
Excellent Potential of Geometric Brownian Motion (GBM) as
a Random Process Model for Level of Drowsiness Signals
Pouyan Ebrahimbabaie and Jacques G. Verly
Department of Electrical Engineering and Computer Science, University of Li
`
ege, Li
`
ege, Belgium
Keywords:
Drowsiness, Somnolence, Random Process, Geometric Brownian Motion, GBM, Driving, Psychomotor
Vigilance Test, PVT.
Abstract:
We show that Geometric Brownian Motion (GBM) appears to be an excellent choice of random process model
to describe mathematically the real-life signals that represent the evolution with time of the level of drowsiness
(LoD) of an individual, such as a driver. We collected data from thirty (30) healthy participants, who each
underwent three tests (either driving in a simulator or performing Psychomotor Vigilance Tests) at successive
levels of sleep deprivation. During each test, the LoD was produced by a photooculography (POG) based
device designed and built by our team. We so obtained a total of 90 LoD signals. For each, we applied
statistical methods to determine whether a GBM was a valid model for it. All 90 signals passed statistical tests
of normality and independency, meaning that each can be modeled by GBM, thereby showing the excellent
potential of GBM as a random process model for LoD signals. This finding could lead to the development
of a number of innovative means for predicting the evolution of the LoD and the occurrence of related events
beyond the present moment. The resulting technology should help reduce the number of accidents due to
drowsy driving.
1 INTRODUCTION
The drowsy state is an intermediate state between
alert wakefulness and sleep as defined electro-
physiologically by the pattern of brain waves (EEG),
eye movements (EOG), and muscle activity (EMG)
(Johns, 2001, p. 5). Drowsiness is a major cause of
accidents in many areas of human activity (whether
personal or professional), and transportation is prob-
ably the single most important source of drowsiness-
related accidents. For example, one third (1/3) of fatal
accidents on highways in France are reported due to
the driver falling asleep at the wheel (Association des
Soci
´
et
´
es Franc¸aises d’Autoroutes, 2010).
It is thus paramount to monitor the level of drowsi-
ness (LoD) of a driver and to devise in-car safety sys-
tems that can help prevent accidents due to drowsi-
ness. This implies the development and use of drowsi-
ness monitoring systems. We focus here on systems
that monitor the physiological state of the subject, e.g.
by using images of an eye.
All systems that we know of can establish a
present LoD based on such data obtained up to the
present time. But, if the LoD at the present time
reaches a critical level, it may be too late to save a
driver’s life. Therefore, there is an imperative need
to estimate how the LoD will evolve past the present
time, and to make LoD-related predictions. To the
best of our knowledge, the field of predicting the evo-
lution of drowsiness and of related parameters in the
future is essentially completely unexplored. The first
investigations of this question appear to be (Ebrahim-
babaie and Verly, 2016a; Ebrahimbabaie and Verly,
2016b; Ebrahimbabaie and Verly, 2016c).
A conventional strategy for predicting future val-
ues of a signal is to describe this signal via a model.
Since the evolution of the LoD is inherently random,
one must treat each real-life ”LoD signal” as a real-
ization of a random process (RP).
The RP process models that often come to mind
in a wide variety of applications are AR, ARMA,
and ARIMA models, where ”AR” stands for ”autore-
gressive”, ”MA” for ”moving average”, and ”I” for
”integrated” (Manolakis et al., 2005; Hayes, 1996).
In (Ebrahimbabaie and Verly, 2016a; Ebrahimbabaie
and Verly, 2016b; Ebrahimbabaie and Verly, 2016c),
we examined the application of such models to a
PERCLOS signal and to an LoD signal, and we
found that these signals could be properly modeled
by AR(I)MA RP models. However, we also pointed
Ebrahimbabaie, P. and Verly, J.
Excellent Potential of Geometric Brownian Motion (GBM) as a Random Process Model for Level of Drowsiness Signals.
DOI: 10.5220/0006545101050112
In Proceedings of the 11th International Joint Conference on Biomedical Engineer ing Systems and Technologies (BIOSTEC 2018) - Volume 4: BIOSIGNALS, pages 105-112
ISBN: 978-989-758-279-0
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
105

out that these models are quite heavy to deal with, in
part because, for each, the order is unknown and the
parameters are unknown and numerous.
Our search for better RP models in the context of
drowsiness monitoring led us to examine the Geomet-
ric Brownian Motion (GBM) RP model (Jeanblanc
et al., 2009). A preliminary investigation indicated
that the GBM RP model could be very appropriate for
the signals found in the context of drowsiness moni-
toring, such as a PERCLOS signal and an LoD signal.
The main goal of the present paper is to describe
the work that we did with real subjects in several
states of sleep deprivation to establish that the GBM
RP model appears to be a good, promising choice of
RP model to describe the LoD signals produced by a
specific, validated, POG-based drowsiness quantifica-
tion instrument, at least based on the data we had.
The GBM RP model lies at the heart of this paper.
We now give a brief definition of what a GBM RP is.
As one shall see, the notion of a GBM RP is rooted in
significantly advanced mathematics (Jeanblanc et al.,
2009).
A continuous-time RP X(t) is said to be a GBM,
or GBM - i.e. to follow a GBM (RP) model - if it
satisfies the stochastic differential equation (SDE)
dX(t)
X(t)
= µdt + σdW (t), (1)
where µ is a fixed, real-valued parameter, σ a fixed,
real, positive parameter, and W (t) a Weiner (random)
process also called Brownian Motion (BM) (Jean-
blanc et al., 2009).
The left side of Equation 1 is the relative incre-
ment of X(t) in the period of time [t,t + dt], i.e.
(X(t + dt) − X(t))/X(t). The right side of this equa-
tion shows that this relative increment has a determin-
istic linear trend µdt that is disturbed by a random
noise term σdW (t). The constant µ is the so-called
“drift” (or “mean rate of return” in financial mathe-
matics), and σ is the so-called “volatility”.
Recall that the goal of this paper is to show that
GBM is a good RP model for real-life LoD signals.
2 METHODS
We used data from two laboratory-based studies, re-
ferred to here as Study A and Study B. Both stud-
ies used the same overall (experimental) protocol,
and they differed only by (1) the groups of partici-
pants/subjects who took part in each study, and (2)
the nature of the tests/tasks that each participant was
asked to submit to in each study.
2.1 Participants
We recorded experimental data from N = 30 healthy
participants aged 19-33. Study A contributed 13 sub-
jects (mean age: 23.7; 7 men, 6 women), and Study B
17 subjects (mean age: 22.7; 8 men, 9 women).
2.2 Protocol
In each of the two studies (A and B), the correspond-
ing participants were each asked to submit to three
successive, time-separated test sessions in different
sleep-deprivation conditions over two days. During
each test session, the LoD signal of each participant
was produced using a drowsiness monitoring system
designed, built, and validated by our team.
In Study A, each test session consisted in driving
in a high-fidelity driving simulator; the three succes-
sive sessions had durations of 45, 45, and 60 minutes.
In Study B, each test session consisted in performing
a Psychomotor Vigilance Test (PVT); the three suc-
cessive sessions all had durations of 10 minutes.
For ease of explanation, the overall two-day ex-
periment for each participant (for either type of test)
can be viewed as the succession of Night 1, Day 1,
Night 2, and Day 2, and as consisting of three succes-
sive test sessions. Figure 1 provides an illustration of
the overall protocol used for both studies. On Night
1, the participant slept at home and was asked to re-
port the number of hours of sleep using a sleep diary
(mean ± standard deviation for all participants is 7.57
± 0.8 h of sleep, range 6.5–9.0 h). Then, the partic-
ipant was not allowed to sleep from the time he/she
woke up on Day 1 until the end of the study (12:00
noon on Day 2). (All times are in 24 h notation.) At
8:00 on Day 1, the participant arrived at our labora-
tory and submitted to the first test session, between
8:00 and 10:00. The participant was then free to leave
the laboratory to carry out his/her normal activities
but was equipped with an actigraph (either Actiwatch
2 or Philips Respironics) in order to check that he/she
had not slept while away. The participant came back
to our laboratory at 20:30 on Day 1. On Night 2,
the participant submitted to the second test session
between 2:00 and 4:00 and, after breakfast on Day
2, he/she submitted to the third test session between
11:00 and 13:00 (and after at least 28 hours of sleep
deprivation). At the end of the study, the participant
was sent back home. From noon on Day 1 until the
end of third test session, the participant was asked not
to consume any stimulant (coffee, tea, etc.). This pro-
tocol was approved by the Ethics Committee of the
University of Li
`
ege (Franc¸ois et al., 2016).
BIOSIGNALS 2018 - 11th International Conference on Bio-inspired Systems and Signal Processing
106
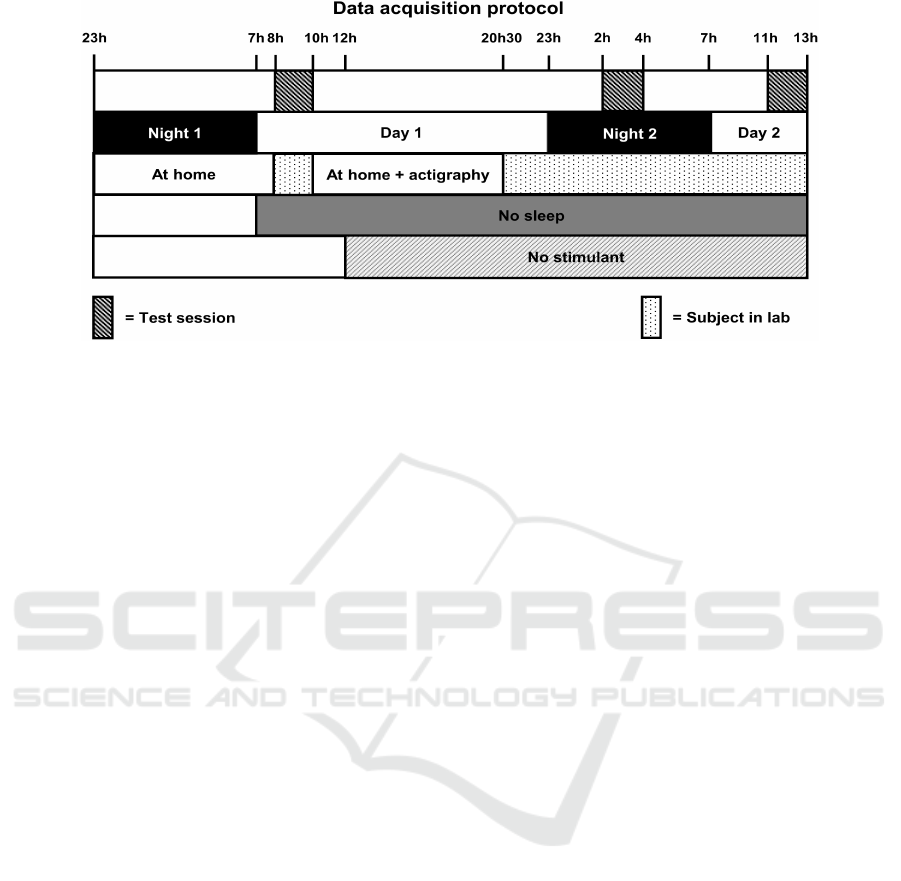
Figure 1: Graphical overview of overall protocol common to both studies, i.e. for Study A (driving in a simulator) and Study
B (PVT). The successive five lines show: (1) when each participant had to submit to a test; (2) the succession of nights and
days; (3) the presence at home or in our lab; (4) the period of sleep deprivation; (5) the period of stimulant deprivation.
2.3 Measurements
We setup our drowsiness monitoring system to pro-
duce one sample of the LoD every 20 sec in Study A
and every 5 sec in Study B. One reason for consid-
ering two distinct sampling intervals was to examine
whether the conclusion concerning the nature of the
underlying RP for LoD signals would dependent on
the value of the sampling interval. One other reason
for decreasing the sampling interval to 5 sec - thereby
producing LoD signals with 4 times as many samples
- was to provide more data for the statistical analysis.
2.4 Instruments
Our team designed, built, and validated (Franc¸ois
et al., 2016; Franc¸ois et al., 2014) a fully automatic
drowsiness monitoring system based on the physio-
logical state of a person. The system consists in a pair
of specially-made eyeglasses linked to a computer via
a cable. The eyeglasses contain a controlled source
of illumination in the infrared (IR) and a high-speed
camera sensitive in the IR.
The algorithms running on the computer use ocu-
lar parameters extracted from images of the eye (i.e.
POG) to determine, periodically in time, an LoD on
a numerical scale from 0 to 10, with 0 corresponding
to ”very awake” (or ”very vigilant”) and 10 to ”very
drowsy” (Franc¸ois et al., 2016).
2.5 Data Analysis
The sequence of LoD values produced by our drowsi-
ness monitoring system during each particular test
session is referred to here as a signal. The signals
recorded during Study A and Study B are further de-
scribed in the next section. In an actual operational
situation, the signal would be the sequence of samples
produced during the time the operator has the glasses
on, such as during a long drive.
Consider a given, real-life signal - such as the one
just described - that is considered to be one realiza-
tion of a RP. Here, we describe the methodology that
is typically used to determine whether the GBM RP
model is a valid model for this real-life signal.
Before describing this methodology, we introduce
some key concepts. For ease of explanation, it is use-
ful to treat a RP as a sequence of random variables
(RVs), thus ordered in time. However, rather than
considering these RVs, one works here with the re-
lated log-ratio (LR) RVs. The LR RV at some time
index n is defined as the natural logarithm of the ratio
of the RV at n and the RV at n - 1. The collection of
LR RVs constitutes a new RP, called here the LR RP.
(Note that the number of RVs in the LR RP is neces-
sarily one unit less that in the original RP.) Of course,
in practice, we (only) have one realization of the orig-
inal RP, and thus one realization of the LR RP, and,
consequently, one realization of each original RV or
LR RV. While all theoretical developments must be
done in terms of RPs and RVs, the methodology only
uses the single available realization of the original RP
and that of the corresponding LR RP, as well as of
their corresponding RVs.
At the theoretical level, if the original RP is a
GBM RP, then one can show that the LR RP is char-
acterized by the following pair of properties: (1) all
LR RVs are individually characterized by a normal
(i.e. Gaussian) PDF, and the PDFs of all these RVs
are identical (thus with the same mean and standard
deviation); (2) any two distinct LR RVs are indepen-
Excellent Potential of Geometric Brownian Motion (GBM) as a Random Process Model for Level of Drowsiness Signals
107

dent in the usual statistical sense, meaning that their
joint (2D) PDF factorizes (Brandimarte, 2014).
At the methodology level, one must determine
whether both of the above properties (or conditions)
are verified. The difficulty - which is typical in the
type of approach used here - is that the theory deals
with all possible realizations, while the methodology
has only access to a single one, i.e. the observed sig-
nal. The methodology must thus do its best with a sin-
gle signal/realization to establish one or more proper-
ties that pertain to all possible realizations. In short,
the methodology must replace considerations across
a statistical ensemble by considerations across time.
Below, we simply describe the methodology, and we
do not attempt to justify it in terms of the theory.
In light of the above discussion, there are thus
two conditions to be verified on the signal/realization
available to establish whether this realization can be
modelled by a GBM RP. We refer to these condi-
tions as the ”normality condition” and the ”inde-
pendency condition”.
In order to verify normality condition, we applied,
to each signal, (1) two established graphical methods,
i.e. the quantile-quantile (QQ) plot and the histogram,
and (2) one numerical (non-graphical) method, i.e.
the Shapiro-Wilk (S-W) test.
To assess the independency condition, we looked
at the scatter plot of Log-Ratios versus time of each
signal to see whether there was any (time) correlation
between the logarithms of the ratios of successive val-
ues.
3 RESULTS
3.1 Data
Each participant in Study A and Study B contributed 3
LoD signals, with each signal corresponding to one of
the 3 tests at progressively increasing levels of sleep
deprivation. Thus, the 13 participants of Study A
(driving in a simulator) contributed 13 x 3 = 39 LoD
signals, and the 17 participants of Study B (perform-
ing PVTs) contributed 17 x 3 = 51 LoD signals.
As alluded to earlier, some characteristics of the
LoD signals produced are different for each study. In
Study A, each signal consists of 42 samples spaced by
20 seconds (for a total duration of 840 sec = 14 min),
and in Study B, each signal consists of 110 samples
spaced by 5 seconds (for a total duration of 550 sec =
9 min 10 sec). The time intervals of 20 and 5 sec are
those at which the drowsiness measurement system
was asked to produce its output samples. This should
be distinguished from the speed at which the images
of the eye were collected, i.e. 120 images/sec in both
Study A and Study B.
In summary, we have the following numbers of
LoD signals and samples:
• Study A: 13 x 3 = 39 signals; 39 x 42 = 1,638
samples;
• Study B: 17 x 3 = 51 signals; 51 x 110 = 5,610
samples
• Total for both studies: 90 signals; 7,248 samples.
Below, we illustrate the application of the methodol-
ogy (described in the Methods section) to one exam-
ple signal from Study A and to one from Study B.
These example signals, referred to as ”Signal A” and
”Signal B”, are shown in Figure 2.
3.2 Application of Methodology to
Signal A & Signal B
We present here the results of applying the methodol-
ogy to Signal A and Signal B. Specifically, we show
the results of applying the three techniques for check-
ing the normality condition (histogram, Q-Q plot, and
S-W test) and the one technique for checking the in-
dependency condition (linear regression).
3.2.1 Check of Normality Condition
Figure 3(a) shows the histogram of log-ratio sample
values - or, simply, log-ratios - for Signal A, and the
corresponding ”best-fit” normal (i.e. Gaussian) PDF,
i.e. that with the mean and standard deviation of the
log-ratios. Figure 3(b) shows the corresponding sub-
figure for Signal B.
Figure 4(a) shows the Q-Q plot of log-ratios for
Signal A, and the corresponding ”best-fit” straight
line, i.e. that minimizing the total least-square fit er-
ror. Figure 4(b) shows the corresponding subfigure
for Signal B.
Since the histogram and Q-Q plot techniques are
graphical, it is by visual inspection of the plots that
one must decide whether the normality condition is
verified or not. Through our experience based on
looking at tens of such plots in the particular context
of LoD signals, as well as at many in the literature for
other applications, we conclude with confidence that,
according to the histograms and Q-Q plots, Signal A
and Signal B both satisfy the normality condition.
The application of the S-W test with significance
level α = 0.05 leads to the following conclusions.
For Signal A: The p-value of the S-W test is 0.10.
Since it is greater than 0.05, we cannot reject the H
0
hypothesis that the log-ratio RVs have a normal (i.e.
Gaussian) PDF. Recall that this does NOT allow us
BIOSIGNALS 2018 - 11th International Conference on Bio-inspired Systems and Signal Processing
108

Figure 2: Example LoD signals from (a) Study A and (b) Study B, referred to as ”Signal A” and ”Signal B”, respectively.
Figure 3: Histograms of log-ratio sample values (or log-ratios) for (a) Signal A and (b) Signal B, and corresponding ”best-fit”
normal PDFs.
to conclude that Signal A then verifies the normality
condition.
For Signal B: The p-value of the S-W test is 0.01.
Since it is smaller than 0.05, we must reject the H
0
hypothesis. This allows us to conclude that Signal B
does not verify the normality condition according to
the present test.
The results of the three techniques (histogram, Q-
Q plot, and S-W test) lead us to the following conclu-
sions.
For Signal A: The pair of graphical tests indicates
that Signal A satisfies the normality condition, and
the S-W test does NOT allow us to say that it does
not satisfy this condition, which is the best one could
hope for in light of the two other tests.
For Signal B: The pair of graphical tests indi-
cates that Signal B satisfies the normality condition,
whereas the S-W test indicates that it does not.
While all three techniques allow us to conclude
with confidence that Signal A verifies the normality
Excellent Potential of Geometric Brownian Motion (GBM) as a Random Process Model for Level of Drowsiness Signals
109

Figure 4: Q-Q plots of log-ratio sample values (or log-ratios) for (a) Signal A and (b) Signal B, and corresponding ”best-fit”
straight lines.
condition, one cannot so easily reach a conclusion
for Signal B. However, since the graphical techniques
both show in a convincing way that Signal B verifies
the normality conditions, we made the decision to de-
clare that Signal B verifies the normality condition.
3.2.2 Check of Independency Condition
Figure 5(a) shows the plot of log-ratio sample values
(or log-ratios) for Signal A as a function of time, and
the corresponding ”best-fit”/regression straight line.
Figure 5(b) shows the corresponding subfigure for
Signal B.
Since the linear regression technique is graphical,
it is by visual inspection of the plots that one must de-
cide whether the independency condition is verified
or not. As for the histograms and Q-Q plots, through
our experience of looking at many such plots, we con-
clude with confidence - from the regression lines - that
Signal A and Signal B both verify the independency
condition.
3.2.3 Conclusion for Signal A & Signal B
Since each of Signal A and Signal B can reasonably
be said to verify both the normality condition and the
independency condition, we conclude that GBM is a
valid choice of model for each of Signal A and Signal
B.
3.3 Results for all 90 LoD Signals
We applied to all 90 LoD signals available the same
detailed analysis as the one applied above for Signal
A and Signal B.
3.3.1 Check of Normality Condition
According to the graphical techniques of histogram
and Q-Q plot, we concluded that all 90 LoD signals
from Study A and Study B verify the normality con-
dition.
According to the S-W test with significance level
α = 0.05, we reached the following conclusions.
For Study A: for each LoD signal in this study,
the H
0
hypothesis cannot be rejected. Recall that this
does NOT allow us to conclude that such signal then
verifies the normality condition.
For Study B: for each LoD signal in this study, the
H
0
hypothesis must be rejected. This allows us to con-
clude that such signal does NOT verify the normality
condition according to the present test.
Therefore, for Study A, all LoD signals verify the
normality condition according to all three techniques,
whereas, for Study B, they verify it only according to
the graphical techniques.
However, just as in the case of Signal B above,
the graphical techniques of histogram and Q-Q plot
allowed us to conclude that all LoD signals in Study
B can reasonably be said to verify the normality con-
dition.
BIOSIGNALS 2018 - 11th International Conference on Bio-inspired Systems and Signal Processing
110

Figure 5: Plots of log-ratio sample values (or log-ratios) as a function of time and of the corresponding ”best-fit” straight lines
for (a) Signal A and (b) Signal B.
In conclusion, all 90 LoD signals from Study A
and Study B can reasonably be said to verify the nor-
mality condition.
3.3.2 Check of Independency Condition
The linear regression technique allowed us to declare
that all LoD signals from Study A and Study B verify
the independency condition.
3.3.3 Conclusion for all LoD Signals from Study
A & Study B
Since each signal in Study A and in Study B can rea-
sonably be said to verify the normality condition and
the independency condition, we conclude that GBM
is a valid choice of model for each signal in Study A
and in Study B.
4 DISCUSSION
Using a carefully planned and executed protocol, and
a validated drowsiness monitoring system, we col-
lected discrete-time signals that represent the evolu-
tion of the level of drowsiness (LoD) of 30 individu-
als at three increasing levels of sleep deprivation over
three days, thus resulting in 90 validated LoD signals.
Given their nature, LoD signals must be viewed
as realizations of random processes (RPs). Predicting
the (unknown) future values of such signals, as well as
related events, based upon data available up to close
to the present time requires one to have a model of the
underlying RP.
Using appropriate statistical analysis, we have
shown that Geometric Brownian Motion (GBM) is a
valid choice of random process (RP) model for mod-
elling all 90 LoD signals, thus without a single excep-
tion.
Of course, before being sure that GBM is an ex-
cellent model for ”all” LoD signals to be encountered
in all real-life circumstances, it will be necessary to
conduct studies on more subjects and in actual opera-
tional conditions such as driving on a real road.
At the time of this writing, we are exploring the
avenues that open up in the field of drowsiness moni-
toring if/when the LoD signals are GBM.
In addition, the work reported here can provide a
strong motivation for researchers interested in mod-
elling physiological and biological processes to ex-
amine whether - starting from the physiological and
biological mechanisms involved in the evolution of
drowsiness, and using appropriate mathematical mod-
els and tools - they can possibly show that an LoD
signal should in fact naturally be a realization of an
underlying GBM RP model.
ACKNOWLEDGMENTS
We wish to thank Mrs. Cl
´
ementine Franc¸ois, from our
research team, for providing the level-of-drowsiness
signals used in this paper. She played a significant
role in their acquisition, as part of her PhD thesis
work.
Excellent Potential of Geometric Brownian Motion (GBM) as a Random Process Model for Level of Drowsiness Signals
111

REFERENCES
Association des Soci
´
et
´
es Franc¸aises d’Autoroutes
(2010). Somnolence au volant:
une
´
etude pour mieux comprendre.
http://www.autoroutes.fr/FCKeditor/UserFiles/File/
Publications/ASFA - Somnolence p-p2.pdf.
Acessed: November 19, 2016.
Brandimarte, P. (2014). Handbook in Monte Carlo Sim-
ulation: Applications in Financial Engineering, Risk
Management, and Economics. John Wiley & Sons,
New Jersey.
Ebrahimbabaie, P. and Verly, J. G. (2016a). ’Prediction of
future values of a level of drowsiness derived from im-
ages of an eye based on its past values, with applica-
tion to drowsy driving’. Paper presented to the Inter-
national Symposium on Somnolence, Vigilance, and
Safety (SomnoSafe). Brussels, Belgium. 21-23 Febru-
ary.
Ebrahimbabaie, P. and Verly, J. G. (2016b). ’Prediction
of future values of the eye PERCLOS based on its
past values, with application to drowsiness monitor-
ing’. Paper presented to the International Symposium
on Somnolence, Vigilance, and Safety (SomnoSafe).
Brussels, Belgium. 21-23 February.
Ebrahimbabaie, P. and Verly, J. G. (2016c). ’Random
process modeling of an optooculography-based level
of drowsiness, with application to drowsy driving’.
Poster presented to the Joint Meeting of the IEEE-
EMBS Benelux Chapter and the 14th Belgian Na-
tional Day on Biomedical Engineering. Brussels, Bel-
gium. 27 November.
Franc¸ois, C., Hoyoux, T., Wertz, J., and Verly, J. G. (2016).
Tests of a new drowsiness characterization and moni-
toring system based on ocular parameters. 13:174.
Franc¸ois, C., Wertz, J., and Verly, J. G. (2014). ’valida-
tion of a new automatic drowsiness quantification sys-
tem for drivers’. Paper presented to the 5th Interna-
tional Conference on Applied Human Factors and Er-
gonomics (AHFE). Krakow, Poland. 19-23 July.
Hayes, M. H. (1996). Statistical Digital Signal Processing
and Modeling. John Wiley & Sons, New York, NY.
Jeanblanc, M., Yor, M., and Chesney, M. (2009). Math-
ematical Methods for Financial Markets. Springer,
London.
Johns, M. W. (2001). Assessing the drowsiness of drivers.
Melbourne: VicRoads.
Manolakis, D. G., Ingle, V. K., and Kogan, M. S. (2005).
Statistical and Adaptive Signal Processing: Spectral
Estimation, Signal Modeling, Adaptive Filtering, and
Array Processing. Artech House, Norwood, MA.
BIOSIGNALS 2018 - 11th International Conference on Bio-inspired Systems and Signal Processing
112
