
Exploring Trust Perceptions in the Medical Context: A Qualitative
Approach to Outlining Determinants of Trust in AAL Technology
Sophia Otten
a
and Martina Ziefle
b
Chair of Communication Science, Human-Computer Interaction Centre, RWTH Aachen University,
Campus-Boulevard 57, Aachen, Germany
Keywords: Trust, Medical Care, AAL, Medical System.
Abstract: Due to a demographic change of the society, health care worker shortage and rising co- and multimorbidity
within older adults, constant care at home and at care facilities face a difficult task to combat these challenges.
Medical AAL technology offers many opportunities to relieve health care workers and assist older adults with
difficulties in managing activities of daily life (ADL). This study has adopted an exploratory interview
method to explore the users’ perceptions of trust in the medical context and specifically, related to medical
AAL technologies. Eleven participants ranging from 20 years to 87 years old (M = 52.27; SD = 24.2) were
interviewed and, in line with previous results in the literature, results revealed three categories of influences,
namely user factors, technology factors, and context factors. This implies a network of trust dependent on
various external and internal influences. These findings have practical implications for clinicians, developers,
policy makers and legal professionals.
1 INTRODUCTION
In Europe, the demographic change of the population
puts an increasing strain on the health care system. By
2070, it is estimated that 30% of Europeans are aged
65 years or older which is about 20% more than today
(see European Commission Report on the Impact of
Demographic Change). Due to these prognoses, it is
necessary to explore the possibilities of relieving the
medical system and bringing down the costs of health
care. Moreover, there is a shortage of health care
personnel which is predicted to increase dramatically
in the coming years with an estimated shortage of 4.1
million health care workers in 2030 (Michel &
Ecarnot, 2020). At the same time, older people also
have a desire to live on their own for as long as
possible (Peek et al., 2014). For example, the WHO
introduced a model of active ageing in order to
promote life satisfaction and quality of life (QoL) in
older adults (WHO, 2002). It defines active aging as
“[...] the process of optimizing opportunities for
health, participation and security in order to enhance
quality of life as people age.” (WHO, 2002). Given
the health barriers and comorbidities older people,
a
https://orcid.org/0000-0002-4027-5362
b
https://orcid.org/0000-0002-6105-4729
especially in Western societies face, it is crucial to
connect theories of aging with the demands and
challenges of the health care system.
There are several approaches trying to tackle these
problems, one of them being active and assisted living
technologies (AAL technologies) designed to
enhance QoL and independence in older adults. These
solutions include wearable or ambient-installed
sensors, actuators, and smart interfaces that are
integrated into the homes of older adults. In this
context, most devices are used for lifelogging which
refers to the digital tracking and documentation of
behavioural and physiological data in order to extract
knowledge about a person’s health status and
behaviour (Climent-Perez et al., 2020; Steinke et al.,
2012). Given the challenges the health care system
faces at the moment and in the future, it is of
relevance to introduce and integrate these
technologies into the lives of older adults still living
at home but also to those living in care facilities.
Studies have shown that there are benefits but also
barriers of acceptance in the user population (Himmel
& Ziefle, 2016; Jaschinski & Allouch, 2015;
Wilkowska et al., 2021). The benefits seen by the
244
Otten, S. and Ziefle, M.
Exploring Trust Perceptions in the Medical Context: A Qualitative Approach to Outlining Determinants of Trust in AAL Technology.
DOI: 10.5220/0011058300003188
In Proceedings of the 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2022), pages 244-253
ISBN: 978-989-758-566-1; ISSN: 2184-4984
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

users are, among other, e.g., the medical security of
instant help, but also the independence of constant
care and comfort, the barriers mostly refer to privacy
and trust issues and data handling and management,
but also usability issues and the fear that technology
does not only assist but potentially replaces human
care (Ziefle & Calero Valdez, 2017; Schomakers et
al., 2021). Users tend to trade-off these benefits and
barriers in their overall evaluation of medical
technology which is why a user-centric view is
important for the implementation of AAL
technologies (Offermann-van Heek & Ziefle, 2019).
However, it is not only the perception of medical
technologies that influences the adoption of such but
also the context surrounding the devices, namely the
quality and the perceived reliability of the medical
system and medical personnel. Trust in the medical
system and health care workers is a core component
of how people perceive medical technology and thus
how open they are to using them in their homes.
There are several conceptualisations of trust in
general, the most common throughout literature being
trust as a belief and expectancy (McKnight &
Chervany, 2001). This study is based on the literature
on trust in medical and non-medical contexts and will
therefore adapt this construct. Trust is made up of
types that each measure a different aspect, i.e.,
dispositional trust (general trusting stance),
institutional or structural trust, and interpersonal trust
(trust in specific others) (McKnight et al., 2011;
Mayer et al., 1995). The combination of the keywords
“TRUST” and “ MEDICAL SYSTEM” on the
database “Web of Science” results in 10,847 hits up
until 2010 whereas up until 2021 there are as many as
53,319 hits on the subject, signalling the growing
interest in the role of trust in medical fields. Qiao et
al. (2015) found that participants’ trust in medical
technology depended on several other context-
dependent variables, such as trust in their primary
care physician and perception of how the physician
uses medical technology. This suggests a complex
network of moderating as well as predictive
relationships regarding trust in medical technology.
Within the broader context of technology, there
are three broad categories of variables that can be
outlined, namely technology factors, user factors, and
context factors (Xu et al., 2014; Bova et al., 2006). In
each category, there are further subgroups that focus
on specific aspects of and around the technology and
the users. While there are studies investigating all
kinds of technology, there is little information about
variables that are specific to the medical technology
context. In relation to that, there is no unified theory
of (the development of) trust across contexts. This
makes it crucial to investigate whether there are
contemporary influences on trust development and
how these fit into the broader concept of trust in the
medical field.
2 QUESTIONS ADDRESSED AND
STRUCTURE OF THE
INTERVIEW PROCEDURE
Based on the existing literature of trust in various
contexts, this study investigates the perceptions of
trust and trust development in a general and medical
context, as well as trust determinants in medical AAL
technology. Within the area of Ambient Assisted
Living (AAL), yet diverse holistic systems and
technical single-case solutions have been developed
in both academia and industry to enable staying at
home longer and independently (Memon et al., 2014;
de Ryter & Pelgrim, 2007, Ziefle, 2021). Still,
sustained adoption of these innovative technologies
in-home environments have failed (Wichert et al.,
2012). Beyond technical and economic reasons as
well as legal barriers towards data usage, one major
barrier could touch the missing trust of caretakers in
the medical technology applied in a very intimate and
sensitive usage context. This study therefore focuses
specifically on users’ trust in the medical context and
medical technology.
It employs a qualitative design with open-ended
questions and scenarios visualising AAL lifelogging
technology. The structure of the interview moves
from general, free association, to specific scenarios.
The first part dealt with perception of trust in general,
in the medical context, and regarding medical AAL
technology. The second part dealt with specific
examples of the medical system and from daily life,
as well as specific scenarios for the participants to
imagine and express their thoughts on trust
development in this context. The exact questions and
their order can be found in the Procedure section. This
was done to gain a first impression of trust
perceptions and only then to narrow in on particular
concerns of trust perceptions of AAL technologies.
Therefore, the first aim is to explore why and under
which conditions people trust the medical system.
The second aim is to explore how and under which
conditions people trust medical AAL technology.
The qualitative approach was chosen to gain
insight into ideographic perspectives of potential
users. Additionally, the exploratory method serves as
a first step into outlining trust perceptions in health
care contexts, i.e. the more specific questions were
Exploring Trust Perceptions in the Medical Context: A Qualitative Approach to Outlining Determinants of Trust in AAL Technology
245

based on previously researched variables across
different contexts to include possible influences that
were not associated with the medical context before.
The theoretical foundation of the questions was based
on previous factors outlined by several studies in the
literature, i.e. technology, user, and context factors.
The purpose of this paper was not to confirm those
previous results but questions were phrased in a way
that allowed participants to mention concerns related
to those factors. The reason of this context-
independent structure was to include other potential
influences and to not limit previous findings to the
medical context in order to avoid bias towards the
research aim. For the purpose of this paper, the quotes
were translated into English.
3 METHODS
3.1 Participants
The final dataset consists of eleven participants with
ages ranging from 20 years to 87 years old (M =
52.27; SD = 24.21). All interviews were conducted in
German as all participants were of German
nationality. The participants were recruited in the
social network of authors and volunteered to take part
in the study. In order to balance the diversity of
participants, they were selected based on gender, age,
and care experience (either professionally or
personally). There were six females and five male
participants. One participant holds a doctorate, nine
participants completed vocational training, and one
participant finished their A-levels. Three of them are
currently enrolled as students at German universities.
Two participants reported to work in the medical field
and four participants reported to have care
experience. Eight participants said to have medium
technical affinity, two participant said they have poor
technical affinity, and one participant said they have
superior technical affinity.
3.2 Open-ended Interviews and Data
Analysis
The interviews were conducted in Germany in
November 2021 with the online application Zoom.
The interviews lasted 30 to 60 minutes and were
divided into a first part, addressing trust in general, in
the medical context, and regarding medical AAL
technology and a more context-related part, in which
specific examples of the medical system and from
daily life were discussed.
Participants answers were analysed using a
qualitative approach, comparing them to existing
factors in the literature. After having evaluated all
points, they were categorised according to previously
established groupings in the literature (Bova et al.,
2006; Xu et al., 2014; Qiao et al., 2015). The analysis
was done with MAXQDA 2018 (VERBI Software,
2019)
3.3 Procedure
At the start of the interview, the participants were
welcomed, received information about the study and
were asked to give informed consent as well as
permission to record the conversations which were
transcribed verbatim and after all interviews took
place. Firstly, they were asked about their perceptions
of trust in general, i.e. what they thought influences
trust and how they deal with trust and distrust in their
daily life. Secondly, they were asked about their
perceptions of trust in the medical context, i.e. what
made them trust in medical workers and institutions.
In the second part, the researcher explained properties
of AAL technologies, emphasising that participants
could picture the technology themselves, as long as
they had some features that are relevant for medical
lifelogging, such as recording vital signs and
detecting falls. Afterwards, the participants were
asked how their perceptions of trust change when
thinking about this type of medical technology and
how human medical care is different than
technological medical care. They were then asked to
rate several examples from their daily life and the
medical contexts according to their level of trust, e.g.
close relatives, medical care personnel, primary care
physician, and health insurance provider. Lastly, they
were presented with a scenario which employs one
form of AAL technology and differs in context-
dependant factors (i.e. living situation, type and
chronicity of disease, whether the scenario concerned
them or a relative, etc.) and asked about their worries
and thoughts on the scenario, and technological
advancements in the medical field altogether. In an
informal last part, they were asked about
demographic information, technological affinity, and
care experience.
4 RESULTS
4.1 Qualitative Findings
Results from the thematic analysis revealed three
major categories of trust predictors, namely user
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
246

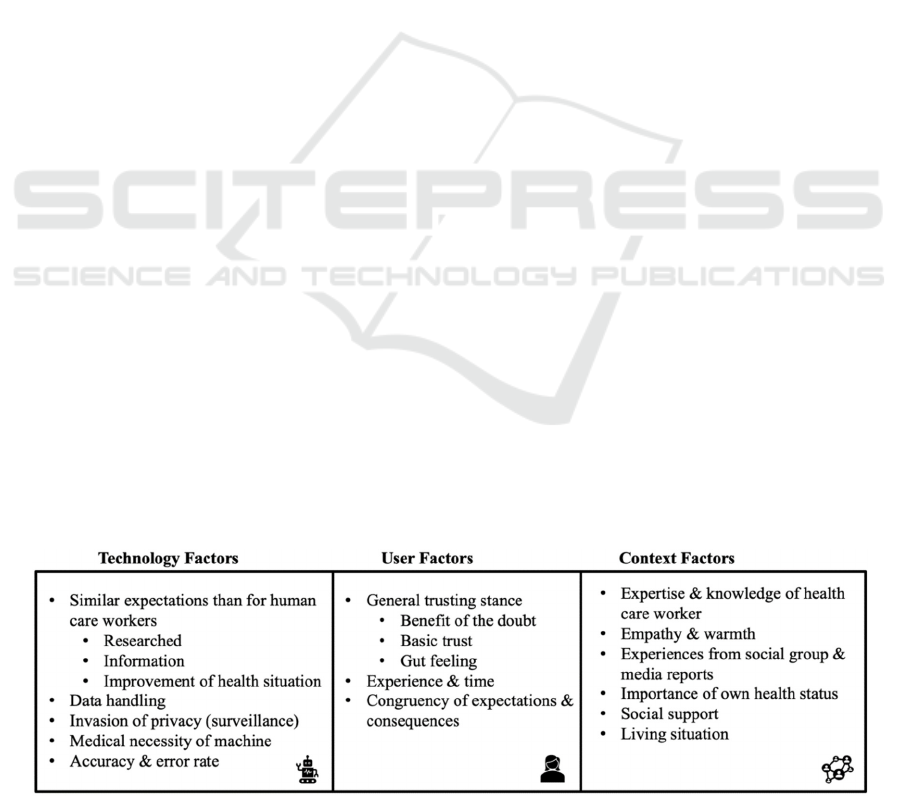
factors, technology factors, and context factors. This
is close to the three categories outlined by previous
research and confirms established patterns of trust
development. An overview of the findings can be
found in Figure 1.
4.1.1 User Factors
Within this category, participants mentioned things
related to dispositions about trust and remarks about
general trusting stance. They mentioned phrases like
“basic trust” [P11] and “benefit of the doubt”[P6]
when referring to interactions with other people.
Moreover, they mentioned that a certain advance in
trust is needed in daily life, without which
interactions of any kind would not be possible. One
participant said that trust is the foundation for a
relationship because it creates intimacy between two
people.
“[without trust] there is a certain distance, I
think trust creates a huge amount of closeness
to a person or a group” [P1]
Overall, they each said that trust is crucial in day-
to-day interactions and depends on the person that the
interactions is with but most importantly, they also
said that trust develops over time and needs to be
fostered to be strengthened.
“trusting someone completely right at the
start, I’d be cautious with that. It develops
over time” [P7]
“a certain basic trust is there but evidently it
grows by doing things together” [P11]
“it depends on how long you’ve known a
person or generally if you know the person”
[P1]
When asked about what generally makes people
trust for the first time, participants often talked about
“intuition”[P5], “chemistry” [P8], and a “gut
feeling” [P8] which, when asked to elaborate, turned
out to be an emotional component that people either
felt they had or did not have. In addition to that,
behavioural components were also important to
participants’ trust feelings. This included experience,
caution, and observation on the trustor’s part but also
a congruency of saying and doing on the trustee’s
side. The participants felt like they needed to be able
to depend on what is being said and to know that the
other side was being honest and sincere with them
which is shown with their actions.
“that the person opposite of me is honest with
me and shares their thoughts and feelings with
me, or at least does not lie about them” [P3]
“that something I am expecting to happen also
comes true in that way” [P5]
“that I feel 100% safe and [...] that things are
not happening behind my back” [P6]
Lastly, the participants were asked about how
they deal with distrust and how they would act if
someone betrayed their trust. Seven participants said
that they would try to trust again but also mentioned
that if there was any doubt about the honesty of the
other person, they would withdraw from the
relationship. Moreover, they said that the other person
had to show their remorse and willingness to be
trusted again. Generally, they all mentioned that it
would take time and was not easy to rebuild and also
depended on the importance and secrecy of the topic.
The other four participants said that no matter how
much time passed and how the other person acted
after the betrayal, they would not fully trust that
person again and would keep their distance about
sharing information and spending time with them.
4.1.2 Technology Factors
In the interview, the participants were asked how their
trust in the medical context differed when thinking
about medical AAL technology. They mentioned
general opinions on medical AAL technology as well
as detailed requirements they would expect from such
devices.
General Aspects. Participants were generally
accepting and enthusiastic about the technology.
They mentioned mostly positive aspects about it and
could picture themselves using it. When questioned
about how trust in medical AAL technology differed
from general trust in the medical context, they said
that there was not much of a difference. More
precisely, they looked for the same qualities that they
also looked for in their physician or care personnel.
In relation to the technology, this included the topic
being researched (their physician being experienced,
having sound medical knowledge), having been
informed about what it does and where the data goes
(honesty and integrity of the physician), and an
improvement of their health situation (benevolence of
care personnel carrying out the medical care). Next to
the positive aspects, some participants also mentioned
concerns which are almost all related to the camera
based AAL technology and included the handling of
data, invasion of privacy, and whether the technology
is merely a way of companies trying to sell things that
are not absolutely necessary. Specifically, one
participant felt strongly that this type of technology
could not provide the kind of warmth, empathy, and
Exploring Trust Perceptions in the Medical Context: A Qualitative Approach to Outlining Determinants of Trust in AAL Technology
247

company that human care could provide and when
given the chance, she would not want it in her home.
“there is something missing and I just
wouldn’t want to use it [...]. Right now, I see it
with my mother because it’s the most beautiful
thing for her when someone stops by, talks to
her, holds her hand [...]. I just think that it is
very important for people, even if it’s just little
things. It’s something the machine can never
give, this kind of warmth.” [P7]
All in all though, they saw AAL technologies as a
possibility of enhancing medical care carried out by
humans and agreed about its benefits to relieve health
care workers, but none of them expect for one
participant could picture this solution as a
replacement of human care. In addition to that, almost
everyone said that they would prefer human care over
technological care, and would only use it if it was
medically indicated.
Specific Requirements. While some people
mentioned that they expected the technology to be
more precise than human medical care, they also said
that they wouldn’t want to rely on it completely. They
argued that because it does not have situational
factors like humans do, i.e. fatigue, traffic, human
error, the technology should work around the clock.
Moreover, one participant expected it to have a 100%
success rate because it should be tested to the point
where it does not make any errors anymore.
“if this technology failed and didn’t notice its
error, if it functioned 90% of the time but
everyone relied on it to work 100% of the time,
it would quickly become dangerous to the
person in need of care [...]. Right, that’s why
it needs to work 100% 24/7 for me to trust it.”
[P1]
“Well, if humans made an error I wouldn’t be
as pissed as if a machine made an error” [P5]
On the other hand, one participant said that as
long as it added to her overall medical care, she would
accept a certain error rate. This participant, however,
also said that she would check the accuracy of the
system beforehand as she herself works as an ICU
nurse.
“The more ‘false alarms’, the less people
react to it but someone will still come. Well, I
can still be sure that if I’m lying on the ground
and can’t call for help myself, that even if it’s
not in five minutes, somebody will come to
check on me in half an hour.” [P10]
Other participants felt like they could never
expect as much from a piece of technology than they
could from a health care worker. They felt like the
technology could be an addition but would always
have to be checked by a human. Across those
interviews, there was a discrepancy when these
participants were asked about the technology itself
and when asked to picture themselves in a scenario
where they would use it. In the scenario, they referred
to the human care as superior but when only asked
about the technology, they referred to it as being more
objective and accurate that human judgement.
4.1.3 Context Factors
After exploring general trust perceptions, participants
were asked about how trust manifested in the medical
context. Strikingly, all participants first spoke of
physicians when talking about medical trust. They
mentioned that, similar to general trust perceptions,
chemistry was a major component. Specifically, most
participants needed to feel that the physician had the
suited expertise and knowledge to treat them. In
relation to that, the outcome of previous patients was
also of importance. This was summarised as the
“word of mouth” [P1] in their social groups and in
media reports. On an emotional level, about half of
the participants wanted to “feel heard and listened
to” [P9] and that the physician paid attention to their
problems. This was summarised as empathy towards
the patient. The other half did not mention this as a
particularly important aspect, and one participant
thought it was not necessary for successful medical
treatment altogether.
Mostly participants that did not work in the
medical context felt that trust in the medical context
was more important than in other context as it
concerned their personal well-being and health.
Moreover, they said that there was no way for them
to verify the information given by the physician other
than seeing another medical professional.
“especially in the medical context [trust]
needs to be bigger because it is about your
own body and not about whether your kitchen
is even or your house is built well” [P1]
“it’s the same thing when the nurse says that
the medication is correctly prescribed and
given out but in reality someone messed it up,
then that’s something that influences trust, in
particular when it’s about body and soul”
[P3]
“without trust you wouldn’t want to place your
body in the hands of that person [physician]”
[P4]
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
248
Conversely, one participant who is a trained
physician mentioned that experience of the treating
physician was not only unimportant but was even a
negative aspect for her, as she felt that having treated
many patients was not predictive of competence and
most often associated with unjustified confidence.
“[Experience] is more of a negative factor,
actually, because I have experienced that
physicians who insist on having experience
usually don’t pay attention to details
anymore” [P5]
Taking these concerns together, it becomes
evident that most of the subsequent behaviour of
patients is related to how they perceive their treating
physician and care personnel. “Medical context” is a
term that all participants related to people, in
particular physicians. When asked about medical
technology, almost all of them connected it to the
conditions under which it would be introduced to
them, i.e. whether their physician appeared to
understand it themselves, whether it was covered by
their insurance, and whether they would receive
assistance in using it. Overall, it was clear that if they
trusted the medical personnel they were closest to,
they were more willing to try the technology as well.
However, if they felt disregarded and suspicious of
the intentions of health care workers, they would not
want to use the technology or risk having their data
be stored in medical files.
“as with the technology I’d say that that the
human is part of it, if the person explains to me
why this technology is useful and what it can
do, then I’d trust it for now” [P2]
“my first thought is that I wouldn’t trust the
care personnel that gets these alarms in the
end. [...] I’d trust the technology, yes, but I’d
question the people behind the system” [P4]
“the entire clinical staff should have
knowledge about this technology for me to
trust it” [P2]
These points suggest that the way of introducing
AAL technology is highly relevant for the acceptance
and willingness of potential users in this context.
However, there are other context factors that were
mentioned to be important as well. Participants felt
good about AAL technology, if it relieved the burden
on family members. They felt that they would most
likely try out the technology if they otherwise had to
rely on their family members to care for them. On the
other hand, they also felt more comfortable using the
technology if they lived alone and without social
support. The reasoning for this was that since they
had no one to help them with any of the tasks that are
provided in AAL technology, the technology would
be the assistance commonly expected of relatives.
“Especially when I imagine living alone, I
would probably perceive this as an extreme
relief” [P6]
Lastly, one participant also said that it depended
on his health status. He perceived it less of a choice
but more of a medical necessity, i.e. if he is healthy,
he wouldn’t try it as there is no need for it. However,
if he was sick and had to be cared for and there was
no medical personnel or family members to help, it
would be irrelevant as to whether he trusted the
technology because there would not be another
option.
“Even at the risk of this thing making
mistakes, because I myself couldn’t do it at all.
I would make mistakes in any case. [...] So, it
would always be worse without that
machine.“ [P3]
In line with part of this argument, more
participants mentioned that if they did have the ability
to manage without these systems, they would always
try to avoid having to use them. This suggests that
AAL technology is associated with a decline in health
status as they most often used examples of advanced
scenarios in disease management, e.g., having severe
dementia or being physically bed-bound.
Figure 1: Illustration of Categories.
Exploring Trust Perceptions in the Medical Context: A Qualitative Approach to Outlining Determinants of Trust in AAL Technology
249

5 DISCUSSION
This paper set out to investigate perceptions of trust
in a general and medical context, narrowing in on
trust in medical AAL technology. The first aim was
to explore why and under which conditions people
trust the medical system. The second aim was to
explore how and under which conditions people trust
medical AAL technology. As the nature of this study
was exploratory, there were no expectations about the
outcomes. Based on previous literature searches,
three categories of trust influences could be outlined,
namely technology factors, user factors, and context
factors (Xu et al., 2014; Bova et al., 2006). The results
of this study suggest that these categories also fit the
answers given by the participants.
5.1 Trust Issues for the User Factors
In the category User Factors, participants mentioned
that trust is generally associated with time and
experience, meaning that that while there is a basic
level of trust, only time and experience will
strengthen this feeling sustainably. Moreover,
participants also felt that honesty and credibility were
important for trusting someone. This is shown by
words, but also with actions that signal integrity and
commitment to the relationship. Lastly, most of the
participants agreed that a serious betrayal of trust
would either result in the termination of the
relationship or could not be fully restored. On the
other hand, others mentioned that, while it is a long
process, trust could be regained over time and with
continuous action that both parties want to reconnect.
Ultimately, this category revealed the importance of
consistent behaviour in the formation of trust and in
the maintenance of it. This suggests a predisposition
of trust but also shows that for the majority of people,
time and trusting behaviour is a key component.
Relating these results back to existing literature, there
is congruency between past studies and this one,
namely that there are specific influences of user
characteristics which alter the overall acceptance of
these technologies (Wilkowska & Zielfe, 2018; Xu et
al., 2014).
5.2 Trust Issues for the Technology
Factors
In the category Technology Factors, answers closely
overlapped with the aspects mentioned for general
trust. Participants felt that AAL technologies should
have the same qualities as humans, i.e. knowledge or
correct results, honesty and integrity, and
benevolence. While the reactions were mostly
enthusiastic, some participants were also concerned
about their data being stored, although this was
strongly related to who had access to it. Moreover,
other concerns were with regard to the lack of
empathy and warmth provided by the technology and
the error rate, i.e. to which extent the technology
gives incorrect data and alarms. Overall, participants
agreed that the technology should not be a
replacement of health care workers but an
enhancement for them. The aspects that were
mentioned in this category are in line with literature
on medical technology, but also with other contexts,
such as autonomous driving, E-commerce, and
internet application, e.g., Facebook & Excel
(McKnight, 2011; McKnight & Chervany, 2014;
McKnight and Chervany, 2001; Montague et al.,
2009, Hengstler et al., 2016).
5.3 Trust Issues for the Context Factors
In the category Context Factors, the results outline
the dependent relationships of trust within the
medical system and the participant’s social context.
Most participants mentioned an emotional
component related to the treating physician, i.e., that
they felt taken seriously and that the physician paid
attention to their concerns. Moreover, they looked for
expertise and knowledge when confiding in health
care workers. The most common line of reasoning
was that they did not have the training themselves and
were obliged to believe a professional. In line with
this, the results suggest that if they trusted their
primary care worker, they would be more open to
trying new technology. This was under the condition
that the person introducing it to them was also skilled
at using and explaining it, and the participants were
informed about data handling. With regard to living
arrangements, it became clear that there was a higher
acceptance and more enthusiasm about AAL
technology if they either lived alone or if it relieved
burden of care on their family members and by
extension, health care workers. Conversely, most of
them did not believe AAL technology could provide
the same quality of medical care than human medical
care. Within the literature, there are studies validating
some of the aspects, i.e. experience of the physician,
information about the technology and perception of
how health care worker use the technology (Bova et
al., 2006; Qiao et al., 2015). In this study however,
there was a proportionally bigger association of
human care and AAL technology than in other
existing studies that could be found. This implies a
strong moderation of context factors on trust in
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
250

medical technology. Moreover, other studies have
also found an association of living situation and social
support on the acceptance and trust of medical
technology, signalling coherence with findings of this
study (Offermann-van Heek et al., 2019; Jaschinski &
Allouch, 2017).
5.4 Strengths and Limitations
This study was exploratory in nature which can
considered a strength since it set out to capture
unbiased opinions and concerns of trust in the
medical context. It was structured from very general
questions to specific scenarios, enabling the
participants to freely associate. Moreover, the sample
was relatively balanced, with four people of younger
age, four people of middle age, and three people of
advanced age. Six of the eleven participants were
female, and there were six people with care
experience, either personally or due to their
profession. Lastly, the results were in line with
previous research, suggesting that the approach was
appropriate for this research question. As with every
study, there are also limitations to consider. Firstly,
the sample was entirely German, limiting the
generalisability with regard to cultural implications.
Secondly, while the exploratory approach has its
advantages, there are downsides to it as well. Because
of the generic approach, many important feelings and
thoughts might not have been captured and could be
explored more precisely in future studies. Moreover,
the features of AAL technologies were described
superficially which might have made it difficult for
participants to imagine a specific, tangible camera or
sensor. Some of the participants also mentioned that
they could not imagine a specific technology
performing these actions and mostly referred to
devices that they have had contact with, e.g., fitness
tracker and emergency wrist bands. Ideally,
participants can physically try out AAL technology
for them to have a more realistic and less scenario-
based experience.
6 IMPLICATIONS: RESEARCH
AND APPLICATION
Given the results of this study, the next step is to
operationalise the aspects and concerns into a scale
with the goal of quantifying them. While the
qualitative approach is useful for an idiographic view
on perceptions of trust, it is necessary to strengthen
the validity of the results and expand their
generalisability with a systematic, quantitative
approach. On the basis of these results, future studies
might focus on specific variables and their individual
influence on trust development in the context of AAL
technologies. As the results revealed three major
categories, future studies can direct their focus on
each of these individually and in due time, address
them in a network of all relevant factors. With the
ultimate goal of mapping trust in the health care
context, this study served as a first step for outlining
idiographic factors and concerns by potential users.
Consequentially, these have to be considered in a
quantitative context with clearly defined parameters.
This will build the foundation to investigate trust
from a psychometric perspective and ultimately, each
influence could be integrated into a model of trust in
health care contexts and AAL technology, for other
researchers to disseminate and corroborate. Finally,
future research could benefit from experimental
studies that look at trust not only from a correlational
or even scenario-based perspective but can
investigate causal mechanisms of important variables
in the health care and AAL context. Moreover, as the
concept of trust in the medical system and medical
technology is of relevance in all cultural settings, the
socio-cultural influences could be explored by
investigating the research aims in different countries.
7 CONCLUSIONS
In line with previous research, this study has shown
that trust is a multi-factor concept embedded in a
network of variables that interact with each other.
This has implications for professionals in various
areas of expertise. However, more research,
specifically with a larger sample, is needed to validate
and corroborate these preliminary findings. This
study has implications for not only researchers in the
field, but also clinicians, policy makers and
developers of medical technology. Trust is not one
variable influencing another but is embedded in a
network of mediators and moderators, most
prominently physicians and care personnel but also
independent institutes and health insurance
companies. In addition, developers can make use of
specific user requirements, such as data handling and
specifically error rates and accuracy measures, when
conceptualising AAL technology and specifically
training of clinicians and health care workers that are
the first to introduce medical AAL technology to
(future) users. Developers could also incorporate the
technological requirements of the users in the design
of AAL technology, such as perfecting the error rate
Exploring Trust Perceptions in the Medical Context: A Qualitative Approach to Outlining Determinants of Trust in AAL Technology
251

and optimising the user interface. On a higher level,
policy makers and legal professionals might benefit
from incorporating general protocols that respect the
users’ need of feeling heard and being informed. This
could be implemented in specific training for health
care workers which in turn, might increase trust of the
users in their treating care personnel.
ACKNOWLEDGEMENTS
The authors thank all participants for their
participation and willingness to share their
experiences. This project has received funding from
the European Union’s Horizon 2020 research and
innovation programme under the Marie Skłodowska-
Curie grant agreement No 861091. The researchers
also thank Alexander Hick, Caterina Maidhof, and
Julia Offermann for research support.
REFERENCES
Bova, C., Fennie, K. P., Watrous, E., Dieckhaus, K., &
Williams, A. B. (2006). The health care relationship
(HCR) trust scale: Development and psychometric
evaluation. Research in Nursing & Health, 29(5), 477-
488. https://doi.org/10.1002/nur.20158
Climent-Perez, P., Spinsante, S., Mihailidis, A., & Florez-
Revuelta, F. (2020). A review on video-based active
and assisted living technologies for automated
lifelogging. Expert Systems with Applications, 139.
https://doi.org/10.1016/j.eswa.2019.112847
De Ruyter, B. D., & Pelgrim, E. (2007). Ambient assisted-
living research in carelab. Interactions, 14(4), 30-33.
doi: 10.1145/1273961.1273981
Jaschinski, C., & Allouch, S. B. (2017). Voices and views
of informal caregivers: Investigating ambient assisted
living technologies. Ambient Intelligence, 110. 110-
123. https://doi.org/10.1007/978-3-319-56997-0_8
Hengstler, M., Enkel, E., & Duelli, S. (2016). Applied
artificial intelligence and trust - The case of autonomous
vehicles and medical assistance devices. Technological
Forecasting and Social Change, 105, 105-120.
https://doi.org/10.1016/j.techfore.2015.12.0 14
Himmel, S., & Ziefle, M. (2016). Smart home medical
technologies: Users’ requirements for conditional
acceptance. I-com, 15(1), 39-50. https://doi.org/10.15
15/icom-2016-0007
Jaschinski, C., & Allouch, S. B. (2015). An extended view
on benefits and barriers of ambient assisted living
solutions. International Journal on Advances in Life
Sciences 7(1-2). 40-53.
Mayer, R. C., Davis, J. H., & Schoorman, F. D. (1995). An
integrative model of organizational trust. Academy of
Management Review, 20(3), 709-734.
https://doi.org/10.5465/amr.1995.9508080335
McKnight, D. H., Carter, M., Thatcher, J. B., & Clay, P. F.
(2011). Trust in a specific technology: An investigation
of its components and measures. ACM Transactions on
management information systems, 2(2), 1-25.
https://doi.org/10.1145/1985347.1985353
McKnight, D. H., & Chervany, N. L. (2001). What trust
means in e-commerce customer relationships: An
interdisciplinary conceptual typology. International
Journal of Electronic Commerce, 6(2), 35-59.
https://doi.org/10.1080/10864415.2001.11044235
Memon, M., Wagner, S. R., Pedersen, C. F., Beevi, F. H.
A., & Hansen, F. O. (2014). Ambient assisted living
healthcare frameworks, platforms, standards, and
quality attributes. Sensors, 14(3), 4312-4341.
https://doi.org/10.3390/s140304312
Michel, J. P., & Ecarnot, F. (2020). The shortage of skilled
workers in Europe: Its impact on geriatric medicine.
European Geriatric Medicine, 11(3), 345-347.
https://doi.org/10.1007/s41999-020-00323-0
Montague, E. N., Kleiner, B. M., & Winchester III, W. W.
(2009). Empirically understanding trust in medical
technology. International Journal of Industrial
Ergonomics, 39(4), 628-634. https://doi.org/10.1016/
j.ergon.2009.01.004
Offermann-van Heek, J., Schomakers, E. M., & Ziefle, M.
(2019). Bare necessities? How the need for care
modulates the acceptance of ambient assisted living
technologies. International journal of medical
informatics, 127, 147-156. https://doi.org/10.1016/
j.ijmedinf.2019.04.025
Offermann-van Heek, J., & Ziefle, M. (2019). Nothing else
matters! Trade-offs between perceived benefits and
barriers of AAL technology usage. Frontiers in Public
Health, 7, 134. https://doi.org/10.3389/fpubh.2019.00
134
Peek, S. T. M., Wouters, E. J. M., van Hoof, J., Luijkx, K.
G., Boeije, H. R., & Vrijhoef, H. J. M. (2014). Factors
influencing acceptance of technology for aging in
place: A systematic review. International Journal of
Medical Informatics, 83(4), 235–248. https://doi.org/
10.1016/j.ijmedinf.2014.01.004
Qiao, Y., Asan, O., & Montague, E. (2015). Factors
associated with patient trust in electronic health records
used in primary care settings. Health Policy and
Technology, 4(4), 357-363. https://doi.org/10.1016/
j.hlpt.2015.08.001
Schomakers, E. M., Biermann, H., & Ziefle, M. (2021).
Users’ Preferences for Smart Home Automation–
Investigating Aspects of Privacy and Trust. Telematics
and Informatics, 64, 101689.
Steinke, F., Fritsch, T., Brem, D., & Simonsen, S. (2012).
Requirement of AAL systems: Older persons' trust in
sensors and characteristics of AAL technologies. In
Proceedings of the 5th International Conference on
Pervasive Technologies Related to Assistive
Environments (pp. 1-6). https://doi.org/10.1145/2413
097.2413116
VERBI Software. (2017). MAXQDA 2018 [computer
software]. Berlin, Germany: VERBI Software.
Available from maxqda.com.
ICT4AWE 2022 - 8th International Conference on Information and Communication Technologies for Ageing Well and e-Health
252

Wichert, R., Furfari, F., Kung, A., Tazari, M. R. (2012):
How to overcome the market entrance barrier and
achieve the market breakthrough in AAL. In: Wichert
R., Eberhardt B. (eds) Ambient Assisted Living.
Advanced Technologies and Societal Change. Springer,
Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-
27491-6_25
Wilkowska, W., Offermann-van Heek, J., Florez-Revuelta,
F., & Ziefle, M. (2021). Video cameras for lifelogging
at home: Preferred visualization modes, acceptance,
and privacy perceptions among german and turkish
participants. International Journal of Human–
Computer Interaction 37(15), 1436-1454.
https://doi.org/10.1080/10447318.2021.1888487
Wilkowska, W., & Ziefle, M. (2018). Understanding trust
in medical technologies. 4th International Conference
on Information and Communication Technologies for
Ageing Well and E- Health. SCITEPRESS. (pp. 62-73).
World Health Organization. (2002). Active ageing: A policy
framework (No.WHO/NMH/NPH/02.8). World Health
Organization.
Xu, J., Le, K., Deitermann, A., & Montague, E. (2014).
How different types of users develop trust in
technology: A qualitative analysis of the antecedents of
active and passive user trust in a shared technology.
Applied Ergonomics, 45(6), 1495-1503.
https://doi.org/10.1016/j.apergo.2014.04.012
Ziefle, M. (2021). Ambient Assisted Living. In
Telemedizin (pp. 451-466). In: Marx G., Rossaint R.,
Marx N., (eds) Springer, Berlin, Heidelberg.
https://doi.org/10.1007/978-3-66260611-7_40
Ziefle, M., & Valdez, A. C. (2017). Domestic robots for
homecare: A technology acceptance perspective.
In International Conference on Human Aspects of IT
for the Aged Population(pp. 57-74). Springer, Cham.
Exploring Trust Perceptions in the Medical Context: A Qualitative Approach to Outlining Determinants of Trust in AAL Technology
253
