would likely extend to the en-
tire public health network in the district. Further, we
also noted that under these high demand conditions,
patient wait times to receive service from the doctor
did not increase significantly due to the very high ser-
vice rates of the doctor. Instead, the impact of high
demand was reflected in wait times at supporting sub-
systems in the PHC such as the pharmacy and the
laboratory, which in turn yielded high LOSs in the
PHCs as a whole. For example, average LOSs were
approximately 60 minutes, in comparison to average
total service times of less than 10 minutes across all
services that a patient may avail of in a typical PHC
visit. Thus, implementing diversion on the basis of
wait times in this context did not appear appropriate;
hence, we considered diversion based on patient LOS
as a whole in the facility.
The diversion mechanism that we propose utilizes
real-time LOS predictions to inform the diversion de-
cision. Diversion mechanisms based on real-time wait
time or ‘delay’ predictions for emergency patients
have been discussed in previous work (Fatma and Ra-
mamohan, 2021a); however, in this work, we use real-
time delay estimates to calculate real-time LOS pre-
dictions that in turn determine the diversion decision.
The real-time delay estimates, and in turn the real-
time LOS predictions, are generated at the point when
the patient decides to visit the facility in question (as
opposed to when the patient arrives at the facility),
implying that an information technology (IT) system,
including a web/smartphone application, to convey
this information to this patient would be required. Ex-
amples of such IT systems can be found in the United
Kingdom’s National Health Service (Mustafee and
Powell, 2020). In this paper, we develop a mech-
anism for patient diversion based on such real-time
LOS predictions (including a discussion of how such
LOS predictions can be generated) and demonstrate
via DES its impact on the operational outcomes of a
healthcare facility network. Our study provides the
operational basis that an IT system such as that de-
scribed in Mustafee and Powell (2020) can leverage
to implement real-time LOS-based diversion.
We now discuss the literature relevant to this
study, and describe our research contributions with re-
spect to the literature.
2 LITERATURE REVIEW
In this section, we focus on the literature associated
with real-time LOS prediction and patient diversion.
As part of the literature review, we also discuss stud-
ies that highlight the importance of information shar-
ing across facilities in the network wherein diversion
is implemented. We describe the research contribu-
tions of this work at the end of each subsection.
2.1 Length-of-Stay Prediction
The importance of LOS prediction at healthcare fa-
cilities and their subunits such as the emergency de-
partment is reflected in the considerable body of lit-
erature devoted to this topic (Song et al., 2015; Als-
inglawi et al., 2020; Shi et al., 2021; El-Bouri et al.,
2021). From the perspective of the methods used for
LOS prediction, it appears that data mining and sta-
tistical learning methods have been most widely used
(Verburg et al., 2014; Barnes et al., 2016; Turgeman
et al., 2017; Guti
´
errez et al., 2021; Shaaban et al.,
2021). A review conducted by El-Bouri et al. (2021)
found that multiple machine learning techniques such
as deep neural networks, random forest trees, regres-
sion techniques and decision trees among others have
been used to predict the patients LOS. The authors
then conclude that the LOS predictions were found
to be useful in planning patient admission schedules
and, as required, the preparation of post-discharge
care.
LOS prediction studies in the literature have pri-
marily focused on inpatients and emergency patients
using statistical learning techniques. The typical
methodology for LOS prediction for these patient
types involved the following steps: (a) recording clin-
ical information of patients such as medication history
at the time of admission, patient age, and the number
of comorbidities, (b) identifying the set of predictor
variables among the data available for LOS predic-
tion, (c) training and validating the statistical learn-
ing methods on the dataset constructed via mining the
available data (Baek et al., 2018; Aghajani and Kar-
Outpatient Diversion using Real-time Length-of-Stay Predictions
57

gari, 2016; Hijry and Olawoyin, 2020). The majority
of authors concluded that factors such as severity of
the disease, recency of diagnosis and type of surgery,
patient age, number of comorbidities, surgery type,
number of days of hospitalisation before surgery, etc.,
were significantly correlated with patient LOS. These
studies did not determine the effect of operational
variables such as the number of patients in the queue
for system resources, the elapsed service time of pa-
tients currently receiving care, etc., on patient LOS.
In this context, we generate LOS predictions via a
methodology grounded in queueing theory and real-
time delay prediction that estimates patient LOSs in
the PHC as a function of operational ‘system state’
variables such as the number of patients in the queue
at each queueing system within the PHC (e.g., the
queueing system represented by the doctor and the
laboratory), the elapsed service times of patients cur-
rently receiving service at each queueing subsystem,
arrival and service rates of patients in the PHC, and
the average travel time of patients to the PHC from
their point of origin. If the patient decides to leave for
the PHC at time t, then the LOS prediction is gener-
ated for the time of arrival of the patient in the system
- i.e., at time t + δ, where δ is the travel time to the
PHC from the patient’s location.
We note here that because we use real-time de-
lay predictions to generate the LOS predictions, our
approach can be extended to multi-class multi-server
systems for which real-time delay predictors have
previously been developed, including certain sys-
tems with non-stationary arrival and service processes
(Ibrahim, 2018). Further, in general, our approach is
likely to require fewer variables to be recorded for
generating the real-time delay estimates in compari-
son to statistical learning predictors, and its develop-
ment and deployment will not require construction of
a training and validation dataset. We also note that the
majority of previous work focuses on generating LOS
predictions for patients at a single unit of a health-
care facility, such as the emergency department, and
do not generate predictions for patients that receive
service from multiple units within a given facility. In
comparison, our approach generates LOS predictions
at multiple units within the same facility; that is, total
predicted LOS is the summation of time spent at each
PHC subsystem.
2.2 Patient Diversion
There are multiple studies considering patient diver-
sion as a means to reduce congestion at healthcare
facilities. In a review by Li et al. (2019), the au-
thors find that patient diversion was initiated based
on multiple measures of congestion, such as the av-
erage wait time of patients before receiving care, the
number of patients waiting to receive care, the num-
ber of occupied beds in a ward, etc. From a method-
ological standpoint, the approaches used to optimize
various aspects of the diversion process include a
Markov decision process formulation to maximize the
cost-effectiveness of diversion policies for ICU pa-
tients in a public-private hospital network (Marquinez
et al., 2021), a simulation optimization approach to
minimize the time to receive care (including wait
times and travel times between facilities) (Ramirez-
Nafarrate et al., 2011), and a mixed integer program-
ming approach to minimize the number of patients
waiting for care across the network (Nezamoddini and
Khasawneh, 2016). Fatma and Ramamohan (2021a)
evaluated via DES the effectiveness of patient diver-
sion strategies on multiple operational outcomes such
as resource utilizations, wait times, and the propor-
tion of patients whose wait time before receiving care
exceeds a threshold duration. The proportion of pa-
tients leaving without receiving care has also been an
operational outcomes of interest in multiple studies
(Morley et al., 2018).
An important consideration in implementing a di-
version mechanism within a healthcare facility net-
work is information sharing across the network re-
garding operational variables at each facility that are
used to determine diversion decisions. In this re-
gard, there is considerable support in the literature re-
garding implementing centralized diversion policies
across healthcare facilities, because diverting patients
without considering the operational information at
other facilities can yield worse operational outcomes
for both patients and the healthcare facilities across
the network, such as increased wait times for the di-
verted patient, and increased crowding at healthcare
facilities in the network (Deo and Gurvich, 2011; Li
et al., 2019; Shi et al., 2021). This has been fur-
ther emphasized in the recently published literature,
wherein Shi et al. (2021) find that communication and
coordination among healthcare facilities are crucial to
relieve congestion across all facilities in a healthcare
network, and diversion decisions must be made us-
ing infomation available from electronic management
systems networked across all facilities under consid-
eration (Adjerid et al., 2018; Dong et al., 2019; Pier-
marini and Roma, 2021). In this context, our study
also proposes a diversion mechanism for outpatients
that implicitly assumes the presence of a centralized
IT system that maintains information regarding the
operational status - in terms of system state variables
such as the number of patients waiting and elapsed
service times in various queues within the facility -
ICORES 2022 - 11th International Conference on Operations Research and Enterprise Systems
58

that is available to all facilities within the network.
We note here that most studies we surveyed, as is
natural, considered diversion of emergency patients.
Only Nezamoddini and Khasawneh (2016) briefly
discuss the effect of diverting non-emergency patients
to other healthcare facilities in a multi-hospital set-
ting. To the best of our knowledge, we did not identify
other studies that considered diversion of outpatients,
and in particular, we did not identify other studies that
utilized real-time LOS estimates for this purpose.
As discussed above, our approach - in relation
with the extant literature - also considers a central-
ized diversion mechanism involving information shar-
ing. In this regard, our work is similar to the work
by Fatma and Ramamohan (2021a); however, where
they use real-time delay estimates to divert emer-
gency (childbirth) patients arriving at facilities within
a healthcare network seeking care, we utilize real-
time delay estimates in generating LOS predictions
- at the point in time when they may access the IT
system associated with the healthcare network - to as-
sign patients to a facility within the network. While
this may seem like a facility assignment exercise in-
stead of patient diversion, we consider this a diversion
issue because patients are typically already assigned
as belonging to the catchment area of their nearest
PHC, and hence our framework determines whether
they must be ‘diverted’ to visit a facility located far-
ther from them on the basis of real-time LOS predic-
tions. However, where such facility assignment is not
a priori performed, our approach can be used for real-
time facility assignment as well.
3 PRIMARY HEALTH CENTERS
In India, PHCs serve as the first point of contact be-
tween the population and the healthcare provider with
the objective of making healthcare services accessible
in both the rural and urban areas. PHCs are estab-
lished to cover a population of 30,000 in rural areas
and 20,000 in hilly, tribal, and desert areas, providing
a range of essential outpatient care, and limited inpa-
tients and childbirth care (IPHS-Guidelines, 2012).
PHCs provide six hours of outpatient care ser-
vices and 24×7 emergency services including in-
patient and childbirth care to the patients. PHCs
have one to two doctors, a non-communicable disease
(NCD) nurse for conducting lifestyle disease checks,
one staff nurse per shift, a pharmacist, and a labo-
ratory technician. Routine blood and urine investi-
gations, and sputum tests for suspected tuberculosis
cases are offered by the in-house laboratory within the
PHCs. PHCs also have one labor bed for normal and
assisted deliveries for childbirth patients and four to
six indoor beds for admitting emergency patients to
ensure easy access to public health facilities. We re-
fer readers to Shoaib and Ramamohan (2021) for a
detailed understanding of medical care operations at
PHCs.
We now briefly describe the patient flow within
PHCs. Outpatients aged greater than 30 years first
consult the NCD nurse before consulting the doctor.
The NCD nurse checks blood pressure and blood glu-
cose levels, body temperature, and also provides diet-
related consultation to patients, as required. Other
outpatients directly consult the doctor or wait in the
outpatient queue if the doctor is busy with other pa-
tients. Once the outpatients complete their consulta-
tion with the doctor, approximately half the patients
are sent to the in-house laboratory for routine inves-
tigations. All patients exit from PHC via the phar-
macy regardless of whether they require medication,
because the pharmacy also performs the administra-
tive task of registering patient visits before their exit
from the PHC. Outpatient flow through the PHC is
depicted in Figure 1.
During outpatient department (OPD) hours, inpa-
tients and childbirth patients are attended to by the
doctor first and if the doctor is unavailable, they are
attended to by the staff nurse. Once their consultation
with the doctor is complete, inpatients are admitted to
the inpatient department (IPD) where the staff nurse
monitors their condition and treats accordingly. In-
patient LOSs in the IPD range from four to six hours,
because patients are typically admitted for minor con-
ditions that require monitoring and treatment for brief
periods. Childbirth patients are taken to the labour
room for delivery under the supervision of the doctor
and the staff nurse. After delivery, childbirth patients
are shifted to the IPD ward. Note that for more com-
plex inpatient and childbirth cases requiring more in-
tensive and specialized care, patients are referred to
higher level facilities. Outside OPD hours, patients
are attended to by the staff nurse alone with doctors
being summoned on very rare occasions.
As documented in Shoaib and Ramamohan
(2021), input parameters such as the average num-
ber of arrivals of each type of patient per day (ar-
rival distributions were assumed to be Poisson), and
the service time distribution parameters of the doc-
tor, nurses, laboratory technicians, and the pharma-
cist were estimated based on data collection from
in person visits to multiple PHCs. For example,
the best-fit distribution for the NCD nurse service
time was found to be the uniform distribution with
parameters U(2, 5). Truncated Gaussian distribu-
tions were found to fit the service times of other
Outpatient Diversion using Real-time Length-of-Stay Predictions
59

Figure 1: Outpatient flow at the PHC. Lab = laboratory.
resources - the doctor, laboratory technician, and
pharmacist - best, with parameters N(0.87, 0.21
2
),
N(3.451, 0.873
2
), and N(2.084, 0.723
2
) minutes, re-
spectively. We refer readers to Shoaib and Ramamo-
han (2021) for a complete description of the param-
eter estimation process for other patient types served
by PHCs.
The focus of this analysis is outpatient flow in
the PHCs given that we consider outpatient diver-
sion based on LOS estimates for the PHCs. We ap-
proximate the outpatient flow through the PHC op-
erations as the flow of an entity through one more
M/G/1 queueing systems in series. This approxima-
tion is possible due to the very large disparity in the
arrival rates between outpatients and patients requir-
ing admission (i.e., inpatients and childbirth patients).
This is discussed in further detail in Shoaib and Ra-
mamohan (2021).
Based on the outpatient flow described in Figure 1
and input parameter estimates, we develop a discrete-
event based simulation model of the patient care op-
erations at two PHCs. The programming was done in
Python using the Salabim package on an Intel i7 64-
bit Microsoft Windows operating system with 16 gi-
gabytes of memory. Salabim is a discrete event simu-
lation package in python developed by (van der Ham,
2018). The package provides animation, queues,
states, monitors for data collection and presentation,
and simulation event tracing functionality. A single
replication of the simulation involved a run-time hori-
zon of 365 days with a warm-up period of 180 days.
Each replication required approximately 4 minutes
of computational run-time. We collect data from 40
replications and report the means and standard devi-
ations of key performance measures at both PHCs in
Table 2.
From Table 2, we observe that the average pa-
tient LOS at PHC
2
is significantly higher than that
of PHC
1
. We also note a similar trend in other per-
formance measures such as resource utilizations and
average wait time for all the staffs involved in pro-
viding medical care to outpatients at both PHCs. We
also see that the individual wait times at each queue-
ing subsystem within PHC
2
do not appear to be pro-
hibitively long in themselves; however, as the over-
Table 2: PHC simulation outcomes.
Outcomes* PHC
1
+
PHC
+
2
(9/1/1/1/1) (2/1/1/1/1)
ρ
doc
0.392 (0.003) 0.935 (0.003)
ρ
NCD
0.512 (0.006) 1.475 (0.019)
ρ
phar
0.383 (0.003) 1.705 (0.007)
ρ
lab
0.317 (0.005) 1.417 (0.019)
w
opd
0.036 (0.001) 0.235 (0.002)
w
phar
0.243 (0.005) 27.93 (0.618)
w
lab
0.593 (0.012) 17.47 (0.419)
w
NCD
0.629 (0.023) 30.12 (0.830)
LOS 7.180 (0.033) 57.31 (1.154)
+
Outpatient interarrival time (in minutes)/number of
doctors/number of NCD nurse/number of laboratory tech-
nicians/number of pharmacists.
∗
Resource utilizations
(ρ) are dimensionless fractions, wait times (w), and average
lengths of stay (LOS) are in minutes.
∗
ρ
doc
: doctor’s utilization, ρ
NCD
: NCD nurse’s utilization,
ρ
phar
: pharmacist’s utilization, ρ
lab
: laboratory technician’s
utilization, w
opd
: OPD queue wait time, w
phar
: pharmacy
queue wait time, w
lab
: laboratory queue wait time, w
NCD
:
NCD nurse queue wait time.
all LOS in the facility is considerable given the sig-
nificantly lower service times (for example, the av-
erage consultation time with the doctor is less than
one minute) at these individual subsystems within the
PHC. These observations motivated the development
of a diversion mechanism for outpatients based on
LOS predictions, which we now describe.
4 OUTPATIENT DIVERSION
MECHANISM
The diversion mechanism for outpatients that we de-
velop is depicted in Algorithm 1. We describe this
mechanism using the case of a specific patient whose
assigned PHC is PHC
1
. We consider one other PHC,
which we call as PHC
2
(located farther from the pa-
tient than PHC
1
), as a potential destination for diver-
sion; however, our approach can be extended to any
number of facilities in a healthcare network. As dis-
cussed in Section 1, we assume that the patient can
ICORES 2022 - 11th International Conference on Operations Research and Enterprise Systems
60

access an IT system - either a web-based or smart-
phone application - that communicates the LOS pre-
dictions at PHC
1
and PHC
2
, and assigns the appro-
priate PHC to the patient based on these predictions.
We assume that the patient accesses the application
at time t, implying that the LOS prediction must be
generated at time t; however, the LOS at each PHC
must be estimated at the time the patient is likely to
arrive at the facility in question. Thus, while the pre-
diction is made at time t, the LOS must be estimated
at time t + δ
1
or t + δ
2
, where δ
1
and δ
2
are the travel
times of the patient to PHC
1
and PHC
2
. If we denote
these LOS estimates as LOS
t+δ
1
and L OS
t+δ
2
, then
the patient is assigned the facility with the smaller of
LOS
t+δ
1
and LOS
t+δ
2
.
Algorithm 1: Outpatient diversion mechanism.
1: At time t, estimate LOS
t+δ
1
at PHC
1
2: At time t, estimate LOS
t+δ
2
at PHC
2
3: Visit PHC with LOS = min{L
t+δ
1
, L
t+δ
2
}
We note here that for the purposes of this study,
we assume that the patient is required to visit the as-
signed PHC, and incurs some penalty if they visit any
other facility in the network; however, this mecha-
nism, if adopted, is realistically more likely to pro-
vide a choice to the patient. In such situations the
probability of compliance with the diversion or facil-
ity assignment suggestion must be considered in the
analysis. We do not explore this in our study, and
leave it as an immediate avenue of future research.
Another consideration here is that the diversion
decision can be based on whether the sum of travel
time to the PHC under consideration plus predicted
LOS at the PHC is less than the corresponding quan-
tity at the other PHCs in the network. We do not con-
sider this case in our current version of the LOS-based
diversion mechanism; this is because we wish to in-
troduce this real-time LOS prediction based diversion
mechanism in its simplest form (i.e., based only on
predicted LOS at each facility). However, the diver-
sion mechanism in Algorithm 1 can easily be mod-
ified to take such additional considerations into ac-
count, and we intend to explore this specific consid-
eration in future work. Note also that the estimates of
travel times used in the above algorithm can be con-
sidered to be average values; however, the actual val-
ues used in the diversion algorithm can be real-time
estimates obtained from applications such as Google
Maps depending upon the application process inter-
face links that can be integrated into the IT system
used for deployment of the diversion mechanism.
It is evident that the key steps within the diversion
mechanism in Algorithm 1 are the estimation of the
LOSs L
t+δ
1
and L
t+δ
2
. We now describe how these
LOS predictions are generated.
4.1 Real-time LOS Prediction
As discussed in Section 3, we approximate the outpa-
tient care process at the PHC as receiving care from
one or more M/G/1 systems in series. The four pos-
sible M/G/1 system pathways for an outpatient in the
PHC have also been depicted in Figure 1. We estimate
the LOS in the PHC as the sum of the LOSs in each
of the M/G/1 subsystems where the patient is likely to
receive service.
LOS
phc
= LOS
doc
+ LOS
NCD
+ LOS
lab
+ LOS
pharmacy
(1)
The terms in equation 1 are self-explanatory. We
note here that for LOS
phc
to be as accurate as pos-
sible, the LOSs associated with the laboratory and
NCD nurse queueing systems must be weighted with
the probabilities that the patient avails of service from
these subsystems. However, we do not do this be-
cause of precendence in the literature regarding pro-
viding quantiles higher than the 50
th
quantile of the
distribution of the predicted delay - or in this case, the
predicted LOS - to increase customer satisfaction in
queues (Whitt, 1999; Ibrahim, 2018). Note that this
implies that we overestimate the LOS; however, given
that each of the terms in equation 1 scales in the same
manner with patient load, and does so to the same ex-
tent for all facilities considered, the diversion decision
itself is not affected by this overestimation. Each LOS
term in the right-hand side of equation 1 is estimated
as the sum of the prediction of the delay experienced
by the patient at the M/G/1 system under question and
the average service time at the system. This is given
in equation 2 below.
LOS
s
= d
s
+ E[s], ∀ s ∈ S (2)
In equation 2, s is a subscript indicating an
M/G/1 queueing subsystem in the PHC, and s ∈ S =
{doc, NCD, lab, pharmacy}. d
s
represents the esti-
mated delay for the patient at a given M/G/1 subsys-
tem, and E[s] represents the expected value of the ser-
vice time. The estimated delay d
s
is in turn estimated
as a function of the number of patients ahead of the
patient under consideration in the queue, and the ex-
pected remaining service time for the patient currently
receiving service at the queueing system. This is ex-
pressed below.
d
s
= L
q(s)
E[s] + r
e
, ∀ s ∈ S (3)
In equation 3, L
q(s)
represents the number of pa-
tients ahead of the patient under consideration in the
queue at subsystem s, and r
e
represents the prediction
Outpatient Diversion using Real-time Length-of-Stay Predictions
61

of the remaining service time given that the elapsed
service time for the patient receiving service is x. We
now discuss how r
e
is generated. For M/G/1 systems,
the estimation of r
e
is traditionally done as in equa-
tion 4. In equation 4, T is the random variable repre-
senting the service time (t is thus its realization), G is
the cd f of the service time.
P(T ≤ t|x) =
P(x ≤ T ≤ t + x)
P(T ≥ x)
=⇒ G(t|x) =
G(t + x) − G(x)
1 − G(x)
(4)
r
e
is then estimated as the expected value of the
remaining service time by calculating the pd f g(t|X)
from equation 4. However, performing this calcu-
lation can prove tedious depending upon the nature
of the distribution G(t|x) (Fatma and Ramamohan,
2021b). For example, computing r
e
via equation 4
for the triangular distribution requires working with a
piecewise continuous cd f , and for the Gaussian dis-
tribution requires numerical computation of the inte-
grals involved in computation of r
e
(which involve
the Gaussian error function). Therefore, we propose
an alternate delay predictor for such systems, which
can potentially also be extended to multi-class multi-
server queueing systems, that is considerably easier to
compute and implement. This delay predictor is given
below.
r
e
=
G
−1
(0.5) − x , 0 ≤ x < G
−1
(0.5)
G
−1
(0.75) − x , G
−1
(0.5) ≤ x < G
−1
(0.75)
(b−x)
2
, G
−1
(0.75) ≤ x ≤ b
(5)
Here, r
e
is estimated depending upon the range in
which the elapsed service time x of the patient cur-
rently in service lies with respect to the service time
distribution. G
−1
(0.5), and G
−1
(0.75) are the 50
th
and 75
th
quantiles of the service time distribution, re-
spectively, and b is the extreme quantile (e.g., equal to
G
−1
(0.99)) or the upper limit of the service time cd f
(e.g., where the cd f has bounded support).
r
e
as estimated from equation 5 can then be used
in conjunction with equations 3 and 2 to estimate the
LOS at the subsystem under consdieration. This com-
putation would suffice if the LOS prediction is re-
quired to be made at time t; however, we require LOS
predictions at time t + δ, where δ is the time required
for the patient to arrive at the PHC. LOS predictions
at time t + δ are generated as follows.
In order to calculate the LOS prediction at time
t + δ, we must first estimate the effective average
queue length at t + δ, L
q(t+δ)
, as a function of the
queue length at time t, given by L
q(t)
. This can be ac-
complished using the average post-diversion patient
arrival and service rates, λ
e
and E[s], respectively.
This is given below.
L
q(t+δ)
= L
q
+ (λ
e
− 1) −
max
δ − r
e(t)
E[s]
, 0
(6)
In equation 6, we substract 1 from λ
e
to account
for the patient under consideration for diversion, and
the third term on the right hand side represents the av-
erage number of patients that can be served in δ time
units after taking into account the remaining service
time r
e(t)
of the patient in service at time t. The av-
erage elapsed service time at time t + δ, denoted by
x
t+δ
, is thus estimated as the remainder of
δ−r
e(t )
E[s]
, and
the average remaining service time at t + δ, denoted
by w
e(t+δ)
, is estimated by inputting x
t+δ
into equa-
tion 5. The expected delay at time t + δ for a patient
arriving to subsystem s, d
s(t+δ)
, can thus be estimated
by inputting L
q,s(t+δ)
and r
e,s(t+δ)
into equation 3, and
the LOS at time t + δ can in turn be generated using
the value of d
s(t+δ)
in equation 2. This is summarized
in equation 7 below.
LOS
s(t+δ)
= d
s(t+δ)
+ E[s]
where d
s(t+δ)
= L
q,s(t+δ)
E[s] + r
e,s(t+δ)
(7)
The LOS at subsystem s estimated from equa-
tion 7 can be used to calculate the LOS at each of
the subsystems in S, and then summed per equation 1
to yield the total LOS at the PHC. Note that the LOS
prediction at each subsystem must be calculated at the
point at which the predicted LOS at the previous sub-
system ends. This process of successively calculating
the LOSs is summarized in Algorithm 2.
Algorithm 2: Calculation of the total LOS at a PHC.
1: Initialize with the ordered tuple S
ord
=
(NCD, doc, lab, pharmacy), δ = travel time
to the PHC, current time t, LOS
tot
= 0.
2: for s ∈ S
ord
do
3: Estimate LOS at s at time t + δ as LOS
s(t+δ)
.
4: LOS
tot
= LOS
tot
+ LOS
s(t+δ)
.
5: δ = δ + LOS
s(t+δ)
We must mention here that in the implementation
of the above algorithm, the arrival rate at each sub-
system is assumed to be the same - that is, λ
e
. This is
possible only because we assume that patients visit all
subsystems in series (Hopp and Spearman, 2011), and
we consider relaxing this assumption as an immediate
avenue of future work. We describe the outcomes of
implementing the diversion mechanism in the follow-
ing section.
ICORES 2022 - 11th International Conference on Operations Research and Enterprise Systems
62
We also note here that the deployment and gen-
eration of these LOS predictions is unlikely to incur
significant computational expense, regardless of the
size of the facility network. This is because the gen-
eration of the LOS predictions at a facility involves
just a single function evaluation, and this will remain
the same regardless of the type of LOS predictor in-
volved - for example, a queueing theory based predic-
tor or a statistical learning based predictor. However,
the specific LOS predictor to be employed must be se-
lected taking into account the number of system state
variables that are required for LOS prediction. For ex-
ample, if a particular LOS predictor requires a large
number of system state variables to be recorded and
updated at high frequency, then the complexity of the
IT system required for this purpose will also increase.
On the other hand, if another LOS predictor is avail-
able that requires significantly fewer variables to be
recorded at a small loss of predictor accuracy, then it
might be prudent to choose this latter LOS predictor
from the standpoint of ease of deployment.
Now, based on the real-time LOS estimates gener-
ated using Algorithm 2, we can implement the diver-
sion mechanism in Algorithm 1.
5 SIMULATION EXPERIMENTS
In this section, we present results from implementing
the diversion mechanism described in Algorithm 1.
We compare the operational outcomes at both PHCs
for three cases: (a) without diversion, (b) diversion
implemented using actual real-time LOS estimates
(which are available to the simulation modeler), and
(c) the real-time LOS predictions generated using the
methodology described in Section 4.1. Before we
present the operational outcomes, we discuss the ac-
curacy of the real-time LOS predictor.
We characterize the accuracy of the LOS predic-
tor using the mean absolute percentage error (MAPE)
score, which is given by the formula MAPE =
1
N
N
∑
i=1
LOS
a,i
−LOS
p,i
LOS
a,i
. Here LOS
a,i
is the actual LOS
estimate of the i
th
patient and LOS
p,i
is the predicted
LOS estimate of the i
th
patient and N is the number
of patients in the sample. When LOS predictions are
generated for the two PHCs that we consider (PHC
1
and PHC
2
) in the first set of computational experi-
ments that we describe in the following paragraphs,
we find that the MAPE scores are 13.00% and 18.14%
at PHC
1
and PHC
2
, respectively. While this appears
to indicate reasonable performance of the LOS pre-
dictor, several avenues of improvement of the predic-
tor remain, which we discuss in the following section.
In Table 3, we report results from the implementa-
tion of the diversion mechanism for PHC
1
and PHC
2
with operational parameters corresponding to those
described in Table 2. Given that diversion is likely
to make the utilization of resources more equitable
across a network of facilities, and due to space lim-
itations, we report the mean and standard deviation
of the percentage difference between operational out-
comes such as resource utilizations, wait time, and
average LOSs across both healthcare facilities in Ta-
ble 3. We also report the percentage of patients who
are diverted - that is, those who visit a PHC than their
assigned PHC. We report these outcomes for the three
cases discussed in the above paragraphs.
Table 3: Outpatient diversion: operational outcomes across
both PHCs.
Outc-
omes
No diver-
sion
With actual
LOS
With pre-
dicted LOS
∆
ρ
doc
58.09 (0.36) 5.91 (0.03) 15.60 (0.01)
∆
ρ
ncd
65.26 (0.58) 7.82 (0.02) 13.50 (0.02)
∆
ρ
phar
77.52 (0.18) 16.33 (0.02) 22.20 (0.04)
∆
ρ
lab
77.59 (0.45) 10.30 (0.03) 18.02 (0.06)
∆
w
opd
84.53 (0.38) 4.07 (0.02) 46.77 (0.03)
∆
w
phar
99.12 (0.02) 51.55 (0.08) 74.28 (0.03)
∆
w
lab
96.60 (0.09) 37.95 (0.05) 79.03 (0.04)
∆
w
ncd
97.91 (0.10) 14.12 (0.10) 86.16 (0.02)
∆
LOS
87.46 (0.26) 10.21 (0.04) 63.41 (0.08)
β
∗
0.00 (0.00) 30.95 (2.98) 45.25 (1.48)
∆
ρ
doc
= difference in doctor’s utilization, ∆
ρ
NCD
= difference in NCD nurse utilization,
∆
ρ
phar
= difference in pharmacist’s utilization, ∆
ρ
l ab
= difference in laboratory techni-
cian’s utilization, ∆
w
opd
= difference in OPD queue wait time, ∆
w
phar
= difference in
pharmacy queue wait time, ∆
w
l ab
= difference in laboratory queue wait time, ∆
w
NCD
=
difference in NCD nurse queue wait time, β
∗
= proportion (%) of outpatients who are
diverted.
It is evident from Table 3 that implementing di-
version leads to significantly more equitable opera-
tional outcomes across both PHCs. Without diver-
sion, as seen from Table 2, the LOS at PHC
2
was
57.31 minutes in comparison to an LOS of 7.18 min-
utes at PHC
1
. When diversion is implemented using
the actual real-time LOS estimates, we see that the
LOS at PHC
2
reduces to 15.33 minutes whereas the
LOS at PHC
1
increases to 13.75 minutes. With diver-
sion implemented using the real-time LOS predictor,
we see LOSs of 25.92 minutes at PHC
1
and 9.50 min-
utes at PHC
2
. Thus it is clear that diversion, even
using the real-time LOS predictor, yields a reduction
in LOS at the more heavily utilized system.
From Table 3, we see similar trends in the other
outcomes as well when diversion is implemented us-
ing the real-time LOS predictor. Overall, we see a
significant decrease in the congestion in PHC
2
. A key
observation is that the extent to which operational out-
Outpatient Diversion using Real-time Length-of-Stay Predictions
63

comes become equitable across both PHCs depend on
the accuracy of the delay predictor employed - that is,
the relative difference in a resource’s utilization or the
wait time at a subsystem increases with a decrease in
the accuracy of the delay predictor used. Another im-
portant observation is that the proportion of patients
diverted also increase with decrease in delay predic-
tor accuracy. However, this is likely due to the sig-
nificant difference in the outpatient loads between the
two PHCs prior to implementing diversion - that is, an
average interarrival time of 9 minutes at PHC
1
com-
pared to an average interarrival time of 2 minutes at
PHC
2
.
In order to check how the operational outcomes
change with diversion when the difference in outpa-
tient loads across both PHCs is not as high as in the
previous case, we conducted a sensitivity analysis by
changing the average interarrival times of outpatients
to 2 minutes at PHC
1
and 4 minutes at PHC
2
. We
present the results from this sensitivity analysis re-
sults in Table 4 and observe similar trends in the oper-
ational outcomes across both PHCs as observed in Ta-
ble 3. We note that the MAPE scores of the real-time
LOS predictor that we propose at PHC
1
and PHC
2
were found to be 13.82% and 18.33% respectively,
respectively.
Table 4: Sensitivity analysis: operational outcomes across
both PHCs.
Outc-
omes
No diver-
sion
With actual
LOS
With pre-
dicted LOS
∆
ρ
doc
37.28 (0.41) 18.82 (0.05) 24.91 (0.01)
∆
ρ
ncd
41.92 (0.85) 19.84 (0.04) 26.68 (0.02)
∆
ρ
phar
49.92 (0.85) 22.96 (0.04) 34.08 (0.01)
∆
ρ
lab
50.02 (1.07) 24.28 (0.04) 33.29 (0.02)
∆
w
opd
60.01 (0.84) 11.52 (0.05) 17.13 (0.07)
∆
w
phar
96.19 (0.08) 46.19 (0.07) 64.84 (0.03)
∆
w
lab
87.59 (0.52) 44.81 (0.09) 71.24 (0.03)
∆
w
ncd
92.52 (0.23) 29.18 (0.07) 71.24 (0.03)
∆
LOS
83.15 (0.29) 31.48 (0.07) 78.96 (0.01)
β
∗
0.00 (0.00) 45.37 (0.78) 36.69 (0.10)
∆
ρ
doc
= difference in doctor’s utilization, ∆
ρ
NCD
= difference in NCD nurse utilization,
∆
ρ
phar
= difference in pharmacist’s utilization, ∆
ρ
l ab
= difference in laboratory techni-
cian’s utilization, ∆
w
opd
= difference in OPD queue wait time, ∆
w
phar
= difference in
pharmacy queue wait time, ∆
w
l ab
= difference in laboratory queue wait time, ∆
w
NCD
=
difference in NCD nurse queue wait time, β
∗
= proportion (%) of outpatients who are
diverted.
Once again, as expected, we notice that the ex-
tent to which operational outcomes become equitable
across both PHCs decreases with a decrease in the
accuracy of the LOS predictor employed. However,
when compared to the corresponding outcome in Ta-
ble 3, we notice the proportion of patients diverted
actually decreases with a decrease in the accuracy of
the LOS predictor. That is, in this case, the proportion
diverted decreases with the less accurate LOS predic-
tor. Thus, our results indicate that the proportion of
patients diverted across a healthcare facility network,
when diverted on the basis of real-time LOS predic-
tions, depend on both the accuracy of LOS predictor
employed as well as the differences in patient loads
across the facilities within the network.
Overall, it is evident that outpatient diversion us-
ing real-time LOS predictions appears to improve op-
erational performance of a healthcare facility network
from both the provider as well as patient standpoints.
We now conclude our work with a discussion of
the contributions of our work and avenues for further
research.
6 DISCUSSION & CONCLUSIONS
In this work, we present preliminary results from the
simulated implementation of a framework for outpa-
tient diversion using real-time LOS predictions. We
emphasize here that the real-time LOS predictions
and the diversion decision are made at the point of
origin of the patient, as opposed to when the patient
arrives at a healthcare facility. We empirically show
via DES that patient diversion results in more equi-
table utilization of resources across the healthcare fa-
cilities that we consider when compared to the case
without diversion. The diversion framework that we
propose can also be repurposed for real-time facility
assignment in health systems where patients are not a
priori assigned their first point of contact for medical
care.
To the best of our knowledge, our study is the
first of its kind that considers real-time LOS predic-
tions in initiating diversion across healthcare facili-
ties. Previous studies initiated diversion using fac-
tors such as average wait time, number of beds occu-
pied, number of patients in waiting queue. Further, we
demonstrate how LOS can become a criterion for di-
version especially when diversion of non-emergency
patients, and in particular outpatients, is considered.
Once again, we did not come across a previously pub-
lished study that considered outpatient diversion. Fi-
nally, to our knowledge, our study is also the first to
develop a methodology for the real-time estimation
of LOSs in the near future. This in turn utilizes a
novel approximation of the real-time delay predictor
for M/G/1 queueing systems. In comparison to most
studies in the literature that utilize LOS predictors
based on statistical learning methods, our analytical
approach grounded in queueing theory may be easier
to program and deploy in practice. Further, our ap-
ICORES 2022 - 11th International Conference on Operations Research and Enterprise Systems
64

proach also opens up avenues for leveraging the sub-
stantial body of work regarding real-time delay pre-
diction for real-time LOS-based diversion for more
complex queueing systems than that encountered in
this study.
A key avenue of future research involves improv-
ing the accuracy of the real-time LOS predictor that
we develop in this study. While the accuracy of
our real-time LOS predictor appears reasonable, with
MAPEs not exceeding 20%, relaxing our assump-
tion that all patients avail service from all subsystems
within the PHC is likely to improve the accuracy of
the predictor. A related direction for future work in-
volves benchmarking our work against statistical ma-
chine learning based predictors of LOS, and assessing
how the operational outcomes compare with respect
to the outcomes associated with our queueing theory
based predictor. Similarly, our LOS based diversion
mechanism can also be compared to other diversion
mechanisms, such as wait-time based mechanisms.
A key question that arises here is how the imple-
mentation of the diversion mechanism in Algorithm 1
would scale in terms of computational and operational
overheads when the size of the network increases.
One of the questions that must be answered prior to
deploying this approach in a larger network would in-
volve determining, for each facility in the network,
the set of facilities at which real-time LOS predictions
must be generated in order to determine the diversion
decision. For example, in a network with 1,000 fa-
cilities, in order to determine the diversion decision
for a patient, real-time LOS predictions need not be
generated at each of the 1,000 PHCs (as many would
be located at a significant distance from the patient’s
assigned PHC). Thus determining the optimal set of
facilities that need to be considered as diversion des-
tinations for a given facility in a large network be-
comes an important avenue of future research when
considering the scaling of this approach to larger fa-
cility networks. As part of this, an immediate avenue
of research we are pursuing includes expanding this
diversion framework to the entire network of 9 PHCs
in the Indian district that we consider, and we plan to
answer the above question for this network.
Finally, another avenue of future research is ex-
tending our work to more complex queueing systems,
including multi-class multi-server systems, which
may be applicable in the case of diversion of inpa-
tients or emergency patients. These more complex
queueing systems can include queueing systems with
non-stationary arrival and service processes. Real-
time delay predictors have been developed for certain
queueing systems with non-stationary arrival, service
or abandonment processes (Ibrahim, 2018); and LOSs
for such systems may correspondingly be calculated
in a manner similar to that which we have described
in this paper. However, in case the non-stationarity is
not complex - for example, increased arrival rates may
be observed during the weekends, and arrival rates re-
main the same during all weekdays - then the method-
ology described for LOS prediction in this paper can
directly be applied by just changing the arrival rates
in the LOS predictor expressions depending upon the
day of the week.
REFERENCES
Adjerid, I., Adler-Milstein, J., and Angst, C. (2018). Reduc-
ing medicare spending through electronic health infor-
mation exchange: the role of incentives and exchange
maturity. Information Systems Research, 29(2):341–
361.
Aghajani, S. and Kargari, M. (2016). Determining factors
influencing length of stay and predicting length of stay
using data mining in the general surgery department.
Hospital Practices and Research, 1(2):53–58.
Alsinglawi, B., Alnajjar, F., Mubin, O., Novoa, M., Alor-
jani, M., Karajeh, O., and Darwish, O. (2020). Pre-
dicting length of stay for cardiovascular hospitaliza-
tions in the intensive care unit: Machine learning ap-
proach. In 2020 42nd Annual International Confer-
ence of the IEEE Engineering in Medicine & Biology
Society (EMBC), pages 5442–5445. IEEE.
Arefian, H., Hagel, S., Fischer, D., Scherag, A., Brunkhorst,
F. M., Maschmann, J., and Hartmann, M. (2019).
Estimating extra length of stay due to healthcare-
associated infections before and after implementation
of a hospital-wide infection control program. PloS
One, 14(5):e0217159.
Ayyoubzadeh, S. M., Ghazisaeedi, M., Kalhori, S. R. N.,
Hassaniazad, M., Baniasadi, T., Maghooli, K., and
Kahnouji, K. (2020). A study of factors related to pa-
tients’ length of stay using data mining techniques in a
general hospital in southern iran. Health Information
Science and Systems, 8(1):1–11.
Baek, H., Cho, M., Kim, S., Hwang, H., Song, M., and
Yoo, S. (2018). Analysis of length of hospital stay
using electronic health records: A statistical and data
mining approach. PloS One, 13(4):e0195901.
Barnes, S., Hamrock, E., Toerper, M., Siddiqui, S., and
Levin, S. (2016). Real-time prediction of inpatient
length of stay for discharge prioritization. Jour-
nal of the American Medical Informatics Association,
23(e1):e2–e10.
Blanchard, J., Washington, R., Becker, M., Vasanthakumar,
N., Gopal, K. M., and Sarwal, R. (2021). Vision 2035
public health surveillance in india.
Deo, S. and Gurvich, I. (2011). Centralized vs. decen-
tralized ambulance diversion: A network perspective.
Management Science, 57(7):1300–1319.
Dong, J., Yom-Tov, E., and Yom-Tov, G. B. (2019). The
impact of delay announcements on hospital network
Outpatient Diversion using Real-time Length-of-Stay Predictions
65

coordination and waiting times. Management Science,
65(5):1969–1994.
El-Bouri, R., Taylor, T., Youssef, A., Zhu, T., and Clifton,
D. A. (2021). Machine learning in patient flow: a re-
view. Progress in Biomedical Engineering.
Fatma, N., Mohd, S., Ramamohan, V., and Mustafee, N.
(2020). Primary healthcare delivery network simu-
lation using stochastic metamodels. In 2020 Winter
Simulation Conference (WSC), pages 818–829. IEEE.
Fatma, N. and Ramamohan, V. (2021a). Patient diversion
across primary health centers using real time delay
predictors. In 2021 Institute of Industrial and Systems
Engineers (IISE) Annual Conference & Expo.
Fatma, N. and Ramamohan, V. (2021b). Patient diversion
using real-time delay prediction across healthcare fa-
cility networks. http://web.iitd.ac.in/
∼
mez188287/NF.
pdf, accessed 29
th
November 2021.
Guti
´
errez, J. M. P., Sicilia, M.-
´
A., Sanchez-Alonso, S.,
and Garc
´
ıa-Barriocanal, E. (2021). Predicting length
of stay across hospital departments. IEEE Access,
9:44671–44680.
Hijry, H. and Olawoyin, R. (2020). Application of ma-
chine learning algorithms for patient length of stay
prediction in emergency department during hajj. In
2020 IEEE International Conference on Prognostics
and Health Management (ICPHM), pages 1–8. IEEE.
Hopp, W. J. and Spearman, M. L. (2011). Factory physics.
Waveland Press.
Ibrahim, R. (2018). Sharing delay information in ser-
vice systems: a literature survey. Queueing Systems,
89(1):49–79.
IPHS-Guidelines (2012). Guidelines for Primary Health
Centres. Directorate General of Health Services, New
Delhi, India.
Li, M., Vanberkel, P., and Carter, A. J. (2019). A review
on ambulance offload delay literature. Health Care
Management Science, 22(4):658–675.
Liu, Y., Zhong, L., Yuan, S., and van de Klundert, J. (2018).
Why patients prefer high-level healthcare facilities: a
qualitative study using focus groups in rural and urban
china. BMJ Global Health, 3(5):e000854.
Marquinez, J. T., Saur
´
e, A., Cataldo, A., and Ferrer, J.-C.
(2021). Identifying proactive icu patient admission,
transfer and diversion policies in a public-private hos-
pital network. European Journal of Operational Re-
search.
Morley, C., Unwin, M., Peterson, G. M., Stankovich, J., and
Kinsman, L. (2018). Emergency department crowd-
ing: a systematic review of causes, consequences and
solutions. PloS One, 13(8):e0203316.
Mustafee, N. and Powell, J. (2020). Providing real-time
information for urgent care. Impact, 2021(1):25–29.
Nezamoddini, N. and Khasawneh, M. T. (2016). Model-
ing and optimization of resources in multi-emergency
department settings with patient transfer. Operations
Research for Health Care, 10:23–34.
Piermarini, C. and Roma, M. (2021). A simulation-based
optimization approach for analyzing the ambulance
diversion phenomenon in an emergency department
network. arXiv preprint arXiv:2108.04162.
Ramirez-Nafarrate, A., Fowler, J. W., and Wu, T. (2011).
Design of centralized ambulance diversion policies
using simulation-optimization. In Proceedings of
the 2011 Winter Simulation Conference (WSC), pages
1251–1262. IEEE.
Rao, K. D. and Sheffel, A. (2018). Quality of clinical care
and bypassing of primary health centers in india. So-
cial Science & Medicine, 207:80–88.
Shaaban, A. N., Peleteiro, B., and Martins, M. R. O. (2021).
Statistical models for analyzing count data: predictors
of length of stay among hiv patients in portugal using
a multilevel model. BMC Health Services Research,
21(1):1–17.
Sharma, R., Prakash, A., Chauhan, R., and Dhibar, D. P.
(2021). Overcrowding an encumbrance for an emer-
gency health-care system: A perspective of health-
care providers from tertiary care center in northern in-
dia. Journal of Education and Health Promotion, 10.
Shi, P., Helm, J. E., Deglise-Hawkinson, J., and Pan, J.
(2021). Timing it right: Balancing inpatient conges-
tion vs. readmission risk at discharge. Operations Re-
search.
Shoaib, M. and Ramamohan, V. (2021). Simulation mod-
elling and analysis of primary health centre opera-
tions. arXiv preprint arXiv:2104.12492.
Song, H., Tucker, A. L., and Murrell, K. L. (2015). The
diseconomies of queue pooling: An empirical investi-
gation of emergency department length of stay. Man-
agement Science, 61(12):3032–3053.
Turgeman, L., May, J. H., and Sciulli, R. (2017). Insights
from a machine learning model for predicting the hos-
pital length of stay (los) at the time of admission. Ex-
pert Systems with Applications, 78:376–385.
van der Ham, R. (2018). salabim: discrete event simula-
tion and animation in python. Journal of Open Source
Software, 3(27):767.
Verburg, I. W., de Keizer, N. F., de Jonge, E., and Peek,
N. (2014). Comparison of regression methods for
modeling intensive care length of stay. PloS One,
9(10):e109684.
Wachtel, G. and Elalouf, A. (2020). Addressing overcrowd-
ing in an emergency department: an approach for
identifying and treating influential factors and a real-
life application. Israel Journal of Health Policy Re-
search, 9(1):1–12.
Whiteside, T., Kane, E., Aljohani, B., Alsamman, M., and
Pourmand, A. (2020). Redesigning emergency depart-
ment operations amidst a viral pandemic. The Amer-
ican Journal of Emergency Medicine, 38(7):1448–
1453.
Whitt, W. (1999). Predicting queueing delays. Management
Science, 45(6):870–888.
Zhou, Q., Fan, L., Lai, X., Tan, L., and Zhang, X. (2019).
Estimating extra length of stay and risk factors of mor-
tality attributable to healthcare-associated infection at
a chinese university hospital: a multi-state model.
BMC Infectious Diseases, 19(1):1–7.
ICORES 2022 - 11th International Conference on Operations Research and Enterprise Systems
66
