
Designing Spoken Dialogue Systems based on Doctor-Patient
Conversation in the Diagnosis Process
Tesfa Tegegne and Theo van der Weide
Institute for Computing and Information Science, Science Faculty, Radboud University, Nijmegen, Netherlands
{tesfa, tvdw}@cs.ru.nl
Keywords:
Doctor-Patient Interaction, Culture, Spoken Dialogue System.
Abstract:
The paper describes the use of doctor-patient interaction in order to design a spoken dialogue system. In
this paper we analyze doctor and patient information seeking and information provision behavior. In our
experiments we found a difference in information seeking and information provisioning behavior of doctors
and patients, although statistically not significant. We identify some important roles that can be used as a
springboard to design a spoken dialogue system. Finally, we conclude that analyzing face-to-face doctor-
patient interaction can serve as an effective starting point to design spoken medical dialogues.
1 INTRODUCTION
Speech is one of the most effective means of commu-
nication for humans. It plays a great role especially
in man-machine interactions. Speech is natural and
the vast majority of humans are already fluent in us-
ing it for interpersonal communication. In the last two
decades there have been a lot of advances in the appli-
cation of spoken dialogue systems in different areas:
academia, military, and telecom companies. A dia-
logue system is one of the promising applications of
speech recognition and natural language processing.
Spoken language interaction with computers has be-
come a practical possibility both in scientific as well
as in commercial terms.
Spoken dialogue systems can be viewed as an
advanced application of spoken language technol-
ogy. Spoken dialogue systems provide an inter-
face between the user and a computer based ap-
plication that permits spoken interaction with the
application relatively in a natural manner (McTear,
2002). Fraser 1997, cited by (McTear, 2002), de-
fines spoken dialogue system as ”computer systems
with which humans interact on turn-by-turn basis and
in which spoken natural language plays an important
role in the communication”. Spoken dialogue sys-
tems enable semi-literate and illiterate users to inter-
act with a complex application in a natural way using
speech. Current spoken dialogue or/and IVR (Inter-
active Voice Response) systems restrict users in what
way they can say and how they can say it. However,
users of speech-based dialogue systems often do not
know exactly what information they require or how to
obtain it- they require the support of the dialogue sys-
tem to determine their precise requirement (a system
directed dialogue). For this reason, it is essential that
the spoken dialogue system is be able to engage users
in the dialogue rather than simply respond to prede-
termined spoken commands.
The propelling factor of this study is the adoption
and application of speech technology and its impact
on the healthcare sector in developing countries where
a significant number of the population is illiterate or
semi-literate. In this paper we analyze the doctor-
patient conversation in order to find out if we can
emulate the methods and techniques used in the con-
versation to design medical spoken dialogue system
that can be accessed easily by non-educated or semi-
educated population with the objective of searching
health information remotely.
Nowadays, mobile becomes an appropriate
medium to minimize the burden of healthcare in de-
veloping countries. Several researchers, for exam-
ple (Black et al., 2009; Bickmore and Giorgino, 2006;
Foster, 2011), are engaged in mobile based applica-
tions such as mHealth, mLearning, mBanking, mA-
griculture etc. The expansion of the mobile network
and the increment of mobile phone users in Ethiopia
provide a fertile ground to adopt and implement mo-
bile based healthcare applications. Designing a med-
ical dialogue alike doctor-patient interaction is very
cumbersome, the advancement of speech recogni-
tion requires another level to fully understand human
speech. It requires at least to design and develop a
261
Tegegne T. and van der Weide T.
Designing Spoken Dialogue Systems based on Doctor-Patient Conversation in the Diagnosis Process.
DOI: 10.5220/0004776302610268
In Proceedings of the Third International Symposium on Business Modeling and Software Design (BMSD 2013), pages 261-268
ISBN: 978-989-8565-56-3
Copyright
c
2013 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

medical dialogue system resembling human-like con-
versation to reduce the error of speech recognition.
Our main motivation is to understand whether face-
to-face doctor-patient interaction plays a vital role in
designing human-like medical spoken dialogue sys-
tem for the healthcare domain in the case of Ethiopia
using Amharic language. To the best of our knowl-
edge this is the first study that not only analyzes the
doctor-patient conversation but also designs and mod-
els a medical dialogue system in the case of Ethiopia.
In this paper we address the following question: Is
it possible to design a spoken medical dialogue sys-
tem based on doctor-patient face-to-face conversation
in the diagnosis process? The paper is organized as
follows. The state of the art of medical dialogue sys-
tems is discussed in section 2. The analysis of the ex-
periment is presented in section 3. Section 4 explains
the proposed spoken dialogue system. Finally, section
5 concludes the paper and gives future directions.
2 SPOKEN DIALOGUE SYSTEMS
IN HEALTHCARE
The healthcare domain has gleaned the benefits of the
advancements of Information Communication Tech-
nology. During the last two decades, these interfaces
have been adopted as part of tele-medicine technolo-
gies (Bickmore et al., 2006; Bickmore and Giorgino,
2006), which enable the delivery of a variety of med-
ical services to sites that are at a long distance from
providers.
The ultimate goal of a dialogue system is to pro-
vide health information for stakeholders primarily us-
ing spoken dialogue. Such a system can be used
for a wide range of applications including: patients
self-treatment and management, disease remote mon-
itoring, diagnosis, health education etc. In line to
this Bickmore and Giorgino ((Bickmore et al., 2006))
say that automated dialogue systems are increas-
ingly being used in healthcare to provide informa-
tion, advice, counseling, disease monitoring, clinical
problem identification, as well as enhancing patient-
provider communication.
However, a dialogue system in the healthcare do-
main is not without challenges. Clinical practice or-
dains complicated guidelines, ontologies and proce-
dures. This makes the dialogue system more com-
plex and cumbersome to handle. Bickmore and
Giorgino also mention some of the challenges of spo-
ken medical dialogue system: criticality (emergency
cases), confidentiality (privacy such as HIV/AIDS
regimen etc.) and mixed initiatives (patient-centered
vs. system-centered). They point out that incorpo-
rating medical and behavioral ontologies and deep
knowledge of health communication strategies are
very important for further development of medical di-
alogue systems.
Bickmore and Giorgino argue that face-to-face
communication together with written instructions re-
mains one of the best methods for communicating
health information to patients with low literacy level.
They report that face-to-face consultation is effective
because providers can use verbal and nonverbal be-
havior, such as head nods, hand gesture, eye gaze
cues and facial displays to communicate factual in-
formation to patients, as well as to communicate em-
pathy and immediacy to elicit patient trust. Accord-
ing to Durling and Lumsden ((Durling and Lumsden,
2008)) a spoken dialogue takes half the time needed
to achieve the same task using keyboard and mouse,
regardless of the participant’s ability to correct their
input. By highlighting the business side of speech
recognition in healthcare, Parente et al., cited by Durl-
ing and Lumsden, show that, in their opinion, the
adoption of speech technology is worthwhile. The use
of speech recognition has, in fact, seen the most suc-
cessful adoption in the healthcare domain.
2.1 Diagnosis Systems
Diagnosis, according to Webster’s dictionary,is the
act or process of deciding the nature of disease or
a problem by examining symptoms. In the medical
domain, many diagnosis systems are proposed and
used such as decision support systems, agent based
systems, and intelligent systems (fuzzy logic, expert
system, neural networks and the like). Mobile diag-
nostic technology is a relatively new concept in tele-
medicine. As suggested by the term itself, it involves
two key characteristics: mobility and remote diagno-
sis (Celi et al., 2009). The aim of using mobile tech-
nologies for healthcare is to support the patients out-
side of the medical and/or home environment.
2.2 Doctor-Patient Face-to-Face
Interaction
The main goal of a doctor-patient conversation is a
focused gathering with a common goal pursued by
its participants. Typically, a patient visits a doctor
with the purpose to be relieved from feeling unwell
possibly caused by an illness; the doctor’s purpose
of the interaction with the patient also is to relieve
the patient. When both parties appear to fail to com-
prehend or understand each other’s goal, the interac-
tion may be dysfunctional. Studying and analyzing
the doctor-patient interaction helps to convey empa-
Third International Symposium on Business Modeling and Software Design
262

thy and obtain a trusted spoken dialogue system, es-
pecially when used by the semi-literate and illiterate
rural people. The analysis should help to design a
full-fledged medical dialogue system. As we pointed
out in the previous sections, the main idea here is not
to analyze the effectiveness and efficiency of the face-
to-face doctor-patient interaction but rather the impli-
cations towards designing and modeling ’human-like’
medical dialogue system.
A good interaction and a quality relationship be-
tween doctors and their patients is now widely rec-
ognized as a key factor in improving not only patient
satisfaction but also treatment outcomes across a wide
range of healthcare disciplines. The use of specific
doctor communication skills has been associated with
improved adherence regimens, improved psycholog-
ical outcomes, more detailed medical histories and
fewer malpractice suits, in addition to increase patient
satisfaction (Bickmore et al., 2005). Doctor’s listen-
ing behavior is a necessary ingredient for an interac-
tion in which patients are describing and expressing
themselves freely and openly (Nevile, 2006).
To test the doctor’s listening behavior, the rela-
tive frequency of each category of information seek-
ing and information giving behavior is calculated for
the doctor-patient interactions, representing the num-
ber of dialogue acts in any particular category as a
proportion of the total number of dialogue acts made
by the speaker. A relative frequency of medical topics
addressed in every interaction is calculated for all in-
teractions. The doctor as a facilitator of doctor-patient
interaction should demonstrate a high frequency of
supportive and encouraging behavior in the presence
or absence of patient desired behavior. Even though
a patient’s characteristics are very important to the
quality of interaction, the doctor’s facilitating behav-
ior is essential since it allows patients either to express
themselves or to repress (Nevile, 2006).
3 FINDING CULTURAL
DEPENDENCIES
Information seeking behavior includes seeking infor-
mation about medical topics. Direct, assertive and
embedded question types are posed by both parties.
On the other hand, information provisioning or in-
formation giving is providing a direct answer to a
question, elaborating the question by providing sup-
plementary information and deviating or changing the
topics of the interaction without prompting from the
interacting partner.
In this study we group the doctor-patient conver-
sation into two categories: information seeking be-
havior and information provisioning behavior. Infor-
mation seeking consists of utterances about informa-
tion gathering, checking and cueing. Information pro-
visioning contains utterances dealing with explana-
tion, confirmation, and giving instructions. Both in-
formation seeking and information provisioning are
analyzed against medical topics: illness, symptoms,
diagnosis, treatment, exam/test and history (medical
history) for both doctor and patient.
In the analysis we remove backchannels.
Backchannels contain, greetings, and acknowledg-
ment that carry little information value for healthcare
doctors and patients. Removing backchannels should
not affect the quality of information obtained from
the interaction. We use a two-way ANOVA (Analysis
of Variance) to see the difference between doctor
and patient in the two criteria and medical topics
or themes. Additionally, we check the number of
questions posed by doctors and patients. Finally, we
analyze the overall interaction process.
3.1 Methodology
The focus of this research is to design a spoken med-
ical dialogue system on the basis of doctor-patient
face-to-face interactions, to understand the weak and
strong side of the interaction and to utilize actions
taken place during the interaction. We have con-
ducted a number of observational studies in which we
recorded the interaction between patients and health
professionals. Based on these observations we de-
sign the content of the conversation including ques-
tion and declarative statements, the order of presen-
tation of content, how a system responds to ques-
tions and words, sentence structure and tone used, to
closely match the user expectations of what a health
professional might ask, respond and sound like. In-
depth interview studies show that this is perceived by
patients as a successful conversation (Migneault et al.,
2006).
The doctor-patient interactions are analyzed as
follows. We classify the elicitation process based on
semantic entities as shown in figure 1, leading to the
following topics: (i) Illness, (ii) Symptoms, (iii) Di-
agnosis, (iv) Previous Treatment, (v) Current Treat-
ment and (vi) Exam. Questions and Explanations
are targeted towards the following variables proposed
by (Nowak, 2011): (i) information, (ii) confirmation,
(iii) checking, (iv) explanation, (v) cue and (vi) giving
instruction.
First we address the efforts taken by both doc-
tor and patient to identify problems and attempting
to recommend. This includes the process of elicita-
tion (information gathering), explanation, confirma-
Designing Spoken Dialogue Systems based on Doctor-Patient Conversation in the Diagnosis Process
263
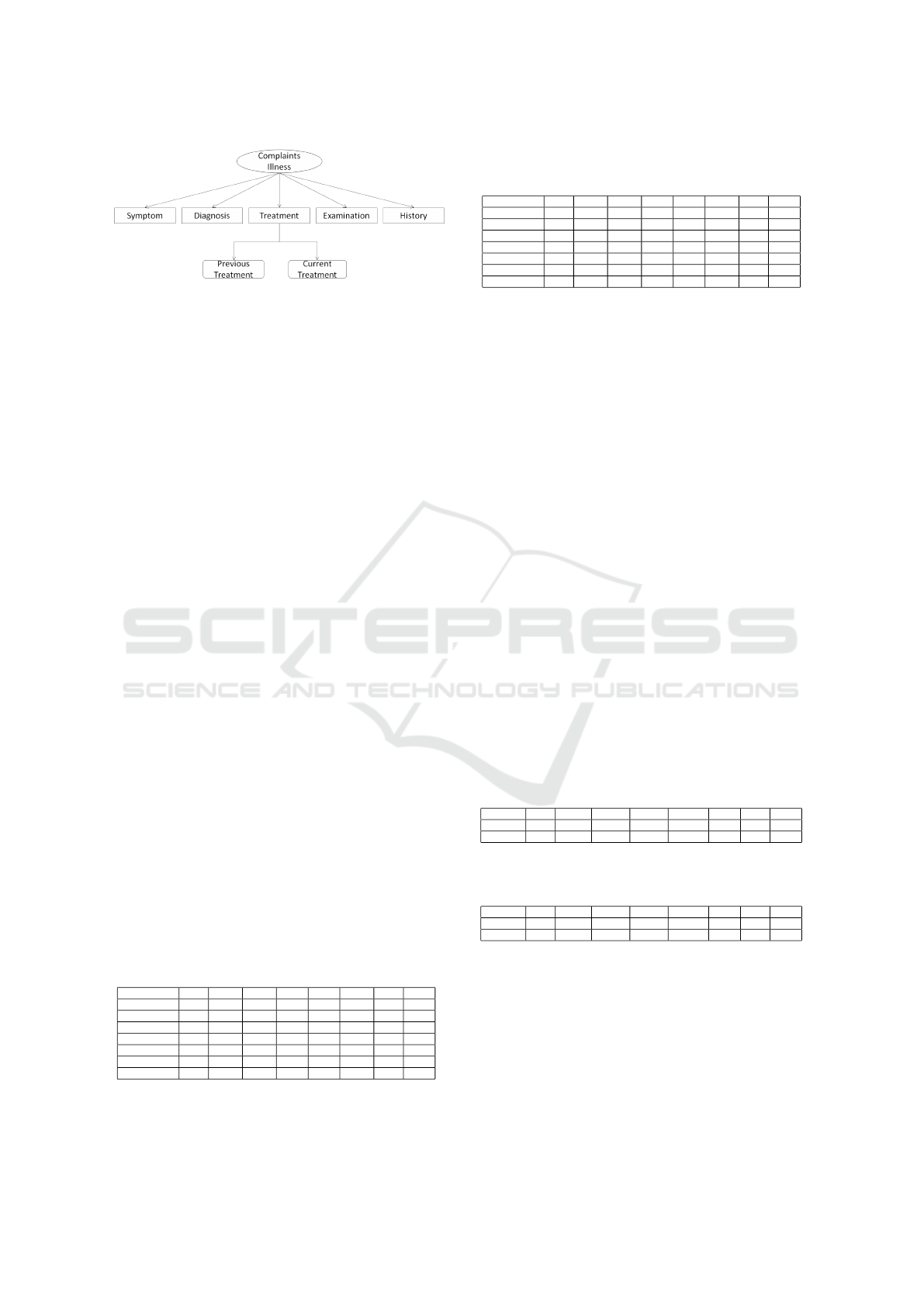
Figure 1: Semantic Entities of Doctor-patient conversation.
tion, checking, cue and giving instruction. We tran-
scribed the audio recordings manually and tabulating
into three categories: Information elicitation or infor-
mation seeking and information provisioning or (in-
formation giving) in the case of the doctor and the
patient in the interaction. We analyzed 29 conversa-
tions done by 4 doctors and 29 patients among 50
patients. We chose only patients coming for diag-
nostic purposes and ignored follow-up patients since
it doesn’t include the elicitation criteria (information
gathering/seeking and information provisioning) and
medical topics (illness, symptoms, diagnosis, treat-
ment, exam/test and history) for diagnostic purpose.
3.2 Results
We have collected data to find out how, in the
Ethiopian context, patients elicit information during
a doctor-patient conversation. Therefore we have
audio-taped 50 real doctor-patient interactions. The
conversations took 6-7 minutes on average. The sta-
tistical analysis of the face-to-face doctor-patient in-
teraction has resulted in the following findings. Out
of 29 medical interactions, comprising of 442 turns,
171 (38%) turns classified as Information gathering,
167 (38%) utterances are uttered by doctors to elicit
health information and only 4 (1%) of the utterances
are uttered by the patients. Table 1 shows the break-
down of the doctor contributions to the doctor-patient
interactions into (variable, topic) combinations. Table
2 shows this breakdown for the patient contributions.
We may interpret this table as an estimator for prob-
abilities as Prob (v—t, a) for variable v, topic t and
actor a (either doctor or patient).
Table 1: Doctor utterances in medical information elicita-
tion process in face-to-face interaction.
Illn Smpt Diag P.Tr C.Tr Exam Hist Total
Information 34 110 9 5 0 1 8 167
Confirmation 0 2 0 0 0 0 0 2
Checking 1 5 9 8 1 4 1 29
Explanation 6 4 9 3 1 5 0 28
Cue 2 1 2 0 1 0 1 7
Instruction 0 0 3 1 0 5 2 11
Total 43 122 32 17 3 15 12 244
Our first conclusion is that the interaction is
mainly led by the doctor. The first dialogue act is a
Table 2: Patient utterances in medical information request
in the face-to-face diagnosis processes.
Illn Smpt Diag P.Tr C.Tr Exam Hist Total
Information 1 2 0 0 0 1 0 4
Confirmation 6 36 1 4 2 2 1 52
Checking 0 28 2 2 0 0 2 34
Explanation 12 76 5 6 0 1 3 103
Cue 0 0 4 1 0 0 0 5
Instruction 0 0 0 0 0 0 0 10
Total 19 142 12 13 2 4 6 198
question posed by the doctor like ’How are you feel-
ing?’. Then the patient explains complaints or feel-
ings (s)he has. The doctor then will ask additional
questions to identify causes, symptoms, and illnesses.
Table 3 and 4 show information seeking and in-
formation provision of doctors and patients. We see
that information seeking behavior of doctors (46%)
is higher than that of patients (10%). Whereas, pa-
tients’ information provisioning behavior (35%) is
much higher than doctors’ (9%). Besides, symp-
toms 60%, illness 14%, diagnosis 10%, treatment 8%,
exam test and history 4% are addressed. In these
doctor-patient interactions the medical topic has been
given much attention during information seeking and
information provision (about 122 turns used by the
doctor for information seeking and 142 turns by pa-
tients to reply the questions posed by the doctor about
the symptoms). The most prominent divergence ap-
pears in the fact that doctors most frequently initiated
questions targeted towards information (68%), much
less frequently towards checking (12%), and even less
frequently towards explanation (11%), giving instruc-
tion (5%), cue (3%) and conformation (1%). The pa-
tients merely were answering the questions posed by
the doctor.
Table 3: Information seeking and information provision be-
havior of Patient.
Illn Smpt Diag P.Tr C.Tr Exam Hist Total
InfoSeek 1 30 2 2 0 1 2 38
InfoProv 18 112 10 11 2 3 4 160
Table 4: Information seeking and information provision be-
havior of doctor.
Illn Smpt Diag P.Tr C.Tr Exam Hist Total
InfoSeek 35 115 21 14 1 10 11 207
InfoProv 8 7 11 3 2 5 1 37
3.3 Discussion
As discussed in the preceding section, turn taking is a
dialogue act. A turn is defined as speaking without in-
terruption. From the doctor-patient audio recordings
we found that the number of turns of doctors is 276
and 238 of the patients. This figure indicates that the
doctor speaks in long turns 56% over patients 46%.
In general, patients talk less than doctors and most
Third International Symposium on Business Modeling and Software Design
264

of their interaction is in the form of giving informa-
tion in response to doctor questions. Many studies in-
dicate that doctor’s dialogue acts encourage patients
to discuss their opinions, express feelings, ask ques-
tions, and participate in decision making. This helps
the doctor to more accurately understand the patient’s
goals, interests, and concerns as well allows the doc-
tors to better align his conversation/interaction with
the patient’s agenda (Goold and Lipkin, 1999; Ver-
linde et al., 2012). On the contrary, some studies re-
port that doctors often underestimate patients’ desire
for information, while overestimating their medical
knowledge (Bickmore et al., 2006). Thus, allowing
patients to ask questions, express concerns and state
preference helps the doctor to infer matters that are
important to patients in relation to their compliance.
Our findings show that the dialogue is initiated
by the doctor in order to seek information about the
patients health compliance and illnesses. Moreover,
the dialogue is controlled by doctors to gather addi-
tional information about the illness (such as symp-
toms, illness history and medication). Generally, the
request for information sets the initial purpose or goal
that motivates the speaker’s actions for the remain-
ing section of the dialogue. The request for informa-
tion further specified by one or more discourse seg-
ments. Asking questions and providing answers play
a significant role in the process of the medical con-
sultation. Mainly, the aim of doctor-centered behav-
ior is efficiently gathering sufficient information to
make a diagnosis and consider treatment options in
the least amount of time necessary. This is in con-
trast to patient-centered interactions that can recog-
nize patients as collaborators who can share not only
their biomedical states (physical condition and well
being) but also knowledge of their psychological sit-
uations (personality, culture, social relations, etc.).
The result of quantitative analysis shows, there still
is an equal distribution of information seeking (ques-
tions) between the dialogue participants, with almost
all elicitation initiated on the part of the doctor. The
data also demonstrate that both doctors and patients
emphasize on asking and responding about symptoms
and illnesses. For example from a total of 442 dia-
logue acts, 122 and 142 dialogue acts are used to elicit
symptom information by doctors and patients. Gener-
ally, 59.7% of the interaction was devoted to seeking
and giving information about symptoms and 14% of
illnesses. The finding show a significant difference
(F= 14.02, P=0.0026, alpha= 0.05 ) between doctors’
and patients’ information seeking behavior in f-test,
but no significance difference is found in patients’ and
doctors’ information giving behavior.
We also analyzed the data using two-way analysis
of variance. We found that the information seeking
score of doctors is higher than for patients, but the
difference is statistically not significant. The score
of information giving behavior of patients was higher
than the doctors, but similarly there is no significant
difference. The first impression about people often
turns into long-term perceptions and reputations. So
doctors in their first encounter should make good eye
contact, shake patient’s hand and introduce himself.
In the face-to-face interaction we recorded that there
were no greetings and introduction during the initial
doctor-patient interaction. In each dialogue sentence
or clauses the participant (doctor/patient) utterance is
categorized into semantic entities (figure 1) in which
the dialogue theme is emphasized. Since the conver-
sation is between a doctor and patient for diagnosis
purpose we identify the main concepts evolved in the
interaction process. Compliant, symptoms, treatment,
illness, exams, history, and prescription are the most
common entities used in the doctor-patient conversa-
tion.
3.4 Cultural Aspects
Cultural differences may be an obstruction for ef-
fective doctor-patient interaction. The cultural per-
ceptions of health, sickness, and medical care of pa-
tients and families may differ with that of the doc-
tors. Speaking the same language and being born in
the same location does not automatically mean shar-
ing all the elements of a particular culture. Studies
have shown that a patient’s culture will affect the way
they perceive their body, illness, and disease. This
is also true for the doctors as their own families and
communities have also helped to shape these cultural
beliefs within them. Each participant in the medical
interview brings with them the culture in which they
were raised. At times, differing cultural beliefs can
have an adverse effect on the care that one receives.
Communication problems arise when the patient and
doctor do not share the same culture.
Culture competencies in medical interaction pro-
vide a patient centered care by adjusting their atti-
tudes and behaviors to the needs and desires of differ-
ent patients and account for emotional, cultural, so-
cial, and psychosocial issues on disease and illness.
Medical competencies relate directly with the doctor-
patient interaction that are required by the doctors to
conduct an effective interview and to create an accept-
able plan of diagnosis and treatment. Studies indicate
that issues that may cause problems in cross-cultural
encounters are authority, physical contact, communi-
cation styles, gender, sexuality, and family.
Hofstede (Hofstede et al., 2010) has identified five
Designing Spoken Dialogue Systems based on Doctor-Patient Conversation in the Diagnosis Process
265

cultural dimensions. (1) Power Distance focuses on
the perceived degree of equality, or inequality. Ac-
cording to Hofstede et al., [2010] ”A high power dis-
tance ranking indicates that inequalities of power and
wealth have been allowed to grow with the society. In
these societies equality and opportunity for everyone
is stressed”. In large power distance cultures, ones
social status must be clear so that others can show
proper respect. In line with this, Hofstede et al. as-
sert that the power distance exhibited in society also
is reflected in the relationship of doctors and patients.
They say that ”in countries with large-power distance
cultures, consultations take less time, and there is less
room for unexpected information exchanges”. The
findings indicate that the average time spent on face-
to-face consultation is 4-6 minutes. This result con-
firms that power distance plays a major role in doctor-
patient interaction. According to Hofstede, Ethiopia
is a large power distance country, so the interaction is
dominated by doctors and patients rarely participated
in treatment and diagnosis decision makings.This is
true especially for illiterate and rural people. The
power distance of literate people and doctors is bet-
ter compared to the illiterate. In line with this (Ver-
linde et al., 2012) said that doctors asked less edu-
cated patients and low income patients more ques-
tions about their disease and medical history. Like-
wise, our findings indicate that doctors’ information
seeking behavior is more than that of patients’. Gen-
erally, in Ethiopia, patients treat doctors as superiors,
consultations are shorter and controlled by doctors.
(2) Hofstede’s cultural dimension indicates that
Ethiopia as a low individualism country. The im-
plication of individualism in healthcare particularly
in doctor-patient interaction goes with patient auton-
omy, the possibility of choice, flexibility of social
roles, less conformity, and psychosocial information
exchange (Meeuwesen et al., 2009)
(3) Ethiopia is a masculine country (Hofstede’s cul-
tural dimension); however, regardless of other dimen-
sions, masculinity doesn’t reflect on the patient - doc-
tor interaction in diagnosis and treatment. Some stud-
ies revealed that there is a difference between female
and male doctors in creating partnerships, with pa-
tients and dealing with psychosocial issues during the
conversation. Meeuwesen et al., [2009] stated that
the more masculine a county, the more instrumen-
tal (disease centered) interaction will dominate, the
less attention will be paid for psychosocial issues and
more frequently the majority of doctors will be men or
male. The analysis result shows that mainly the inter-
action between doctors and patients was on the theme
of symptoms 60% and illnesses 14%. Eventually the
theme of the conversation is disease-centered.
(4) Uncertainty Avoidance in the healthcare domain
primarily deals with patients’ emotionality or anx-
iety, or stress and doctor’s task-orientation, prefer-
ences of technological solution and degree of med-
ication. In countries with strong uncertainty avoid-
ance (Meeuwesen et al., 2009) the more disease-
centered (instrumental talking), the less affective talk-
ing and the more biomedical exchange can be ex-
pected. This a true scenario in Ethiopia cases; since
doctors indulge themselves in diagnosing the illness.
In the experiment, we have not found a single in-
troduction (greetings) communication act. Hofstede
further explained that ”doctors in uncertainty tolerant
countries more often send patients away with com-
forting talk, without any prescription. In uncertainty
avoiding countries doctors usually prescribe several
drugs, and patients expect them to do so” (Hofstede
et al., 2010).
(5) Regarding long-term orientation, as Ethiopia
doesn’t have data we left out in our analysis.
4 A SPOKEN DIALOGUE MODEL
Eliciting user requests in the medical spoken dia-
logue is the main challenge for developers and imple-
menters of the system. Unlike a face-to-face doctor-
patient interaction it is very hard to analyze the pa-
tients’ attitudes and emotions. As a result the eliciting
techniques should be patient centered; and the main
role of the doctor is a facilitating behavior, focused
and unfocused open questioning, request for clarifi-
cation, summarizing and empathy. Thus, the dialogue
system should act like human which can help to elicit
the patients’ request in order to provide accurate con-
sultation, diagnosis and treatment.
To the best of our knowledge eliciting user medi-
cal requests using spoken medical dialogue based on
some suggested principles is not assessed, and there
is no any results obtained. Our objective is using
the best practice of in-person doctor-patient interac-
tion activities to be adopted in the spoken medical
dialogue system to search medical information using
mobile phones.
4.1 A Simplified Dialogue System
Spoken medical dialogue tends to be patient centered.
Thus the system should facilitate the interaction and
ask open questions in which the patients can express
not only knowledge of their biomedical state (illness
and complaints) but also knowledge of their psycho-
logical and social situations (personality, culture, re-
lationships). As discussed before, the face-to-face in-
Third International Symposium on Business Modeling and Software Design
266

teraction in Ethiopia is doctor dominated. However,
in the dialogue system it is impossible to detect the
non-verbal behavior of the patient. Thus, the elicita-
tion should be dominated by the patient in order to
seek biomedical as well as psychosocial situations of
the patient. Doctor’s behavior that encourages patient
active participation includes asking open ended ques-
tions, ensuring and confirming patient comprehen-
sion, requesting patients’ opinions, and making state-
ments of concern, agreement and approval. Hence,
spoken dialogue to resemble human-human interac-
tion, should encourage patients to take part actively
in the interaction process. Instead of being expecting
responses from patients, the system must take a fa-
cilitative role in order to provide time and space for
patients to speak out what their symptoms, illnesses,
suggestions and to participate in decision making.
From the analysis of the in-person interaction of
doctors and patients, it was found that there are some
gaps that should be filled. The main gaps observed
in the face-to-face interaction is doctor domination as
well as we identified that the social status of patients
and doctors inhibits the interaction process. Other
factors that affect the face to face interaction are il-
literacy and culture. In rural Ethiopia, the illiteracy
rate is higher than in urban areas, so patients from
rural areas visited find the interaction with the doc-
tor is difficult; the doctor may consider that non ed-
ucated rural patients do not express themselves so
that a doctor prefers to ask some closed questions and
open leading questions to elicit the user requirements.
But even when doctors and patients born and live in
the same area, they do not necessarily have the same
understanding of social norms and cultures. Conse-
quently, the non-literate rural patients are more con-
servative of their values and cultures; some of the ill-
ness may not be disclosed in public so to keep their
culture or values they reserved from disclosing their
feelings, symptoms and illnesses. For instance, a
study conducted in USA revealed the gap between
doctors and Ethiopian migrants in disclosing illnesses
and diseases. According to this study, the migrants
did not want to be told if their disease is life threat-
ening; whereas, doctors in US disclose the nature of
the illness, the risks of the illness (curable and incur-
able) and the magnitude of the illness (treatable or
non-treatable) (Beyene, 1992).
From the face-to-face doctor-patient interaction
we deduce the user request elicitation model dis-
played in figure 2 for spoken dialogue system for
healthcare application. The model consists of four
components: opening initiatives, asking information,
giving information and closing. Figure 2 displays user
request elicitation process for the spoken dialogue
systems in a healthcare scenario based on doctor-
patient face-to-face dialogue.
4.2 Design Dialogue System
Data validity, accuracy and integrity are the vital
points to be considered in designing a spoken dia-
logue application; since automatic speech recogni-
tion(ASR) technology is not perfect. The design
of spoken dialogue technology should take into ac-
count the possibility of speech recognition errors and
improve the overall accuracy using dialogue actions
such as re-prompts, conformations, error correction
and handling etc. Secondly, it should provide equal
access to novice and experienced end users of the
system. Thirdly, it should also consider individual
differences such as personalization and user context.
Finally, before developing the dialogue system it is
very important to conduct a face-to-face interview or
pay live observation while a doctor is treating a pa-
tient (if possible video tape the conversations). The
most commonly applied methods to design a spoken
dialogue include human-human dialogues and design
by simulation. Thus, our interest lies on to look into
doctor-patient interactions as a means to design med-
ical spoken dialogue.
Figure 2: User request elicitation process.
4.3 Designing a Dialogue based on
Doctor-Patient Interaction
Human-human dialogue provides an insight how hu-
mans accomplish a task-oriented dialogue. The
doctor-patent interaction studies take place in the
early stages of the speech application life cycle. They
act as a starting point for spoken dialogue design and
help to define requirements. The purposes of doctor-
patient interaction studies are to help the designer see
the task form the user point of view, develop a feeling
for the style of interaction, and acquire some specific
knowledge about the vocabulary and grammar used in
the diagnostic process.
Designing Spoken Dialogue Systems based on Doctor-Patient Conversation in the Diagnosis Process
267

Doctor-patient interaction (natural dialogue) study
differs significantly from the wizard-of-oz studies,
that have been used extensively by others in the design
of spoken dialogue systems. Researchers who use the
wizard-of-oz techniques begin the process with a pre-
experimental phase that involves studying natural hu-
man dialogues. Whereas the natural dialogue takes
place prior to any system design or functional specifi-
cations (Yankelovich, 2008). The main purpose is to
launch the design process.
Before designing the medical dialogue system, we
wanted to discover how doctors and patients inter-
act in the diagnosis process. From the analysis of
the doctor-patient interaction, we found that the in-
teraction is doctor-centered as well as we found that
patients question asking behavior is hampered by the
cultural influences such as: distance power, high un-
certainty avoidance and the like (see section 3.5).
It is impossible to produce a medical dialogue sys-
tem design based entirely on doctor-patient face-to-
face interaction. Rather it can play an important role
in the early stages of the development life cycle, and
serve as an effective starting point for spoken medical
dialogue system design.
5 CONCLUSIONS
We have analyzed the interaction in 29 audio-taped
doctor-patient diagnosis dialogues in the Gamby
Teaching hospital. The study is mainly conducted
to investigate the information seeking and informa-
tion provisioning behavior of doctors and patients.
The finding shows that there is no statistical signif-
icant difference between doctor information seeking
and patient information seeking behavior. Similarly,
we didn’t find any significant difference between pa-
tients information provisioning and doctors informa-
tion provisioning behavior. From this analysis we
conclude that studying face-to-face interaction be-
tween doctor and patients is an effective starting point
for spoken medical dialogue system design. We also
found an influence of culture on doctor-patient in-
teraction; so cultural values should be incorporated
while designing and developing a medical dialogue
system. Finally, based on our results, we propose a
model to assist user requirements elicitation in order
to develop a medical spoken dialogue system. In the
future we will implement our model to develop a med-
ical dialogue system.
REFERENCES
Beyene, Y. (1992). Medical disclosure and refugees - telling
bad news to ethiopian patients,. The Western Journal
of Medicine, 157(3):328 332.
Bickmore, T. and Giorgino, T. (2006). Methodological
review: Health dialog systems for patients and con-
sumers. Biomedical Informatics, 39(5):556–571.
Bickmore, T., Giorgino, T., Green, N., and Picard, R.
(2006). Special issue on dialog systems for health
communication. Biomedical Informatics, 39(5).
Bickmore, T., Gruber, A., and Picard, R. (2005). Estab-
lishing the computer-patient working alliance in auto-
mated health behavior change interventions. Patient
Educ Couns., 59(1):21–30.
Black, J., Koch, F., Sonenberg, L.and Scheepers, R., Kahan-
doker, A., Charry, E., Walker, B., and Soe, L. (2009).
Mobile solutions for front-line health workers in de-
veloping countries. In Healthcom, pages 89–93.
Celi, L., Sarmenta, L., Rotberg, J., Marcelo, A., and Clif-
ford, G. (2009). Mobile care (moca) for remote diag-
nosis and screening. Journal for Health Informatics
in Developing Countries, 3(1):17–21.
Durling, S. and Lumsden, J. (2008). Speech recognition use
in healthcare applications. In MoMM 2008.
Foster, C. (2011). Icts and informal learning in developing
countries.
Goold, S. and Lipkin, M. (1999). The doctor patient re-
lationship challenges, opportunities, and strategies. J
Gen Intern Med., 14(Supp1):26–33.
Hofstede, G., Hofstede, G., and Minkov, M. (2010). Cul-
tures and Organizations: Software of the Mind: In-
tercultureal Cooperation and Its Importance for Sur-
vival. McGraw Hill.
McTear, M. (2002). Spoken dialogue technology: Enabling
the conversational user interface. ACM Computing
Survey, 34(1).
Meeuwesen, L., van den Brink-Muinen, A., and G., H.
(2009). Can dimensions of national culture predict
cross-national differences in medical communication?
Patient Education and Counsiling, 75:58–66.
Migneault, J., Farzanfar, R., Wright, J., and Friedman, R.
(2006). How to write health dialog for a talking com-
puter. Biomedical Informatics, 39:468–481.
Nevile, M. (2006). Communication in context: A conver-
sation analysis tool for examining recorded voice data
in investigations of aviation occurrences. Technical
report.
Nowak, P. (2011). Synthesis of qualitative linguistic re-
searcha pilot review integrating and generalizing find-
ings on doctorpatient interaction. Patient Education
and Counseling, 82(3):429–441.
Verlinde, E., De Laender, N., De Maesschalck, S., De-
veugele, M., and Willems, S. (2012). The social gra-
dient in doctor-patient communication. International
Journal for Equity in Health, 11(12).
Yankelovich, N. (2008). Using natural dialogs as the basis
for speech interface design. Human Factors and Voice
Interactive Systems Signals and Communication Tech-
nology, pages 255–290.
Third International Symposium on Business Modeling and Software Design
268
