
More Time for the Doing, Having Made the Thinking
3D Printing for Knowledge Circulation in Healthcare
Federico Cabitza
1,3
, Angela Locoro
1
, Aurelio Ravarini
2
and Vittorio Satta
2
1
Università degli Studi di Milano–Bicocca, Milano, Italy
2
Università Carlo Cattaneo – LIUC, Castellanza, Italy
3
IRCCS Istituto Ortopedico Galeazzi, Milano, Italy
Keywords: DiDIY, Medical 3D Printing, Diagnostic, Training, and Surgical Tools, Knowledge Circulation in Healthcare.
Abstract: This paper investigates the phenomenon of the Digital Do-It-Yourself (Di-DIY) in the medical domain. In
particular, the main contribution of the paper is a conceptual framework based on the notion of DiDIY in
healthcare. To help focus on the main actors and assets composing the 3D printing innovation roles in
healthcare we model: the DiDIY-er as the main initiator of the practice innovation; the available technology
allowing the envisioning of new practices; the specific activities gaining benefits from the innovative
techniques introduced; and the knowledge community continuously supporting and evolving knowledge
practices. A general introduction on the notion of Knowledge Artifacts (KAs) and on the use of 3D printing
(3DP) in medicine will be followed by our research questions and by a more detailed analysis of diagnostic,
training and surgical planning activities for clinicians and patients. Observations carried out in a hospital in
Italy are reported to exemplify activities based on 3DP bone models in the radiological and orthopaedic fields.
These observations can be considered a second contribution of the paper, although secondary with respect to
the conceptual framework. They also help proof how knowledge sharing and circulation in the community of
healthcare professionals may be improved by the introduction of tangible and intangible KAs around the
practice of DiDIY. Our framework is then presented in the end.
1 INTRODUCTION
A knowledge artifact has been defined (Cabitza et al.
2014c) as any artifact that is purposely designed to
support knowledge-related activities in any practice.
Although this is an (intentionally) broad definition, it
allows to exclude most of the tools that are used in the
human activities where users do not rely on these
tools to take decisions, access a body of notions that
are useful to interpret or understand a situation, or to
solve a problem and complete a task relying on past
experiences and solutions.
After a comprehensive survey of the varied
literature available on this matter, Cabitza and Locoro
(2014a) identified two main perspectives along which
to conceive this class of artifacts: objectivity and
situativity. These are seen as two extremes of a broad
spectrum of application solutions, which often offer
functionalities that cannot be traced back to only one
extreme but rather lie in between. What do these two
terms refer to? At the former extreme, there lies the
idea that knowledge can be expressed in explicit and
linguistic forms, in terms of guidelines, procedures,
rules and notions. As such, knowledge is somehow
quantifiable (e.g., in terms of how many statements,
rules, notions constitute it); it exists independently of
any possible consumers, like a book on a library shelf;
and it can be transferred from one place to another,
e.g., by email or a courier. Therefore knowledge is
seen as if it were an object for any practical purpose
(hence the name of the approach). At the situativitist
extreme, instead, knowledge is assimilated to a
knowledgeable behavior that competent people
exhibit during a specific situation and within a social
practice. This latter is seen as a set of activities where
more or less explicit rules and conventions that are
shared within a social group stipulate and normate the
right way to have things done, and where an often
totally ineffable know-how allows the practitioners to
accomplish their tasks. In the situativist case, KAs are
those artifacts that enable the sharing of ideas, the
learning process and the mediation of collective
activities of problem framing, agreement reaching
and decision making, without knowledge being
Cabitza, F., Locoro, A., Ravarini, A. and Satta, V.
More Time for the Doing, Having Made the Thinking - 3D Printing for Knowledge Circulation in Healthcare.
DOI: 10.5220/0006095402890298
In Proceedings of the 8th International Joint Conference on Knowledge Discovery, Knowledge Engineering and Knowledge Management (IC3K 2016) - Volume 3: KMIS, pages 289-298
ISBN: 978-989-758-203-5
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
289

objectified in any form (neither as written facts nor
written rules) as above.
This objective-situative spectrum regards the
degree of specification (high in objective KAs and
low in situative KAs – Cabitza et al. 2013) and the
very way in which knowledge is conceived (cf.
objectivism vs constructivism – Vrasidas, 2000). In
this contribution, to this dimension we add two
further dimensions regarding interactivity, and
tangibility. KAs can be either passive or interactive.
And they can be either tangible or intangible.
The latter dipole allows to distinguish, quite
sharply, between software applications and physical,
tangible objects. The former KAs are certainly
“physical” (and often even material) in that their users
can perceive them, but their way to show themselves
is through patterns of energy and matter that could
hardly be touched (in this light a mouse is just a
tangible controller to move a pointer on the screen,
but the real application regards bit of energy in
memory modules or pixel grids). Tangible objects,
which we all are very familiar with, are usually
passive, but this is not necessarily always the case: a
washing machine, for instance, can be touched
(indeed, it is even quite heavy) but through some
controllers it can also respond to the users’ commands
and settings and through sensors can “take decisions”
on how to proceed in carrying out its washing
programs. On the other hand, not all of the intangible
(software) objects are interactive in the same way, nor
necessarily so their level of interaction matters. For
instance, the Wikipedia, although it is a very
comprehensive and convenient source of knowledge
(in an objectivist viewpoint), responds to the user’s
textual query and allows just to open new pages from
the links of another one, that is a sort of basic
interaction; but it is not proactive in its provision of
knowledge nuggets, facts, taxonomies and
procedures, as an expert system would be; rather it is
reactive. To the other extreme, there are decision
support systems, that is software systems that, once
been fed in with the available information about a
case, suggest ways to classify, treat or manage it (e.g.,
in the healthcare domain, in the legal one and in
Customer Relationship Management). These are very
interactive intangible KAs, which can even surprise
its users (and indeed rightly so they consult it to get
indications they still ignore).
In our studies, we identified two extreme
examples of KA: shapes produced with 3D Printing
(3DP) technology, in particular bones and anatomical
parts printed by radiologists and orthopaedic
surgeons. And social media that support the practices
of the professional roles mentioned above, by
providing videos, blog articles, guides and a place for
DIYers, makers and 3DP enthusiasts in the
orthopaedic surgery domain to ask questions and
exchange advice. This latter case also regards the
increasing use of intangible and interactive KAs that
can support (in a more less objectivist/situativist
manner) the pioneers and early-adopters of 3DP
technologies for their delicate and often very difficult
work (consisting in very complex surgery aimed at
correcting important deformities and alleviating
multiple pathological conditions).
Although both cases are important and worthy of
further research, in this paper we will focus on the
former case, 3DP, in order to both keep the scope of
the paper circumscribed, and also to acknowledge the
increasing relevance of the literature contributions on
embodiment (Dourish, 2001; Lakoff & Johnson,
1999; Varela et al., 1991), which argues for a close
link between physical activity and cognition and on
the role of physical manipulative materials in
supporting learning (Rybarczyk & Fonseca, 2012;
Hornecker & Buur, 2006; Pernin et al., 2012). In the
same vein, we observed how relying on situativist,
tangible and passive KAs, rather than only 2D
representations, improved planning, communication
and decision making in the orthopedic settings we
studied. In what follows, we will interpret these
observations referring to the concept of Digital Do-
It-Yourself (DiDIY), that is a complex phenomenon
that we are characterizing within the DiDIY EU
funded project (DiDIY, 2016) in which either an
amateur or a professional (which we call DiDIYer)
builds up material artifacts by herself with 3D
printing technologies for her job and daily work,
without the aid of specialists.
1.1 Research Questions
Our research topic focuses on the impact of Digital
Do-It-Yourself (DiDIY) and 3D printing (3DP) on the
healthcare practices, training and communication
processes. All of these ambits have in common the
exploitation of knowledge and knowledge artifacts in
different forms (Cabitza et al. 2014c). Healthcare
practitioners rely most of the time on a kind of tacit
knowledge based on their training, “situation specific
wisdom”, and narrative exchange of real cases with
their peers (Greenhalgh and Wieringa, 2011).
Traditional training techniques in health education
are mostly based on human cadavers dissection and
inspection, either for school teaching or pre-operative
simulations (McMenamin et al., 2014; Regier et al.
2010). Finally, pre-surgical, intra-operative and
patient-specific communication are well known to be
KITA 2016 - 2nd International Workshop on the design, development and use of Knowledge IT Artifacts in professional communities and
aggregations. Knowledge Artifacts as resources in the maker and DIY communities
290

delicate moments where improving the awareness for
patient consenting (de Mel, 2016; Starosolski et al.,
2014; Regier et al., 2010), the shared understanding
in surgical rehearsal (Mitsouras et al. 2015) and the
rapid decision-making during the ongoing operation
may be of vital importance.
Consequently, our research questions regard
whether and how DiDIY processes and artifacts may
influence, enhance and guide the mechanisms of
knowledge circulation (Cabitza et al., 2014b) in
medical settings, and in particular in radiological
practice either by single doctors or in cooperation
with other clinicians. In summary, they are the
following:
Do 3DP artifacts modify diagnostic and
therapeutic decision making?
Do 3DP artifacts modify training and teaching in
radiology?
What are the dynamics of knowledge circulation
between members of hybrid communities and the
hospitals where they work?
Some preliminary answers can be found in this study,
where we elaborate a DiDIY framework tailored on
the specific healthcare domain that should help focus
on the main actors, technologies, activities and
communities involved.
We report in this study some early reflections, on the
basis of the specialistic literature and of the existing
online communities, mentioned in Section 2, and in
observational studies carried out in an Italian hospital,
from which some vignettes have being extracted and
are reported in Section 3 and discussed in Section 4
where we introduce our framework; Section 5 draws
some conclusions on our study.
2 BACKGROUND
2.1 The Technology at Hand
In the healthcare literature, 3D printing is finding its
place in different facets of the professionals practice.
We will shed light in particular on the practice of
surgery, orthopaedics and radiologists, starting from
the technical process of medical 3DP.
For reproducing patient-specific anatomy, 3DP
objects are generated from medical imaging acquired
through either Computer Tomography (CT) in its
several variants (e.g., Multidetector Computer
Tomography (MDCT), Single Photo Emission
Computer Tomography (SPECT), and so on) and
Magnetic Resonance Imaging (MRI). A second step
of this elaborate acquisition is the saving of imaging
data into Digital Imaging and Communication in
Medicine (DICOM) format. A further step consists in
the 3D rendering of the image, by segmentation
techniques, which can be manual, automatic or semi-
automatic (Auricchio and Marconi, 2016), depending
on the complexity of the data managed. Segmentation
allows to place regions of interests on the images for
further volumetric refinement (Mitsouras et al.,
2015). During segmentation, a 3D model of the
acquired image is rendered as a geometrical
transformation into a set of triangles (called mesh),
which allows the data to be readable by a 3D printer.
One of the most common 3D files format for 3D
object printing is the Standard Tessellation Language
(STL), which refers to the property of the image to be
represented as a set of triangles, at different degree of
precision (or smoothing). Commonly, a 3D model is
then virtually cut into equally-thin horizontal slices,
and each slice can be printed in various materials
(e.g., “powder, resins, filaments and hydrogels” – see
de Mel, 2016 and Mitsouras et al., 2015) and laid
down as a layer of the 3D object. Each slice is then
fused together with the just printed layers, according
to disparate techniques using chemical and physics
processes (e.g., photopolymerization, material
jetting, material extrusion, powder bed fusion, sheet
lamination, direct energy deposition, and so on –
Auricchio and Marconi, 2016; Rengier et al., 2010;
Malik et al., 2015). Figure 1 depicts some main
passages from the acquiring of an image to the printed
object.
2.2 A Quick Glimpse at the Literature
A 3D printed object is very different from a 3D virtual
object. Recent comparative studies of 3D virtual and
material objects in manipulation tasks have shown
that “performance during the activities was
significantly higher when using tangible representa-
tions” (Cuendet et al., 2012). In healthcare domain,
this has proven to give a pre-operative visuo-haptic
capability to physicians of unprecedented flexibility
and precision (de Mel, 2016). 3DP objects can be
exploited to gain a huge amount of patient-specific
detailed and clear information before a complex
surgery takes place, for example in case of
deformities correction. Obviously, not all the
activities need the use of 3DP, and this is especially
evident in diagnostics and classification tasks
(Mitsouras et al., 2015). A literature survey (Malik et
al., 2015) on around 500 papers retrieved from
Medline, Embase and PsychInfo databases, helps
detect the three main areas where 3DP is currently
exploited in surgery. They are: anatomic models,
More Time for the Doing, Having Made the Thinking - 3D Printing for Knowledge Circulation in Healthcare
291
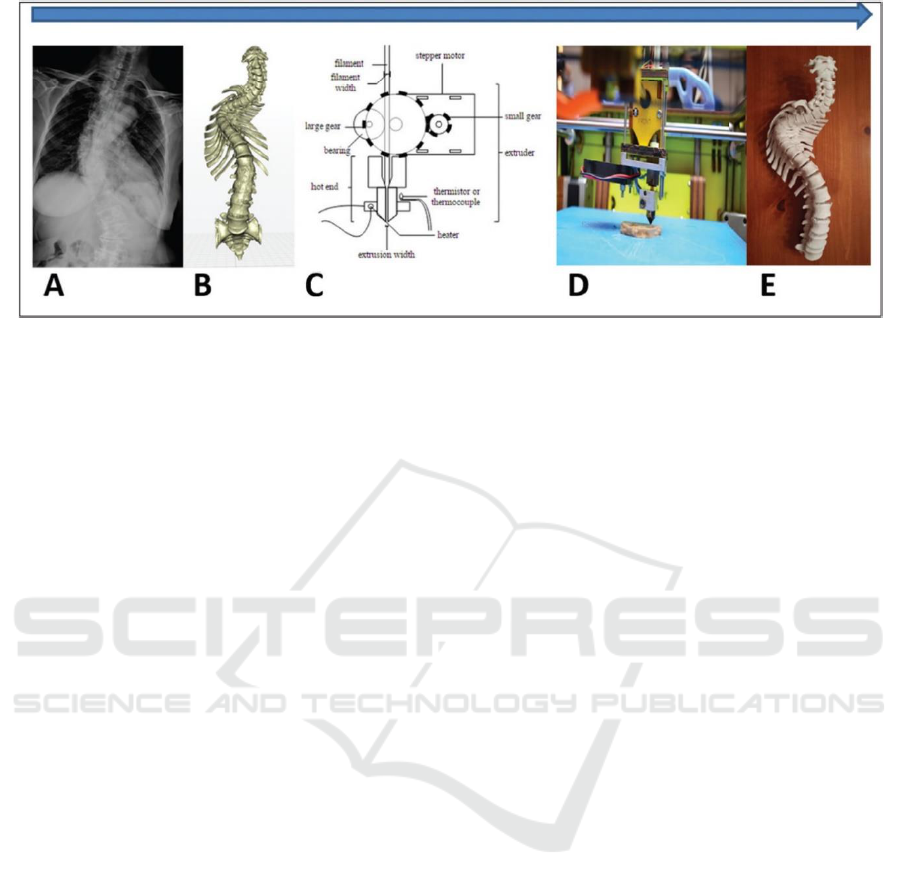
Figure 1: The process from the virtual image to the printed object, taken from Eltorai et al. (2015).
medical devices like surgical instruments and
implants, and prostheses. Anatomic models are used
by doctors to familiarize with the patient anatomy in
surgery planning, and help them reflect on the
challenging and risky passages of an operation well
in advance. This patient-specific appreciation
overcomes traditional simulations (see, for example
Malik et al. 2015; Rengier et al., 2015). In some cases,
for example cardiothoracic surgery, bespoke heart
models are exploited either for planning and for intra-
operation activities. Young surgeons can be trained
(Malik et al., 2015) through the manipulation of these
objects besides traditional virtual patients
environments (Cabitza et al., 2016), which help
“simulate in vivo conditions and real tissues without
any risk of patient complications” (Rengier et al.,
2015). Also patients and their family may be better
informed on the pathology at hand and the necessary
therapy, and this helps the psychological conditions
under which a surgery can be understood, accepted
and perceived as satisfactory (Malik et al., 2015).
In orthopaedic surgery, where “radiographs are
used routinely […] yet they provide inadequate
information on the precise 3D extent of bone defects”
(Auricchio and Marconi, 2016), 3D models are
exploited to assess tools trajectories, to measure and
prepare materials for fixing bone fractures and
placing plates and screws in advance (e.g., assessing
surgical manoeuvres for the placement of pedicle
screws in spinal surgery). Patient-specific guides and
templates are also printed in 3D and used during the
operation as supportive devices that are removed at
the end. In the maxillofacial reconstruction or in the
implants placement, for example, these kind of
devices have reduced the time of operation and
improved the efficacy of the outcomes (Malik et al.
2015).
In low error-tolerance scenarios, such as for
example in neurosurgery, the 3D reproduction of the
skull or of the tumors may help understand the exact
resection boundaries and provide a level of accuracy
that reduce risks, operation time and the number of
errors and adverse events (Mitsouras et al., 2015).
A pivotal factor in favour of the manipulation of
medical imaging for 3DP technology adoption is that
radiologists and radiographers, as more and more
“image guided surgeries call for radiology to become
strongly integrated in a therapeutic team together with
different surgical specialists” (Rengier et al., 2010)
are acquiring prominent roles. However, open issues
rise in the passage from data images into 3D
prototypes as this encompasses “a multidisciplinary
array of fields involving knowledge ranging from
data acquisition, image post-processing and
manufacturing of the prototype by various
techniques” (ibidem). The authors contend that
although radiologists may facilitate the introduction
of additive manufacturing in healthcare, this
integration would result difficult, if feasible at all,
without a close cooperation with other roles such as
computer scientists, material experts, clinicians and
other healthcare professionals.
At the frontier of 3D printing technologies we also
mention bioprinting, i.e., the reproduction of cellular
tissues and the related organs for implantation in
human bodies. Since research studies are still
preliminary, we do not treat them here and refer the
interested reader to the overview by Mok et al.
(2016).
2.3 Online Communities in the Medical
Field
Communities in the field are those of physicians who
meet periodically with 3DP professionals in their
KITA 2016 - 2nd International Workshop on the design, development and use of Knowledge IT Artifacts in professional communities and
aggregations. Knowledge Artifacts as resources in the maker and DIY communities
292

universities, institutions and research centers, where
a broad spectrum of experimental activities takes
place. This aspect is witnessed for example by our
observational studies reported in Section 3.
Virtual communities of makers exist and gather
around online platforms such as 3D Slicer (Fedorov
et al., 2015), an MIT initiative, which provides a
mature, open source, and fully-fledged software
platform specialized in “image guided therapy”.
Intelligent online platforms such as POIGO (Popescu
et al., 2015) aim to integrate medical expertise with
the manufacturing of tools for the so called
personalized surgical templates, an increasing
popular range of tools for helping surgeons customize
their operations around their patients, and reduce
costs, risks and adverse events.
Other kind of tools are online blogs and reference
websites that help gain knowledge on specific health
topics and techniques, and are tailored for specialists
of different kind; for example: the Italian blog
“Fermononrespiri” (http://fermononrespiri.com/)
where discussions on MRI, CT, and diagnostic by
images are the main topics discussed by the
participants to the online forum that the website
provides; “Embodi3D” (http://www.embodi3d.com),
where a virtual community gathers around virtual
spaces such as blogs, forums, textual tutorial and
“how-tos” for 3DP, a marketplace where to buy and
sell biomedical models, and a training section with
training models, realized with the aid of health
professionals (e.g., 3D vascular models such as
venous models and arterial models).
3 OBSERVATIONAL STUDIES
In our study, we had the opportunity to carry out two
observational studies in the Marino hospital in
Cagliari, Italy. This hospital is near to be dismissed,
since the recent regional policy making decision of
cutting administrative costs. However, currently the
hospital hosts healthcare figures of both professional
and academic kind, in the two local specializations of
traumatology and emergency surgery. The hospital is
one of the only two hospitals in the Sardinia Island
equipped with hyperbaric chambers. Its main areas of
orthopaedic expertise are hip and knee surgery, upon
which we will focus our investigation. In particular,
we will examine a case where the introduction of
additive manufacturing (3DP) has been used to
support the planning and pre-operative training of a
knee prosthetic surgery.
This is not the case of an ex-novo, patient-specific
3D printing of a knee prosthesis (re)production, but
of a traditional bone-prosthesis replacement, with the
support of an anatomic model of the patient bones,
exploited to support and enhance the outcome of a
traditional surgical practice.
We depict in the following two vignettes on how
3DP is used to inform and educate the patient to know
more of his pathology and of the subsequent therapy,
as well as for surgical rehearsal.
3.1 The Patient Informed Consent
It is Monday morning. Today Prof. Bones will
explain the pros and cons of the procedure of knee
replacement surgery that Marco Poli (male, 58 years
old) will decide to undertake or not. In case he decides
to do it, he will sign the informed consent form.
Prof. Bones, the orthopaedic surgeon, met Mr.
Poli previously and, during that occasion, he
prescribed to him routinely examination tests such as
blood, urine, drugs intolerance, and a radiography. By
reporting the radiologist report of this last exam Prof.
Bones realized the morphological deformities and
damages affecting the patient’s knee joint and the
need for Mr. Poli to undergo a surgery.
For this reason, once the surgeon analyzed the
report, he prescribed to Mr. Poli a second and more
complete diagnostic examination: a CT, with the aim
to obtain from it a 3D dataset in DICOM format and,
hence, to use addictive manufacturing to create a
patient-specific anatomical model before the meeting
with him during the day hospital session. In so doing,
Prof. Bones could further investigate the patient-
specific problem and let Mr. Poli see and touch first
hand the tangible representation of his condition,
through the replica of his irreversibly injured
articulation.
Monday it’s the day where other tests are done,
more extensive and specific, to gather information
about the patient’s anamnesis. In particular, physical
examinations are aiming at assessing movement,
stability, strength, and alignment of the patient’s
joint, and a more specific test (an MRI) was aimed to
better analyze the anatomy of his soft tissue (muscles,
tendons, and cartilage).
The study of Mr. Poli’s anamnesis already
showed a compound fracture dating back to when he
was 32, which involved the femur to come closer to
the same left knee region now under examination. In
addition, during these last exams, Prof. Bones
evaluates the condition of the damage caused by post-
traumatic arthritis, which severely limits the patient
in articular functionality by afflicting him with
persistent pain, and pronounce himself in favour of
the joint replacement as a treatment of election.
More Time for the Doing, Having Made the Thinking - 3D Printing for Knowledge Circulation in Healthcare
293
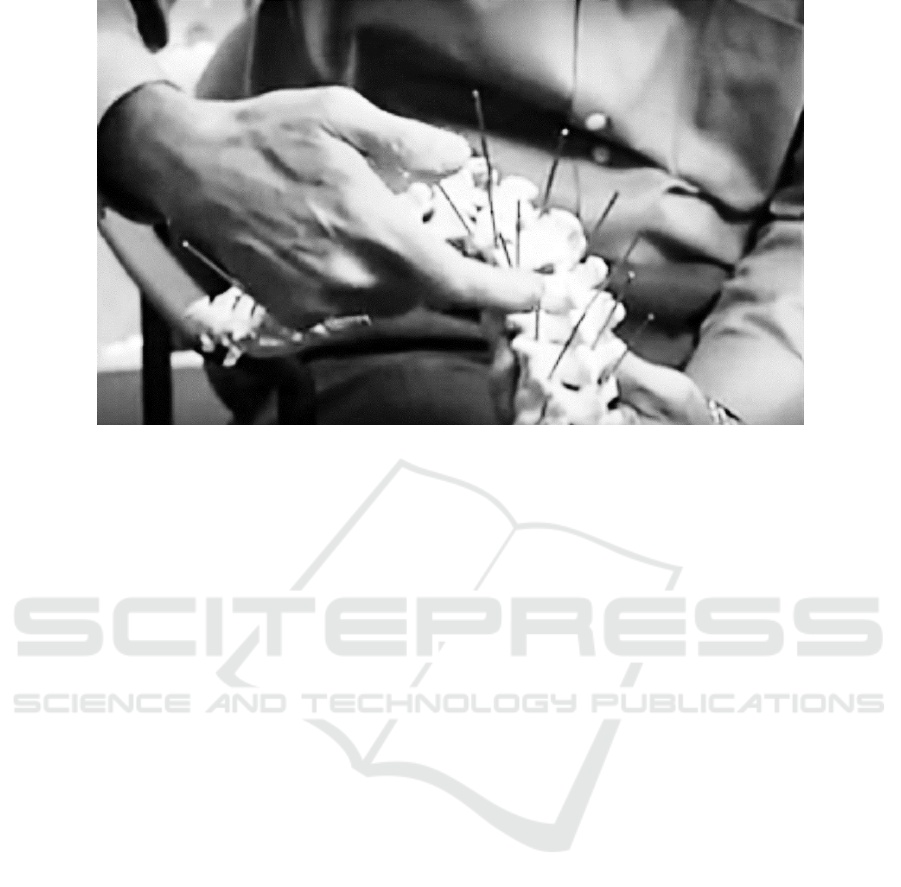
Figure 2: A 3DP spine with implanted nails for pre-surgical rehearsal.
Now Prof. Bones is ready to talk to Mr. Poli, who
may appreciate his own case also with the aid of
anatomic models reproducing his articulations, and
that the surgeon made ready before their meeting.
Thanks to them, the surgeon can show with precision
to the patient which parts of his knee are irreducibly
deteriorated, which operation Mr. Poli should
undergo to his bottom femur and top tibia to let the
articulation work out again, and to hypothesize with
him the exploitation of the proper traditional
prosthesis having the best dimensions similar to his
original bones.
In so doing, Mr. Poli understands vividly his case,
and is able to integrate these information with those
reported in the informed consent form. Mr. Poli,
under a mood of psychological relief for the
awareness gained during the meeting with the
surgeon, agrees to the operation.
3.2 The Surgical Planning
The Friday before, the orthopaedic surgeon met the
radiologist to discuss in more details the case at hand
and asked him whether he recommended to run a
further test in order to use additive manufacturing
with the case at hand. The radiologist proposed to do
an MRI scan, and to call Dr. Bolt, who is a
professional consultant in the field of additive
manufacturing and 3D technologies applied to
prosthetic surgery, with the aim to print a 3D model
of the patient’s joint bones. In particular, the
radiologist asked Dr. Bolt to do an evaluation of the
most appropriate acquisition parameters, in order to
optimize the effectiveness of the dataset for later use
with additive manufacturing technologies.
Both MRI and CT results are exploited in order to
obtain the most accurate reproduction of both the hard
and soft tissues of the patient-specific anatomical
model.
The surgeon then calls the professional
consultant, with whom he agrees upon which are most
appropriate materials and processes to be used. An
anatomical replica of the patient’s hard tissues should
be produced by using Fused Deposition Modeling
(FDM) technology and Polyethylene terephthalate
glycol-modified (PETG) material, as this can be
submitted to antibacterial sanitizing processes, if
necessary. An anatomical replica of soft tissues
should be produced by stereolitography (SLA) and
photosensible resin, which is a soft and flexible
material that could be also compatible with some
sanitizing procedures.
Thanks to the 3DP custom-made models the
surgeon and his team may start the surgical planning.
The surgeon studies the osteotomy planes, performs
measures of trajectories and lengths of the necessary
perforations by simulating them directly in the
anatomical models.
In so doing, the surgeon may transfer all the
necessary data to the consultant, so that he can in his
turn create the anatomic replicas, the surgical guides
and all the supporting material for the operation. For
example, he may prepare the osteotomy planes in the
custom-made models with the cuts and the holes
already performed on them, through FDM and SLA
technologies, and under the direct supervision of the
KITA 2016 - 2nd International Workshop on the design, development and use of Knowledge IT Artifacts in professional communities and
aggregations. Knowledge Artifacts as resources in the maker and DIY communities
294

surgeon, who can simulate the operation moments in
minute detail.
The software used in this phase allows the
application of osteotomy planes and holes, the
creation of scaffolds for dimes and the 3D models
availability of virtual existing surgery environments.
Furthermore, in case that a prostheses has
undergone a 3D scanning process or simply its 3D
models are available from the manufacturer, it is
possible to pre-operatively overlap 3D prosthesis
models with custom-made anatomical models, so that
the prostheses fitting the patient’s bones size can be
easily selected.
After this surgical rehearsal, some comparisons
and verifications of the obtained results are still
possible. In this sense, the surgeon verifies all the pre-
operative process details by applying a real prosthesis
of the same size of the one used in the surgical
planning phase.
3.3 Some Cost-effort Data and Lessons
Learnt
3DP is not cost nor effort free. In the specific cases,
different phases before the printing were carried out,
namely: image of bones acquisition; DICOM data
storage and transfer (after the clinicians’ decision on
what to print); rendering, segmentation and triangula-
tion for the generation of the 3D model; further
editing and preparation (with the aid of the clini-
cians); slicing and G-code generation (for program-
ming the printer). These pre-printing activities takes
on average from 4 to 20 working hours. The printing
of the patient-specific bones took around 50 hours.
The costs depend on the printing technologies (e.g.,
either Stratasys or MakerBot printers, whose costs
vary from 60.000 to 4.000 euros, respectively), on the
materials used, and on the level of standardisation of
these materials with respect to standards such as ISO
and so on. For the case at hand, these may vary from
an average of 50 to 250 euros per kilo. In the specific
case, the 3DP bones were accurate enough to
guarantee similar material characteristics (e.g.,
density and resistance).
The most critical and error-prone passage was the
activity of conversion from ERM raw data into
DICOM data. In general, this is the most delicate
passage and the one where both radiologists,
engineers and other experts are requested to cooperate
and coordinate their work and competences. As a
general lesson from our experience, we may report
that costs and efforts were considered affordable and
the exploitation of the cheapest printer (the MakerBot
one) did not compromise the quality of the work and
the satisfaction of both the patient and the clinicians
in manipulating the 3DP bones.
4 A DIDIY FRAMEWORK
The DiDIY project (http://www.didiy.eu/) defines
DiDIY as human-centered phenomenon
characterized by the diffusion of:
• a mindset among individuals: the “DiDIYers”;
• a set of activities enacted by DiDIYers: the
“DiDIYing”.
The latter activities are intended as pragmatically
translating in a context the abstraction of mindset of
an individual and, as a consequence, natively
overcoming the level of analysis of the single
individual. In DiDIY digital technology is an
“enabler”, but the very existence of DiDIY does not
depends on the presence of digital technology, as its
core properties are human-centric, thus related to
individuals’ mindsets and activities.
In short, according to this approach an individual
can be defined as a DiDIYer when, due to her
mindset: (i) she uses to “do things” on her own that
had been previously carried out by experts or
specialized companies (this aspect deals with the
traditional notion of Do-It-Yourself, or “DIY”), and
(ii) these “things” could not be “done” without digital
technology (“Di”DIY).
Under this premise, an operational definition
which enables the identification of DIDIY activities
is the following:
a) a DiDIYer, i.e., certain organizational roles
b) carries out on their own certain activities,
c) by exploiting certain digital technologies;
d) possibly exploiting the knowledge sharing within
a certain knowledge community (Cabitza et al.
2014c)
According to this definition and to our
preliminary research, we instantiate its four
dimensions in the medical domain, as follows:
DiDIYers: are the healthcare professional whose
skills are those of a digital craftsman. This role can be
played for example by doctors, surgeons, nurses,
technical clinicians (e.g., radiographers). In particular
our research focused on two main roles and activities:
the Radiologist, in her diagnostic and prognostic
activities, who runs examinations with proper
technologies and acts directly or highlights to her
colleagues actions to be taken, based on all the
medical information gathered during the analysis
More Time for the Doing, Having Made the Thinking - 3D Printing for Knowledge Circulation in Healthcare
295

of examinations results. State-of-the-art
information are bi-dimensional representations
(axial, coronal and sagittal planes) of the
analyzed anatomical parts or, at last, 3D
visualizations available thanks to 3D dashboards
provided by the ultimate diagnostic tools.
Whenever there are strong interpretation
misalignments of diagnostic examinations, for
example in case of congenital deformities, the
radiologist joins the surgeon (or her
collaborators) in order to analyze the
examination together, so as to reconcile meaning
and proceed the activity with the aid of a complex
however complete set of information;
the Surgeon, in her therapeutic activities, who
applies her surgical specialty methodologies. She
needs to collect the most part of information
before taking decisions and actions that are
neither diagnostic nor prognostic, hence they are
not at all repeatable. For this reason, the surgeon
needs the support from her colleagues, and in
most complex scenarios, even from other
healthcare professionals, such as for example
clinical engineers, other specialists, consultants
and so on.
Technology: is the elective tool of the DiDIY-er to
improve her activities or to face them in innovative
ways and under unusual perspectives. The
technologies involved in the healthcare domain
encompass: 3D datasets from physical objects
through scanning and diagnostic image acquisition;
2D visualizations of physical objects, through
DICOM files or CAD software; 3D manufacturing of
physical objects. In this sense, 3DP amplifies the
capabilities to go from bits to atoms back and forth
(blinded reference).
Activity: is the (knowledge) practice of the DiDIYer;
it is the daily routine that a professional carries out
alone or as a part of a community. The use of
technology should improve and innovate her daily
activities, so that a virtuous circle can be triggered,
and creativity and new skills can emerge and flow
freely, also thanks to her network community.
Medical practice is peculiarly “practical”, and
tangible and intangible information concur to define
the logic of “knowing how to do it” or DIY. In the
words of an orthopaedic surgeon (Malik et al., 2015)
that we adapted to emphasize the importance of tools
that improve the situated awareness and support more
critical scenarios during surgical operations:
“Having the chance to perform on a 3D model all
the necessary steps preoperatively, valuable time is
saved and surgeons have more time to focus on the
present moments: you have more time for the doing,
having made the thinking”
Community: can be offline, online or both, and
encompasses individuals who are either
contextualized in physical meetings and workshops
or in the virtual spaces of an online environment. In
communities people can find inspiration for new
ways of doing things while exchanging and sharing
knowledge. The community is the vehicle to share
experiences, results and open new ways and
directions to practical problems.
In the medical domain, cross-fertilization has a
pivotal role: during conferences or pre-operative
meetings, surgeon together with radiologists,
biomedical engineers, and other medical team
members may share heterogeneous knowledge and
competences and find a synergy to solve problems,
propose solutions or simply hypothesize new
healthcare trajectories and allies.
5 CONCLUSIONS
In this paper we have investigated how healthcare
professionals may be helped in sharing knowledge
and cooperating thanks to 3DP resources and 3D
objects, seen as either intangible and tangible
(respectively) Knowledge Artifacts (KAs).
In so doing, we have illustrated as the printing of
virtual 3D objects into tangible material artifacts does
not regard only the transition “from bits to atoms”
(Bull & Garofalo, 2009). Rather it also pertains the
transition from digital objects to “matters of fact”
(i.e., physical objects) and eventually to “matters of
concerns” (Latour 2004), that is things, to discuss
both about and around. The physical availability in
an increasing number of work settings of this kind of
things, through a making-oriented and DIY attitude,
creates opportunities also for other kinds of social
making, like sense making and decision making (in
our case, among health practitioners) and enrich these
activities in ways that are still to be explored.
In particular, we illustrated this phenomenon in
two vignettes taken from our observational study:
1) the orthopaedic surgeon talks with the patient,
who is going to undergo a surgery for the replacement
of his knee joints, by showing him details of his injury
and the necessary operation details with the aid of a
custom-made 3D anatomical model. This KA helps
the patient “see” his situation more clearly and take a
more informed decision on the surgical operation;
2) the orthopaedic surgeon talks with his team
members to discuss the details of the surgical
KITA 2016 - 2nd International Workshop on the design, development and use of Knowledge IT Artifacts in professional communities and
aggregations. Knowledge Artifacts as resources in the maker and DIY communities
296

operation and to test in advance the prosthesis against
the patient-specific 3D reproduction of the knee joint
articulation (the KA). In so doing, a relevant amount
of time can be saved for settings and measurements,
and the KA can help reduce the operation time,
improve safety and lead to better outcome.
As purported in the specialist literature and
confirmed in our observational studies, 3DP has got a
potential to change the work of surgeons, both in
regard to surgery planning, and in educational
activities with novices, as well as in the
communication with the patient. In this sense,
medical 3DP objects represent a new toolkit of KAs
available to prosthetic practitioners, as these artifacts
allow for the patient-specific configuration and
setting of the main parameters and measurements that
can be tested before the surgery takes place. In this
light, further research should be aimed at
understanding whether prototype replicas can help
practitioners replace the more traditional “diagnostics
by imaging” paradigm with a complementary, if not
alternative, one: a “diagnostics by volumes”, which
would enable the emergence of new knowledge
circulation practices and habits.
ACKNOWLEDGEMENTS
This article has been developed under the DiDIY
project funded from the European Union’s Horizon
2020 research and innovation programme under grant
agreement No 644344.
REFERENCES
Auricchio, F., & Marconi, S., 2016. 3D printing: clinical
applications in orthopaedics and traumatology. EFORT
Open Reviews, 1(5), 121-127.
Bull, G., & Garofalo, J., 2009. Personal Fabrication
Systems: From Bits to Atoms. Learning & Leading with
Technology, 36(7), 10-12.
Cabitza, F., Colombo, G., & Simone, C. 2013. Leveraging
underspecification in knowledge artifacts to foster
collaborative activities in professional communities. Int
J Hum-Comput St, 71(1), 24-45.
Cabitza, F., Fogli, D., & Locoro, A., 2016. Virtual patients
for knowledge sharing and clinical practice training: a
gamified approach. GALA 2015, LNCS, 329-335.
Cabitza, F., Locoro, A., 2014a. Made with knowledge:
Disentangling the IT Knowledge Artifact by a
qualitative literature review. In KMIS 2014, 64-75.
Cabitza, F., Cerroni, A., Locoro, A., Simone, C. 2014b. The
knowledge-stream model: A comprehensive model for
knowledge circulation in communities of
knowledgeable practitioners. In KMIS 2014, 367-374.
Cabitza, F., Cerroni, A., & Simone, C. 2014c. Knowledge
artifacts within knowing communities to foster
collective knowledge. In AVI 2014, ACM, 391-394.
Cuendet, S., Bumbacher, E., and Dillenbourg, P. 2012.
Tangible vs. virtual representations: when tangibles
benefit the training of spatial skills. In NordiCHI '12.
de Mel, A., 2016. Three-dimensional printing and the
surgeon. British Journal of Surgery, 103(7), 786-788.
DiDIY, D3.1-1.2, Deliverable Doc no 3.1 of the DiDIY
project, Sept 2016.
Dourish, P. 2001. Where the Action is: The Foundations of
Embodied Interaction. MIT Press, Cambridge, USA.
Eltorai, A. E., Nguyen, E., & Daniels, A. H. 2015. Three-
Dimensional Printing in Orthopedic Surgery.
Orthopedics, 38(11), 684-687.
Fedorov A., Beichel R., Kalpathy-Cramer J., … Kikinis R.,
2012. 3D Slicer as an Image Computing Platform for
the Quantitative Imaging Network. Magnetic
Resonance Imaging, 30(9), 1323-41.
Greenhalgh, T., & Wieringa, S., 2011. Is it time to drop the
‘knowledge translation’metaphor? A critical literature
review. Journal of the Royal Society of Medicine,
104(12), 501-509.
Hornecker, E. & Buur, J. 2006. Getting a grip on tangible
interaction: a framework on physical space and social
interaction. In: Procs of ACM CHI 2006. 437-446.
Lakoff, G., & Johnson, M. 1999. Philosophy in the flesh:
The embodied mind and its challenge to western
thought. Basic books.
Latour, B., 2004. Why has critique run out of steam? From
matters of fact to matters of concern. Critical inquiry
30(2), 225-248.
Malik, H. H., Darwood, A., … & Baskaradas, A., 2015.
Three-dimensional printing in surgery: a review of
current surgical applications. Journal of Surgical
Research, 199(2), 512-522.
McMenamin, P. G., Quayle, M. R., McHenry, C. R., &
Adams, J. W., 2014. The production of anatomical
teaching resources using three-dimensional (3D)
printing technology. Anatomical sciences education,
7(6), 479-486.
Mitsouras, D., Liacouras, P., ... & Ho, V. B., 2015. Medical
3D printing for the radiologist. RadioGraphics, 35(7),
1965-1988.
Mok, S. W., Nizak, R., ... & Malda, J., 2016. From the
printer: Potential of three-dimensional printing for
orthopaedic applications. Journal of Orthopaedic
Translation, 6, 42-49.
Pernin, J. P., Michau, F., Mandran, N., & Mariais, C. 2012.
ScenLRPG, a board game for the collaborative design
of GBL scenarios: qualitative analysis of an
experiment. In Proc. of the 6th European Conference
on Games Based Learning, 384-392.
Popescu, D., Laptoiu, D., Hadar, A., Ilie, C., & Pârvu, C.,
2015. Workflow for additive manufacturing of an
individualized surgical template. Procs in
Manufacturing Systems, 10(3), 131-140.
More Time for the Doing, Having Made the Thinking - 3D Printing for Knowledge Circulation in Healthcare
297

Rengier, F., Mehndiratta, A., von Tengg-Kobligk, H.,
Zechmann, C. M., Unterhinninghofen, R., Kauczor, H.
U., & Giesel, F. L., 2010. 3D printing based on imaging
data: review of medical applications. International
journal of computer assisted radiology and surgery,
5(4), 335-341.
Rybarczyk, Y. and Fonseca, J. 2011. Tangible interface for
a rehabilitation of comprehension in aphasic patients.
In: Association for the Advancement of Assistive
Technology in Europe.
Starosolski, Z. A., Kan, J. H., Rosenfeld, S. D.,
Krishnamurthy, R., & Annapragada, A., 2014.
Application of 3-D printing (rapid prototyping) for
creating physical models of pediatric orthopaedic
disorders. Pediatric radiology, 44(2), 216-221.
Varela, F.J., Rosch, E., Thomson, E. 1991. The Embodied
Mind. MIT Press.
Vrasidas, C. (2000). Constructivism versus objectivism:
Implications for interaction, course design, and
evaluation in distance education. IJET, 6(4), 339-362.
KITA 2016 - 2nd International Workshop on the design, development and use of Knowledge IT Artifacts in professional communities and
aggregations. Knowledge Artifacts as resources in the maker and DIY communities
298
