
Managing the Process Conglomeration in Health and Social Care
Monica Winge, Paul Johannesson, Erik Perjons and Benkt Wangler
Department of Computer and Systems Sciences, Stockholm University, Forum, SE-164 40, Kista, Sweden
Keywords: Process Conglomeration, Patient Care Process, Coordination Theory, Speech Act Theory, Information
Services.
Abstract: The organisation and processes of today’s health and social care are becoming ever more complex as a
consequence of societal trends, including an ageing population and an increased reliance on care at home.
One aspect of the increased complexity is that a single patient may receive care from several separate care
providers, which easily results in situations with potentially incoherent, uncoordinated and interfering care
processes. In order to describe and analyse such situations, the paper introduces the notion of a process
conglomeration. This is defined as a set of patient care processes that all influence the same patient, which
are overlapping in time, and that all have the goal of improving or maintaining the health and social
wellbeing of the patient. Problems and challenges of process conglomerations are investigated using
coordination theory and speech act theory. In order to address the challenges, a number of information
services are proposed.
1 INTRODUCTION
Today’s health and social care systems face a
number of challenging trends that contribute to their
increased complexity. One trend is that the
population in developed countries is ageing meaning
that more and more people are suffering from
multiple diseases. Many patients are being cared for
in their homes due to both individual preferences
and needs for cost containment. This adds to
complexity as health and social care at home
typically requires that many care providers with
different specialities are involved, private as well as
public ones. Not only health care is required but also
social care with assistance for daily living.
Furthermore, informal care parties like family
members and neighbours also get a more prominent
role for support and mediation.
In this complex and patient centered care
environment, multiple care parties are hence
engaged in concurrent and asynchronous processes
for assisting, investigating and treating a patient. The
complex environment results in situations where
care is provided through an aggregation of
potentially incoherent, uncoordinated and interfering
processes. In order to represent and analyse these
emergent aggregations of processes, we introduce
the notion of a process conglomeration that consists
of separate and more or less independent care
processes. In a process conglomeration, the patient
may experience problems like several care parties
visiting at the same time, different care parties
prescribing conflicting treatments, or care parties
neglecting their responsibilities.
Most work on business process management in
health care has focused on improving organisational
performance, medical effectiveness, knowledge
exchange and information system integration (e.g.,
Lenz and Reichert, 2007; Walburg, 2006; Beveren,
2003). However, to the best of our knowledge, the
research literature has as yet not paid any attention
to the problems that arise when several similar,
interdependent and concurrently ongoing business
processes are entangled in what we here refer to as a
process conglomeration.
In order to overcome the problems and
challenges of process conglomerations, multiple
complementing solutions are needed. Some
solutions aim at improving organisational structures
and processes, while others focus on attitudes and
behaviours among personnel. There are also
solutions that address reimbursement models and
incentive structures. In this paper, we focus on
information and communication solutions that
enable multiple care parties and patients to
coordinate their activities. A main goal of the paper
374
Winge M., Johannesson P., Perjons E. and Wangler B..
Managing the Process Conglomeration in Health and Social Care.
DOI: 10.5220/0004248903740381
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 374-381
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

is to propose a set of information services that, in the
context of process conglomerations, can facilitate
effective and seamless communication between
health care parties.
2 THEORETICAL BASIS
2.1 Language Action Perspective
A common view on business processes is that they
transform inputs into outputs. The activities of a
process are seen as contributing to more value for a
customer as inputs are successively refined into
outputs. However, as noted by Goldkuhl and Lind
(2008), this view may be too restrictive as it
disregards the coordinative aspects of business
processes. From a coordination perspective, a
business process focuses not on value
transformations but on communicative acts like
requests, offers, counteroffers, commitments,
agreements, acknowledgments, etc. The theoretical
foundations of this view come primarily from speech
act theory, (Searle, 1970). A basic idea in speech act
theory is that people carry out social activities (also
called speech acts) that, if properly combined and
executed, result in social relationships. For example,
a request (social activity) followed by a commitment
(social activity) will result in a contract (social
relationship) between two actors.
One influential approach to a communicative
view on business processes is the action workflow
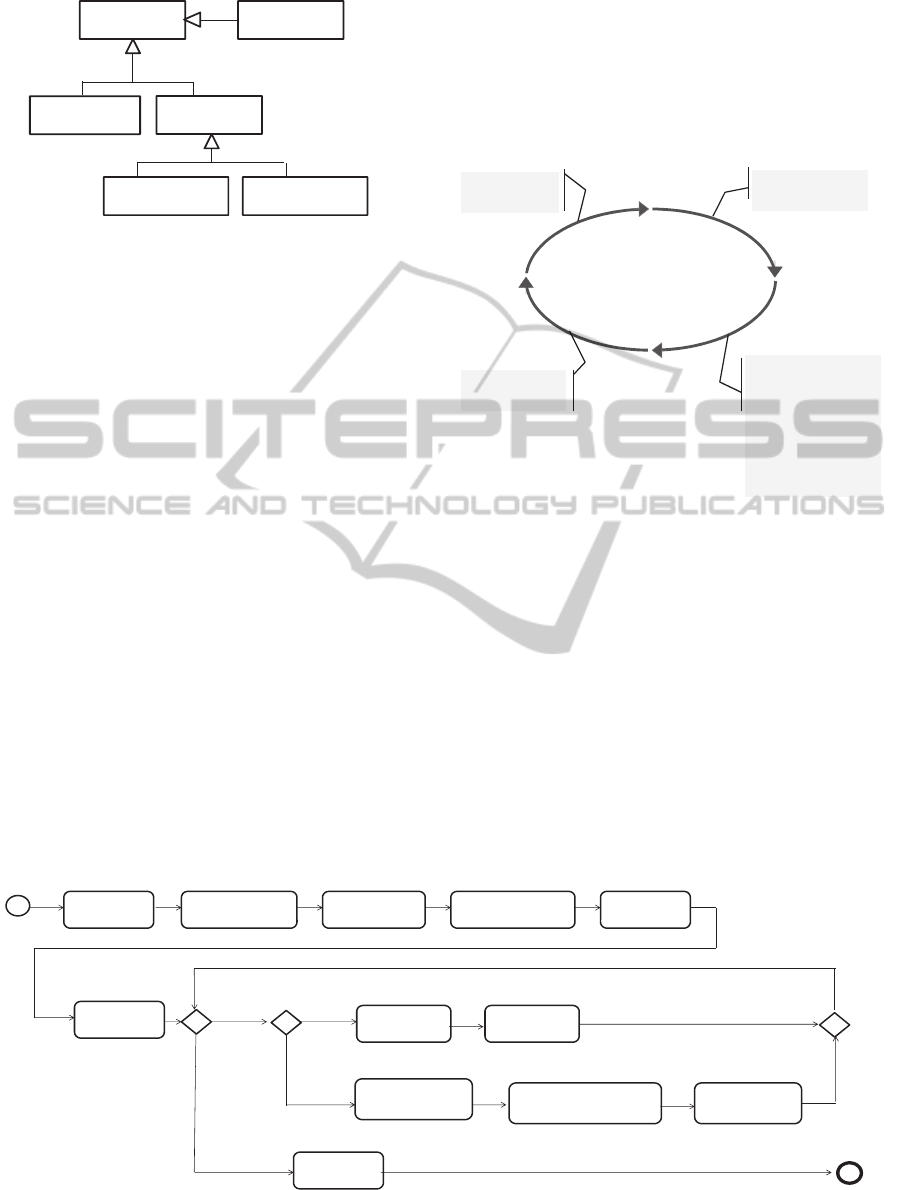
loop (Winograd and Flores, 1987), see Figure 1. The
loop consists of four parts:
Request. One party requests another party to
carry out some activity.
Commitment. After an optional negotiation, the
party who received a request for an activity may
commit to carry it out. This results in an
agreement, a social relationship, between the
two parties that one of them is to carry out an
activity for the benefit of the other.
Execution. The party who committed to carry
out an activity actually executes it.
Acknowledgement. The requesting party
acknowledges the execution of the activity and
confirms that she is satisfied with it.
2.2 Coordination Theory
In order to work smoothly, processes need to be
coordinated. Malone and Crowston (1990) suggest
the following definition of coordination: “the act of
Request
Commitment
ExecutionAcknowledgement
Figure 1: The action workflow loop.
managing interdependencies between activities
performed to achieve a goal”. Such dependencies
may give rise to conflicts and need to be detected
and resolved. There are three main kinds of activity
dependencies:
Flow Dependencies. A flow dependency
between two activities occurs when one of the
activities needs to be carried out before the
other one, often because the first activity
produces some resource required by the other
one.
Share Dependencies. A share dependency
occurs when two activities try to get exclusive
access to the same resource at the same time.
An example is that two physicians want to use
the same X-ray machine at the same time, or
simply that two actors need to get access to a
patient at the same time.
Fit Dependencies. A fit dependency occurs
when two activities modify the same resource
and need to ensure that the modifications are
consistent and coherent, taking into account the
overall needs and constraints of the resource.
An example is that a patient is given two drugs
that interfere with each other.
3 THE PROCESS
CONGLOMERATION
CHALLENGE
This section introduces the notion of process
conglomerations as well as the challenges they give
rise to. Before addressing these issues we introduce
some basic concepts for the actors involved in health
care, see Figure 2. These concepts are based on
(CONTSYS, 2007) and (Gustafsson and Winge,
2003).
A health/social care party (sometimes
abbreviated care party) is a person or organisation
that is involved in health/social care. There are three
kinds of care parties: health/social care provider,
health/social care third party, and patient. A
health/social care provider (sometimes abbreviated
ManagingtheProcessConglomerationinHealthandSocialCare
375
Health/social
care provider
Health/social
care party
Health/socialcare
organisation
Health/socialcare
professional
Health/social
care third party
Patient
Figure 2: Basic concepts for actors involved in health care.
care provider) is a person or organisation that
provides health/social care. A health/social care
third party (sometimes abbreviated carer) is a
person or organisation that supports care services
and is not a professional health/social care party. An
example could be a relative to a patient that
performs some or all care activities needed for
taking care of the patient. A patient is a care party
that receives or can receive health/social care.
Finally, a care provider can be of two kinds:
health/social care organisation and health/social care
professional. A health/social care organisation
(sometimes abbreviated care organisation) is a
private or public organisation that provides care as
its main service, while a health/social care
professional is a person that in her professional role
provides care.
The work carried out by one care provider for
one patient can be described as an action workflow
loop, see Figure 3, which we refer to as the Patient
Care Process. It contains the following activities:
Request. A care provider receives a request
from a care party to address a health/social
problem for a patient.
Negotiation. The care provider commits to
address the care request.
Execution. The care provider together with the
patient set up a plan including a set of goals and
activities that aims to improve the patient’s
health/social situation. The care provider then
performs the planned activities.
Acknowledgment. Finally, the requester
evaluates goal fulfilment.
Request
Commitment
ExecutionAcknowledgement
• Receive care
request
• Confirm care
commitment
• Determine
health/social
problem
• Decide care goals
• Specify care plan
• Performcare
activities
• Evaluate goal
fulfillments
Figure 3: The patient care process described as a workflow
loop.
While Figure 3 provides an overview of the Patient
Care Process, Figure 4 describes it in greater detail.
This model is based on the patient care processes
described in SAMBA (Samba, 2004) and SAMS
(Winge, 2007), though adapted for the purpose of
addressing process conglomerations.
The detailed Patient Care Process (described in
Figure 4) contains the following activities:
Request. The Patient Care Process starts when a
care provider receives a care request from a
care party.
Negotiation. The receiving care provider checks
Receive
care request
Confirm
care commitment
Specify care
plan
Evaluate goal
fulfillments
Send care request
foractivity
Receive care
commitment foractivity
Isthere an
activityin
theplan
thatisstill
left tobe
carried out ?
Yes
Receive activity
completion
No
Isthe
activity
decided to
becarried
out inthe
organisa‐
tion?
Yes
No
Schedule
activity
Perform
activity
Identify health/
socialstatus
Determine health/
socialproblem
Decide care
goals
Figure 4: The Patient Care Process described in more detail.
HEALTHINF2013-InternationalConferenceonHealthInformatics
376
that it is able to take responsibility for the care
request. If so, it confirms a care commitment.
Execution - planning level. The responsible care
provider identifies the patient’s health/social
status, i.e., anamnesis, symptoms and earlier
treatments, and determines the patient’s
health/social problems. Thereafter, a care plan
is to be specified. This can often be done by the
responsible care provider and the patient
themselves, but it sometimes requires a planning
conference, in which several care parties
participate.
Execution - performance level. Each activity in
the care plan needs to be performed by either
the responsible care provider or another actor. If
the activity is performed by the responsible care
provider, it will both schedule the activity and
then perform the activity. If the activity is to be
performed by another actor, a care request is
sent to this actor asking it to be responsible for
the activity.
Acknowledgment. Finally, when all the activities
in the care plan have been carried out, the
responsible care provider evaluates the goal
fulfillment of the care plan. This includes an
acknowledgement from the original requester
that the care plan has been executed as well as a
confirmation or refutation that the patient’s
health/social situation has been improved.
A patient is often involved in several processes, as a
patient care process can be nested within another as
a consequence of a care provider outsourcing some
activities. In addition to several processes being
nested due to activities being outsourced from one
care provider to another, a patient can also be
subject to a number of more or less independent care
processes, each conducted by separate care parties.
The reason may be that the patient suffers from and
is treated for multiple health/social problems.
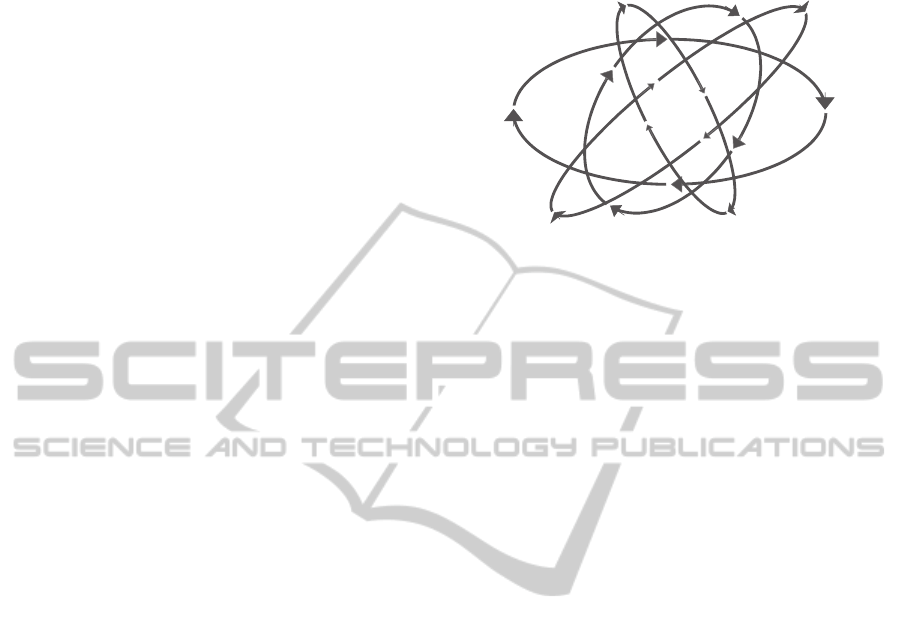
A set of independent care processes around a
patient will form a process conglomeration, see
Figure 5, which includes activities that are
potentially incoherent, uncoordinated and
interfering. More precisely, we define a process
conglomeration as a set of patient care processes
that all influence the same patient, which are
overlapping in time, and that all have the goal of
improving or maintaining the health and social
wellbeing of the patient.
Process conglomerations give rise to
coordination problems that go beyond those
encountered in single or nested patient care
processes. A key difference between single patient
care processes and conglomerations is that the
activity dependencies in a patient care process are
PATIENT
Figure 5: A process conglomeration, i.e., a set of
individual though interdependent care processes around a
patient.
planned and known beforehand, while those in a
conglomeration are emergent and may occur
unexpectedly for the involved care parties. While
each patient care process is internally coordinated in
the form of an action workflow loop with a clear
structure and distribution of responsibilities, there is
no corresponding coordination across the care
processes in a process conglomeration. Thus,
dependencies between activities from different
patient care processes may easily be neglected,
which may cause worries and inconveniences for the
patient as well as ineffective and inefficient care.
Furthermore, as many parties are involved in a
process conglomeration, responsibility issues may
arise.
As a process conglomeration can be highly
complex, problems can easily occur if it is not
adequately managed. Based on coordination theory
and previous work in Gustafsson and Winge (2003)
and Centrum för e-Hälsa (2007), we have identified
four main categories of problems in a process
conglomeration.
Share Negligence. Two or more care parties try
to provide care to a patient at the same time. In
other words, the parties try to carry out activities
between which there exists a share dependency.
For example, a patient may be busy with her
physiotherapist when a nurse shows up to
plaster a leg ulcer.
Flow Negligence. Two care parties carry out
activities in the wrong order. In other words,
there is a flow dependency between activities
that is not respected by the care parties. For
example, a nurse first plasters the leg ulcer of a
patient, and thereafter the home care personnel
give the patient a shower, while these activities
ought to be carried out in the opposite order.
ManagingtheProcessConglomerationinHealthandSocialCare
377

Fit Negligence. Two activities are carried out
though they may conflict with each other. In
other words, there is a fit dependency between
activities that is not respected. For example, a
patient is given a therapy by a physiotherapist
that is not suitable for a certain medical
treatment given by a nurse from primary care.
Responsibility Negligence. A health care party
who is responsible for a task does not carry it
out or carries it out in an unsatisfactory way.
For example, a nurse may not distribute
prescribed medication to a patient, though this is
her responsibility.
The underlying causes to these problems may vary,
including deficiencies in organisational structures
and gaps in personnel competence. However, in a
process conglomeration, a main cause for the
problems is lack of information, knowledge and
common views due to inadequate communication.
Based on the activities of the Patient Care Process as
well as previous work by Gustafsson and Winge
(2003), we have identified four categories of
knowledge deficiencies that cause problems in
process conglomerations.
Lack of knowledge about the health/social
problems and health/social status of patients
Lack of knowledge about performed, ongoing
and planned activities as well as activity
dependencies and changes in plans
Lack of knowledge and consensus on care goals
and their priorities
Lack of clearly allocated responsibilities and
knowledge about them.
4 SOLUTION REQUIREMENTS
The information and communication problems of
process conglomerations can be addressed by
providing care parties with information services that
support them in exchanging information, building
consensus and distributing responsibilities. This
section identifies a number of requirements that
these services need to fulfil in order to effectively
address the problems. The requirements below are
structured according to the problem causes they
address.
Lack of knowledge about the health/social problems
and health/social status of patients
R1: Care providers shall be able to exchange their
assessments on the health/social problems of a
patient
R2: Care providers shall receive support for
detecting, discussing and negotiating differences in
their assessments of the health/social problems of
patient
R3: Care parties shall be able to communicate about
the health/social status of a patient
Lack of knowledge about performed, ongoing and
planned activities as well as activity dependencies
and changes in plans
R4: Care parties shall be able to communicate about
care activities planned to be carried out
R5: Care parties shall be able to request care from
other care parties as well as commit to carry out care
R6: Care parties shall be able to communicate
ongoing and completed care activities
R7: Care parties shall be able to communicate about
the results of care activities
R8: Care parties shall receive support for detecting
and managing activity dependencies
Lack of knowledge and consensus on care goals and
their priorities
R9: Care parties shall be able to communicate about
the goals for activities carried out by care providers
R10: Care parties shall receive support for detecting
and managing care goal conflicts
Lack of clearly allocated responsibilities and
knowledge about them
R11: Care parties shall be able to communicate
about the responsibilities of care providers
R12: Care parties shall receive support for detecting
and managing responsibility negligence
As can be seen from the above requirements, the
information services need to handle complex
information structures. A first step towards defining
the services is, therefore, to construct an information
model that can represent all the information needed
by the services.
5 SOLUTION - INFORMATION
MODEL AND INFORMATION
SERVICES
A solution to the process conglomeration challenge
is suggested in this section in the form of a number
of information services, see Section 5.2. First, in
HEALTHINF2013-InternationalConferenceonHealthInformatics
378
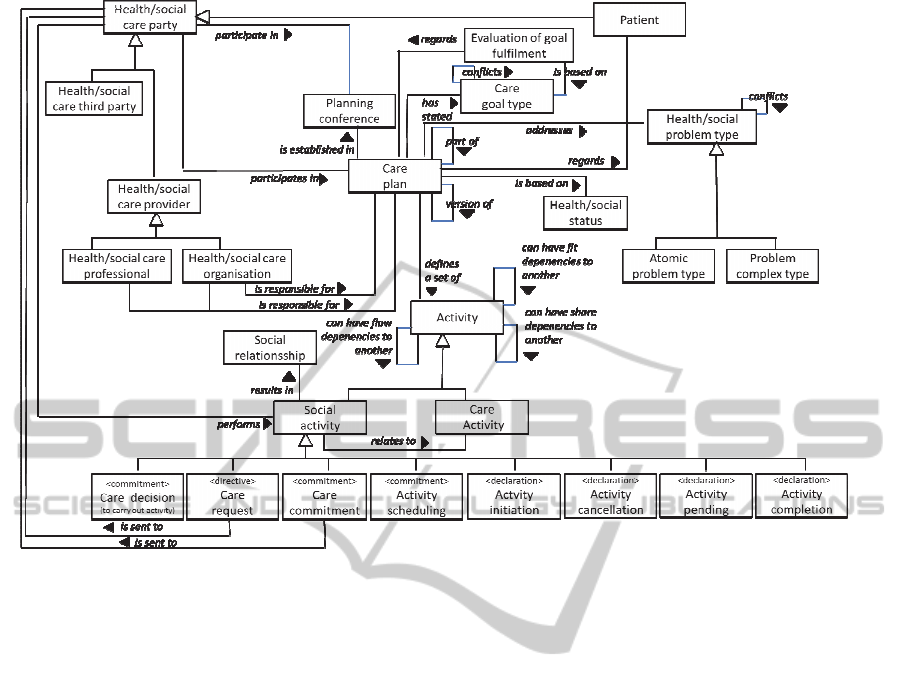
Figure 6: An information model that represents all the information needed by the services.
section 5.1, an underlying information model is
presented, which can represent all the information
needed by the services.
5.1 Information Model
The proposed information model, which is based on
(CONTSYS, 2007) and (Gustafsson and Winge,
2004), is described below and shown as a UML
class diagram in Figure 6. The first group of
requirements in Section 4 demands that the
information services be able to manage information
about the health/social problems and health/social
status of patients. To handle this, the information
model includes the classes health/social problem
type (sometimes abbreviated health problem) and
health/social status (sometimes abbreviated health
status). A health/social care problem type is a need
for care for a patient as defined by a care provider,
often expressed as a diagnosis. A health/social
problem type is either an atomic problem type or a
combination of problem types, called problem
complex type. The latter notion is useful as patients
often experience a number of related health/social
problems, which can be effectively addressed by the
same care plan. The information model also includes
the class health/social status, which contains a
description of a patient’s anamnesis, symptoms and
earlier treatments when a care plan is established.
The second group of requirements in Section 4
demands that the information services be able to
manage information about activities and activity
dependencies. To handle this, the information model
includes the class care plan. A care plan can be a
part of or a version of another care plan. To establish
the care plan, there is sometimes a need for a
planning conference, which can be carried out
synchronously or asynchronously as well as at a
central place or in a distributed way. To represent
activity dependencies, the information model
includes associations for flow dependency, fit
dependency and share dependency.
The third group of requirements demands that
the information services be able to manage
information on care goals. To handle this, the
information model includes the class care goal type,
which is a set of predefined goals. To represent goal
conflicts, the information model includes an
association called conflicts. Each plan has one or
several of these goals related to it. The information
model is also able to represent the evaluation of the
goal fulfillment of the plan, that is, the result of a
performed care plan.
The fourth group of requirements demands that
the information services be able to manage
information about responsibility allocation. A care
ManagingtheProcessConglomerationinHealthandSocialCare
379

activity is a clinical activity that aims to investigate
or treat a patient. Around a care activity, various
care parties take a number of decisions that can be
seen as driving the care activity forwards. For
example, one care party can decide that a certain
care activity is to be carried out, and another care
party can decide to actually carry it out.
In order to represent decisions about care
activities, we introduce a class social activity. A
social activity, as described in Section 2.1, is a
sequence of speech acts that results in one or several
social relationships. There exist a number of
subclasses to social activity:
A care decision is a decision taken by a care
professional that a certain care activity is to be
carried out.
A care request is a social activity where one
care party asks another care party to take on the
responsibility for a care activity.
A care commitment is a commitment by a care
party, who has received a care request and that
takes on the responsibility for the care activity.
An activity scheduling includes a commitment
by a care party to start carrying out a care
activity at a time point.
An activity initiation includes a declaration by a
care party that a care activity has started.
An activity cancellation includes a declaration
that a care activity has been aborted before
completion and that no further work is planned.
An activity pending includes a declaration that a
care activity has been aborted before completion
as well as a commitment that it is to be
restarted.
An activity completion includes a declaration
that a care activity has been completed as
intended.
5.2 Information Services
Five high level services are identified, based on the
activities of the patient care process, and for each of
these a number of sub-services. For each sub-
service, its relationship to the information model is
specified and the requirements (R) it addresses.
Identify Health/Social Status and Determine
Health/Social Problem
This service provides support for communicating
about care need assessments. The included sub-
services are:
● Create, read and update health/social status
and health/social problem (R1, R3)
● Notify about conflicting views of
health/social problem among care parties
(R2)
Decide Care Goals
This service provides support for communicating
about care goal creation. The included sub-services
are:
● Create, read and update care goals (R9)
● Notify about about conflicting views of
care goals among care parties (R10)
Specify Care Plan
This service provides support for communicating
and negotiating care planning. The included sub-
services are:
● Create, read and update care plans, care
activities, care decisions, care requests and
care commitments (R4, R5, R11)
● Notify about activity dependencies that
occur when creating new care decisions and
care plans (R8)
● Support resolution of conflicts due to
activity dependencies (R8)
● Check for outstanding care decisions, i.e.,
care decisions for which there are as yet no
care requests (R12)
● Check for outstanding care requests, i.e.,
care requests for which there are as yet no
care commitments (R12)
Schedule and Perform Care Activity
This service provides support for communicating
about and managing the performance of care
activities. The included sub-services are:
● Create, read and update activity initiations,
activity cancellations, activity pendings,
and activity completions (R6)
● Notify about activity dependencies that
occurred when care activities were initiated
or completed (R8)
● Check for outstanding activity schedulings,
i.e. activity schedulings for which there are
as yet no activity initiations (R12)
Care Evaluation
This service provides support for communicating
about care evaluation. The included sub-services are:
● Create, read and update evaluations of goal
fulfilment (R7)
6 CONCLUDING REMARKS
In this paper, we have investigated how care
activities and processes are organised in today’s
complex and patient centered health and social care
HEALTHINF2013-InternationalConferenceonHealthInformatics
380

landscape. The main theoretical contribution of the
paper is the introduction of the notion of process
conglomeration, which is used to capture the
emergent nature of health care provisioning in an
environment of independent care parties. The paper
also provides practical contributions through an
analysis of the challenges posed by process
conglomerations as well as solutions in the form of
information services.
The proposed information services are based on
the assumption that care activities offered by one
care provider can be structured according to the
patient care process, basically an action workflow
loop. The patient care process structures the internal
work of a care provider and its interactions with a
patient, thereby producing a large amount of
information. This constitutes the bulk of the
information needed by the proposed information
services. Thus, implementing the services does not
require extensive additional information
management for care providers that already use the
patient care process.
Our work has been carried out according to the
design science framework, which is also reflected by
the structure of the paper that follows the methods
proposed by Peffers et al. (2007). While this paper
focuses on problem analysis, requirements definition
and solution design, previous work has addressed
demonstration and evaluation of the services.
In future work, we will detail the contents of the
information services and integrate them into an
overarching systems and service architecture. We
will also continue our work on empirical validation
of this architecture.
REFERENCES
Beveren, J. Van, 2003. Does health care for knowledge
management? In Journal of Knowledge Management,
7 (1): 90 – 95.
Centrum för för eHälsa, 2007. IT-implementering i vård
och omsorg: Slutrapport 2007-12, Centrum för eHälsa
(in Swedish)
CONTSYS, 2007. Health Informatics – Systems of
concepts to support continuity of care. Part 1: Basic
Concepts, EN-13940-1:2007.
Goldkuhl, G., and Lind, M., 2008. Coordination and
transformation in business processes: towards an
integrated view. In Business Process Management
Journal, 14 (6): 761–777.
Gustafsson, M., and Winge, M., 2003. SamS-projektet:
Process- och begreppsmodellering – delrapport (in
Swedish).
Gustafsson M., Winge M., 2004. SAMS Konceptuell
Informationsmodell – delrapport (in Swedish).
Lenz, R., and Reichert, M., 2007. IT support for healthcare
processes - premises, challenges, perspectives. In Data
and Knowledge Engineering 61: 39-58.
Malone, T.W., and Crowston, K., 1990. What is
coordination theory and how can it help design
cooperative work systems? In Proceedings of the 1990
ACM conference on Computer-supported cooperative
work, New York, NY, USA, pp. 357–370.
Peffers, K., Tuunanen, T., Rothenberger, M.A., and,
Chatterjee, S., 2007. A Design Science Research
Methodology for Information Systems Research. In
Journal of Management Information Systems, 24(3):
45-78.
SAMBA, 2004. Structured Architecture for Medical
Business Activities. Available (2012-09-03) at:
http://www.contsys.net/documents/samba/samba_en_s
hort_1_3.pdf.
Searle, J.R., 1970. Speech Acts: An Essay in the
Philosophy of Language, Cambridge University Press
Walburg, J., 2006. The outcome quadrant. In Walburg, J.,
Bevan, H., Wilderspin, J., and Lemmens, K. (eds.)
Performance Management in Health Care. Improving
patient outcomes: an integrated approach, Routledge..
Winograd, T. and Flores, F., 1987. Understanding
Computers and Cognition: A New Foundation for
Design. Addison-Wesley Professional
Winge., M., Johansson, L.-Å., Gustafsson, M., Fors, U.,
Lind Waterworth, E., and Sarv-Strömberg, L., 2007.
Slutrapport MobiSams-projektet: Mobilt IT-stöd för
samverkan i vård och omsorg.
ManagingtheProcessConglomerationinHealthandSocialCare
381
