
Non-invasive Multichannel Electrostimulation of Neck Nerve
Structures for the Treatment of Patients with Anxiety Disorders
Timur Petrenko
1,2
, Mikhail Shalyagin
2
, Konstantin Retjunskiy
2
,
Vladimir Kublanov
1
and Mikhail Babich
1
1
Ural Federal University, Mira 19, Yekaterinburg, Russian Federation
2
Ural State Medical University, Repina 3, Yekaterinburg, Russian Federation
Keywords: Anxiety Disorders, Neurostimulation, Autonomic Nervous System.
Abstract: The efficiency of non-invasive multichannel neuro-electrostimulation device (‘SYMPATHOCOR-01’) for
treatment of anxiety disorders against the standard antidepressant medication is presented in article. Forty
patients from psychiatric clinic with diagnosed 'panic disorder' were treated and followed-up during six weeks.
The Hamilton (HAM-A) and Sheehan (SPRAS) anxiety scales were used to determine changes in state of
patients. Electrostimulation has helped patients quickly overcome symptoms of anxiety and better control
panic attacks. There was a significant difference in the final psychometric assessment of anxiety among
groups on the Hamilton (HAM-A) and Sheehan (SPRAS) scales almost twice.
1 INTRODUCTION
Anxiety disorder is one of the most common among
all mental disorders. According to the data of Russian
and foreign scientists panic disorder occurs in 1,5-3,0
% of the adult population, and its subthreshold forms
are diagnosed among 9-10 % of adult population in
the developed countries (NIMH, 2017; Schmidt et al.,
2003).
Contemporary neurophysiological studies have
revealed that panic disorder develops in the midst of
the increasing dysfunction of the autonomic nervous
system (ANS) (Stahl and Moore, 2013). In the
beginning, the ANS dysfunction is permanent and
subtle. Then, it intensifies and becomes a paroxysmal
one, fully defining the clinical symptoms of the panic
attack (Kar and Sarkar, 2016). If the dysfunction of
ANS stayed for a considerable time, it would cause
irreversible changes in the blood vessels walls. This,
in turn increases the risk of the vascular disorders
development, which could result in stroke or heart
attack (Kar and Sarkar, 2016). Autonomic disorders
in different countries occurs in 25-80 % of the adult
population (Schmidt et al., 1999). More than half of
these people have a risk of the paroxysmal anxiety
disorders.
Negative impact of the panic disorder on quality
of life and social adaptation defines the relevance of
the search for novel treatment approaches (Schmidt et
al., 1999). At the same time, the effectiveness of the
medicamentous approaches stays quite low
(Starcevic, 2009).
Contemporary approaches of the anxiety
disorders therapy imply psychotropic medication –
antidepressants. These drugs increase exchange of the
serotonin and other neuromediators in structures of
the central nervous system (CNS), which are
responsible for the emotions. This increases the role
of the inhibitor mechanisms in the conscious control
of the fear and anxiety emotions (Stahl and Moore,
2013).
However, the medicamentous approach is
effective only among the one third of the patients. In
most cases, the life-long drug regimen is implied,
which is accompanied by the numerous side effects.
Essentially, the medicamentous approach is just a
substitution therapy and does not treat the disorder
itself (Stahl and Moore, 2013).
Combination of the medicamentous therapy with
the psychotherapy allows to increase effectiveness up
to 50 % (Weaver et al., 2009). However, this
approach implies life-long psychotropic drug
regimen and daily psychiatrist appointments. Many
patients cannot afford such expenses. In 20 % the
disorder can become a malignant one. In that case, the
known approaches become inefficient (Stahl and
Moore, 2013).
Petrenko T., Shalyagin M., Retyunsky K., Kublanov V. and Babich M.
Non-invasive Multichannel Electrostimulation of Neck Nerve Structures for the Treatment of Patients with Anxiety Disorders.
DOI: 10.5220/0006592603450350
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Recently, the methods of neuro-electrostimulation
for treatment of the depressive and anxiety disorders
are being actively developed (White and Tavakoli,
2015). The highest effectiveness was reported for the
transcranial magnetic stimulation and invasive
stimulation of the vagus nerve (Sarkar and Cohen
Kadosh, 2016). The anti-depressive and anti-anxiety
effects are associated with the stimulation of the
brainstem nucleus and midline brain structures,
which, in turn leads to the massive emission of the
neurotransmitters and reconstructions of the neural
networks (White and Tavakoli, 2015).
In current study, we have investigated the
effectiveness of the dynamic correction of activity of
the sympathetic nervous system (DCASNS) approach
in comparison with standard medicamentous
approaches. The DCASNS approach is realized by
the medical device ‘SYMPATHOCOR-01’
(Kublanov et al., 2014).
2 NECK NERVE STRUCTURES
Centres for regulation of the life-important functions
are placed in nucleuses of the brain stem, middle
brain, the bridge, and cerebellum, and also, in the
vegetative nucleuses of the neuraxis and cerebrum.
Many of the conducting paths of these centers are
located in the neck. The neck somatic innervation is
provided by the neck neuraxis nerves that forms the
massive cervical interlacing on its back surface. The
afferent nerve fibers pass through the neuraxis back
horns and end in the sensitive nucleuses of the brain
stem and reticular formation. The reticular formation
participates in processing the sensors’ information
and, additionally, makes activating impact onto the
brain-cortex. By this way, the formation controls the
neuraxis activity.
This mechanism implements the tonus control of
the skeletal muscles and moreover, of the human
vegetative functions. The ganglia of the sympathetic
stem are placed in deep muscles of the neck. These
ganglia are formed by the nerve stems of the
vegetative ones of the neuraxis nervous offshoots.
The upper, middle, and lower (stellular) sympathetic
ganglia have multiple branches that perform
sympathetic innervation of glands, brain involucres,
and vessels of the neck, head and vertebra. The vagus
nerve is located abreast the main neck arteries. Its
ganglia are placed in the brain stem and are common
with the tong-pharyngeal nerve. They have wide
connections with the hypothalamus, rhinal system,
and reticular formation. The pair of IX and X cranial
nervous branches jointly implements para-
sympathetic innervation of the majority of human
organs. Together with branches of vagus nerve, ones
of the neck part of the sympathetic stem form several
nervous interlacings in the heart region. By this, the
vegetative regulation of the heart activity is
implemented. The nervous formations of neck area
are tightly joined with brain stem, middle brain,
cerebellum, thalamus, hypothalamus, and the large
brain cortex. Presence of these connections provides
participation of the neck nervous formations in
analysis of irritations from sensors and in regulation
of the muscle tonus, vegetative and the highest
integrative functions (Moore et al., 2013; Netter,
2014). Taking into account the mentioned facts, it is
perspective to use the neck neuraxis nervous
interlacing and the X and IX cranial nerves as a target
for electro-stimulation. It will allow one to stimulate
(through the afferent paths) the grey matter of the
brain stem. Through the reticular formation, this
action can propagate onto the thalamic structures and
the cerebrum cortex. Stimulation of the neck ganglia
of the sympathetic stem will permit to affect onto both
the vascular tonus of the brain arteries and onto the
vegetative ganglia of the neuraxis. Thus, the neuro
electro-stimulation system (under developing) is
completely able to modulate the vegetative processes
and affect onto the sensori-motor control and
cognitive functions.
3 MATERIALS AND METHODS
3.1 Multichannel
Neuro-electrostimulation Device
The group of scientists and engineers from the Ural
Federal University developed the portable corrector
of activity of the sympathetic nervous system
(‘SYMPATHOCOR-01’) is an electrical pulse
generator that delivers the spatially-distributed field
of the carefully-controlled current pulses in the neck
(Kublanov, 2008).
The device is included in the register of medical
equipment products of the Russian Federation
(registration certificate № FCR 2007/00757) and has
the Certificate of correspondence to the requirements
of the regulations GOST R 50444-92.
The spatially-distributed field of the current
pulses is formed between two multi-element
electrodes of the device. Each multi-element
electrode comprises a cluster of thirteen partial
current-conducting elements. The multi-element
electrodes are arranged on the neck into left and right
sides. In the working state, one element of one multi-
element electrode performs the role of the anode.
Elements on the other side become the cathodes. If it
is necessary, the arrangement can be reversed in
opposite direction.
Placing the multi-element electrodes on the
subject neck, the centre elements of multi-element
electrodes have to be located in projections of the
neck ganglia of the sympathetic nervous system
(Fig. 1).
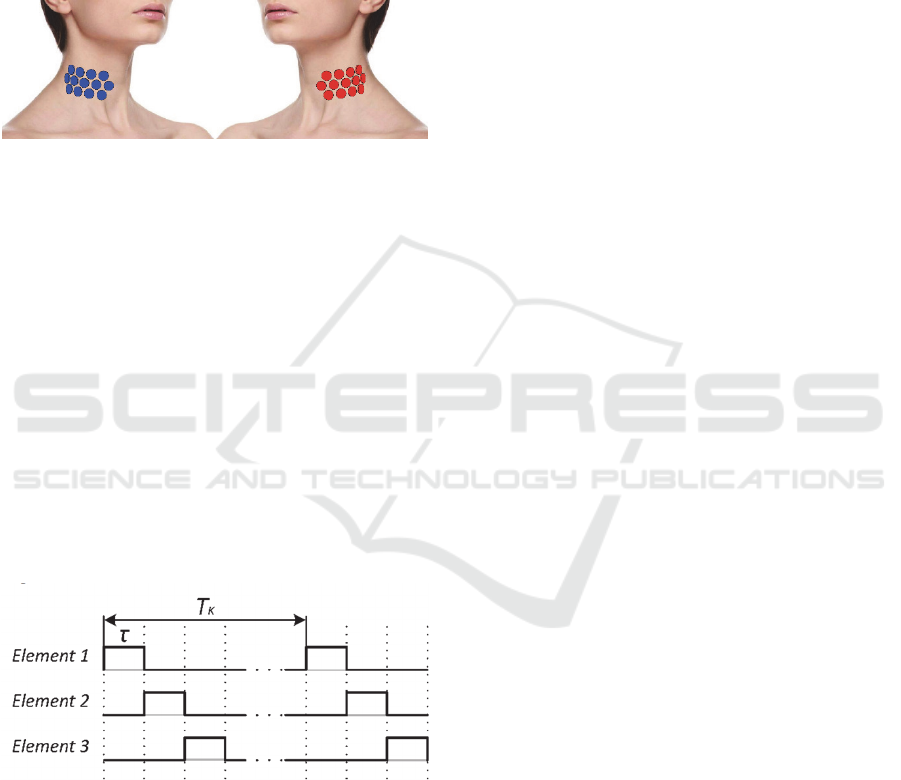
Figure 1: Scheme of the partial current-conducting
elements of the multi-element electrodes location.
Note the following basic bio-tropic characteristics
of the field: the current partial pulses duration τ is
from 15 to 60 usec. The number of partial pulses in
the period (pulse group) is 12. The frequency f of
pulses group is from 5 to 150 Hz. Pulses group period
is named as T
K
and calculated as T
K
=1/f. The cathode
elements are switched accordingly to each given rule
(for example, a pseudo-random with the clockwise or
counterclockwise direction of switching, and so on).
The used anode is set depending on the stimulation
target. The duration of the anode connection varies
from 30 seconds to several minutes and is controlled
by the doctor. The current pulses amplitude can be up
to 15 mA.
Elements connection timing diagram is shown in
Fig. 2.
Figure 2: Elements connection timing diagram.
Before starting the stimulation, the generator
connects the positive pole of the built-in current
source to the element used as the anode. During
stimulation process, the generator sequentially
switches elements used as cathodes to the negative
pole of the current source in accordance with
switching order used. Cathodes and anodes
connections are performed by the built-in multi-
channel switches.
Depending on pathogenesis of the peripheral or
central dysfunctions of the ANS, the dynamic
correction of the activity sympathetic nervous system
(DCASNS) algorithm has two different branches.
Decision of which branch should be executed is based
on nature of the ANS dysfunction. The bio-tropic
parameters of the implemented current pulse field
(the field structure, pulses amplitude, frequency, and
duration) are calculated from the analysis of the heart
rhythm variability. In particular, in the case of the
abnormal hyperactivity of sympathetic innervation, it
is necessary to block or suppress the activity of the
sympathetic nervous system. In contrast, sympathetic
innervation should be increased, if the hyperactivity
of the parasympathetic innervation is observed. In
case of central dysfunctions, the bio-tropic
parameters of the stimulation field are calculated,
based on analysis of the main activity rhythms of the
cerebral cortex and its deviation from the norm.
In clinic practice, the ‘SYMPATHOCOR-01’
device and DCASNS algorithm were efficiently
applied for treatment of various diseases including
organic and/or functional disorders of the CNS and/or
the ANS: consequences of brain trauma or stroke,
epilepsy, chronic headache, somatoform disorders,
anxiety and depressive spectrum disorders, attention-
deficit hyperactivity disorder, disorders involving
cognitive impairments (Kublanov et al., 2017).
In transistory paths of the nervous system of the
neck region, there are both myelinated fiber and non-
myelinated fiber. The rate of excitation propagation
in the myelinated fibers is significantly larger than in
the non-myelinated ones. To provide participation in
stimulation of structures of various formations, it is
necessary that the length of the partial spatially
distributed pulses is matched with the rate of
excitation propagation in the myelinated fibers, and
the length of the spatially concentrated pulses’
structure is matched with the rate of excitation
propagation in the non- myelinated ones.
Block diagram of the engineering feasibility of
multi-channel neurostimulation system is shown in
Fig. 3.
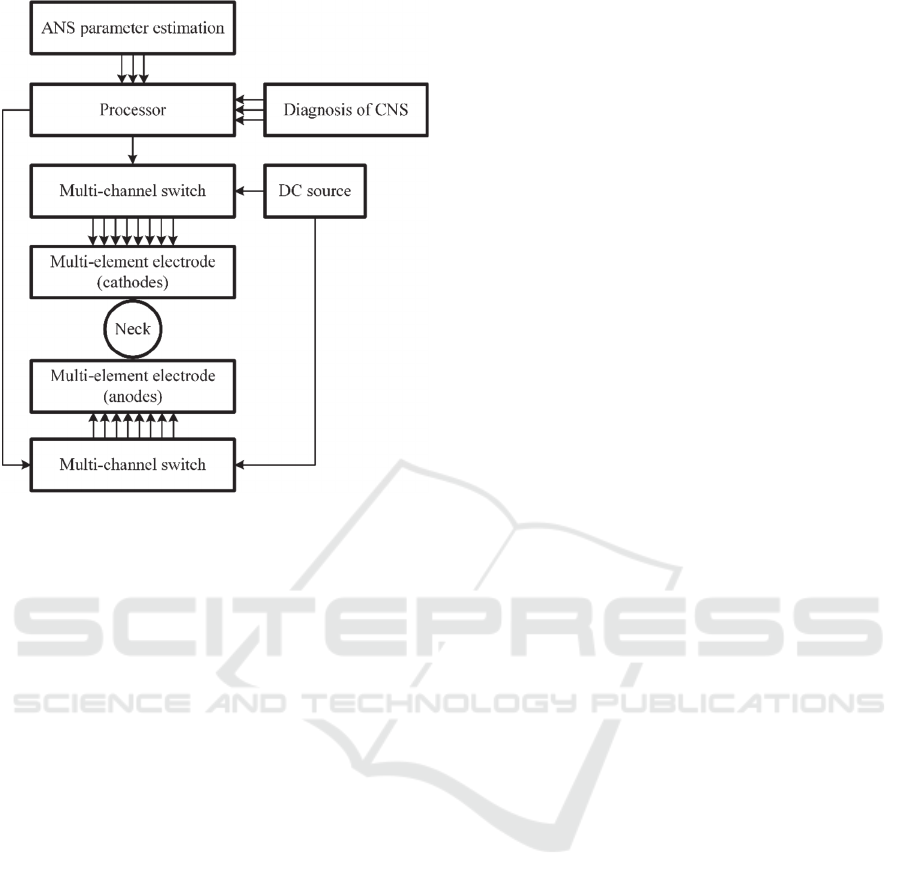
Figure 3: Block diagram of the engineering feasibility of
multi-channel neurostimulation system.
The detailed technical description of the
‘SYMPATHOCOR-01’ device and the algorithm of
the DCASNS approaches were presented in
(Kublanov, et al., 2008) and (Kublanov, et al., 2017).
3.2 Clinical Data
The study on the clinical basis of the Department of
Psychiatry at the State Medical University was
conducted. The study has an approval of the Local
Ethics committee (protocol 2 from 16.03.2007). The
study included 40 outpatients with a newly diagnosed
"panic disorder" (“ICD-10,” 2010). All participants
have signed the informed consent of participation in
the study. Among the participants, there were 20 male
and 20 female patients. Average age of the
participants was 28,5 years. On average the disorder
has lasted for 7,6 months.
The following patients were excluded from the study:
patients, having clinically significant disease,
which can prevent the therapy evaluation and
which can affect safety of the therapy;
patients, suffering from the paroxysmal anxiety
within other mental disorders (bipolar disorder,
schizophrenia disorder, eating disorder,
obsessive-compulsive disorder, dependence on
psychoactive substances);
patients, taking psycho-pharmacological
medicine prior to the study;
female patients during pregnancy and lactation.
The period of therapy and dynamic follow-up was
6 weeks for each patient. All patients were randomly
divided into two equal groups (20 patients each). In
the first group (to be referred as AD), patients
received drug therapy with antidepressant –
escitalopram, 10 mg once daily, during whole study.
In the second group (to be referred as SCR), patients
were treated by means of the device
‘SYMPATHOCOR-01’. The treatment course
consisted of daily 15-minute long procedures, for 10
days in a row. It was allowed to take a break for a
single day once during the course. After 10-day
course the patients did not take any additional
treatment for the rest of the study.
The medical examination was performed by the
psychiatric doctor in all groups of patients initially (to
be referred as T0), on the 4-th day of therapy (to be
referred as T1), and then on 7-th, 10-th, 14-th, 21-st,
28-th, 35-th and 42-nd days (to be referred as T2, T3,
T4, T5, T6, T7, T8 respectively). In order to evaluate
effectiveness of the therapy during each visit (T0-T8)
the following scales were used to estimate anxiety
level and anxiety symptoms reduction degree:
Hamilton anxiety rating scale (HAM-A)
(Hamilton, 1959);
Sheehan anxiety rating scale (SPRAS)
(Schmidt et al., 2003);
Quality-of-life index (QLI) (Katschnig, 2006);
Global clinical impression – Severity scale
(CGI-S) (Busner and Targum, 2007).
The statistical analysis was performed by the
software ‘STATISTICA 12’. Analysis of variance
was used to find the inter-group differences.
4 RESULTS
Figures 4 – 7 show that the group of patients with
neuro-electrostimulation therapy (SCR) has a faster
reduction of the anxiety symptoms, evaluated by the
generally accepted tests, in comparison with the
antidepressant therapy group (AD).
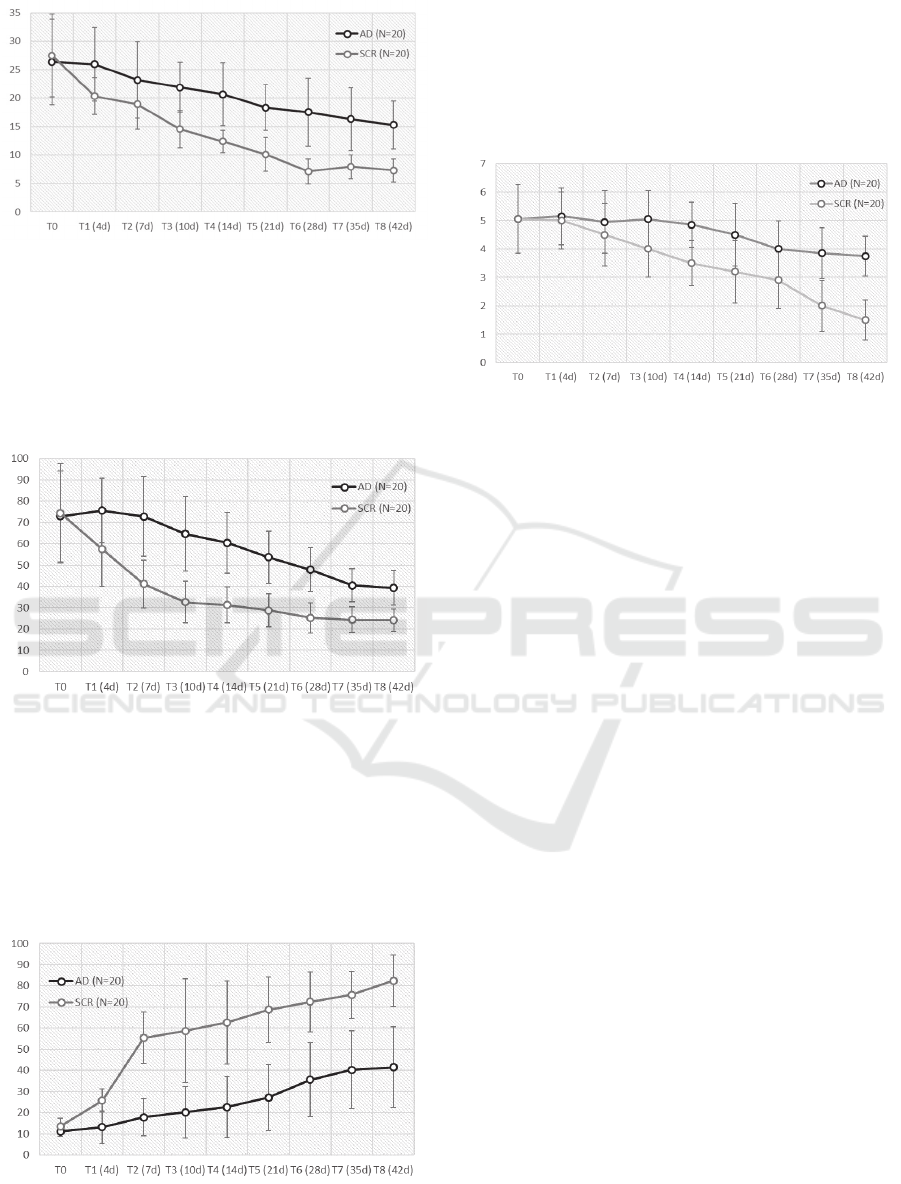
Figure 4: HAM-A dynamic for two patient’s groups.
Data on Fig. 4 shows that after 4 days of treatment
the DCASNS method has a greater effectiveness than
medicamentous approach. After three weeks, the
anxiety evaluation for patients in second group is as
for healthy people (less than 10). The DCASNS
method effect stays until the end of the study.
Figure 5: SPRAS dynamic for two patient’s groups.
Fig. 5 shows that after the first days the DCASNS
method significantly suppresses the medicamentous
treatment. After 10 days of treatment the subjective
evaluation of the patients is comparable to those of
healthy people (less than 40 points). It can be seen,
that the effect is stable until the end of the study (day
42).
Figure 6: QLI dynamic for two patient’s groups.
Plots on Fig. 6 show that patients’ evaluation of
quality of life significantly changes for two groups
after the first therapy days. After first two weeks, the
QLI evaluation for patients ingroup with neuro-
electrostimulation therapy reaches an acceptable level
(more than 60).
Figure 7: CGI-S dynamic for two patient’s groups.
Data on Fig. 7 shows that after 14 days of
treatment the DCASNS method has a greater
effectiveness than medicamentous approach. After
five weeks, the global clinical impression about
patients in second group is as for healthy people (less
than 2).
5 CONCLUSIONS
Clinical effect of the non-invasive multi-electrode
neuro-electrostimulation based on the DCASNS
approach for patients with panic disorder shows high
effectiveness in comparison with the medicamentous
therapy. This is confirmed by the psychometric study
using generally accepted scales HAM-A, SPRAS,
QLI and CGI-S. The effect is most likely associated
with the stimulation of the neurotransmitters emission
in the stem structures of the CNS and reconstruction
of the existing neural networks for most efficient
functioning. This enhances the achieved clinical
effect. However, this assumption needs confirmation
by long-term clinical studies involving technologies
of the neuroimaging. The results can be considered as
a model for treating the anxiety and depression
diseases.
In the future, we plan functional neuroimaging
study of neuroplasticity changes after proposed
neuro-electrostimulation method in patients with
anxiety and depressive disorders.
Success of this technology development depends
on interaction and collaboration of various
specialists: engineers, physicians, physiologists, and
biologists.

ACKNOWLEDGEMENTS
The work was supported by Act 211 Government of
the Russian Federation, contract № 02.A03.21.0006.
REFERENCES
Busner, J., Targum, S.D., 2007. The Clinical Global
Impressions Scale. Psychiatry Edgmont 4, 28–37.
Hamilton, M., 1959. The assessment of anxiety states by
rating. Br. J. Med. Psychol. 32, 50–55.
ICD-10 [WWW Document], 2010. URL
http://apps.who.int/classifications/icd10/browse/2010/
en (accessed 9.5.17).
Kar, S.K., Sarkar, S., 2016. Neuro-stimulation Techniques
for the Management of Anxiety Disorders: An Update.
Clin. Psychopharmacol. Neurosci. 14, 330–337.
doi:10.9758/cpn.2016.14.4.330.
Katschnig, H., 2006. Quality of life in mental disorders:
challenges for research and clinical practice. World
Psychiatry Off. J. World Psychiatr. Assoc. WPA 5, 139–
145.
Kublanov, V., Babich, M., Dolganov, A., 2017. Principles
of Organization and Control of the New
Implementation of the “SYMPATHOCOR-01” Neuro-
electrostimulation Device. Presented at the Special
Session on Neuro-electrostimulation in
Neurorehabilitation Tasks, pp. 276–282.
Kublanov, V., Shmirev, V., Shershever, A., Kazakov, Y.,
Porshnev, S., Vasilev, A., 2014. About innovative
possibilities of the device SIMPATOCOR in
management of functional disorders of vegetative and
central nervous system in neurology. Kremljovskaya
Med. 1, 60–64.
Kublanov, V.S., 2008. A hardware-software system for
diagnosis and correction of autonomic dysfunctions.
Biomed. Eng. 42, 206–212.
Moore, K.L., Agur, A.M.R., Dalley, A.F., 2013. Clinically
Oriented Anatomy, 7th edition. ed. LWW, Philadelphia.
Netter, F., 2014. Atlas of Human Anatomy: Including
Student Consult Interactive Ancillaries and Guides, 6e,
6 edition. ed. Saunders, Philadelphia, PA.
NIMH, 2017. Anxiety Disorders [WWW Document]. URL
https://www.nimh.nih.gov/health/topics/anxiety-
disorders/index.shtml (accessed 9.5.17).
Sarkar, A., Cohen Kadosh, R., 2016. Transcranial electrical
stimulation and numerical cognition. Can. J. Exp.
Psychol. Can. Psychol. Expérimentale 70, 41–58.
doi:10.1037/cep0000064.
Schmidt, N.B., Joiner, T.E., Staab, J.P., Williams, F.M.,
2003. Health perceptions and anxiety sensitivity in
patients with panic disorder. J. Psychopathol. Behav.
Assess. 25, 139–145.
Schmidt, N.B., Lerew, D.R., Jackson, R.J., 1999.
Prospective evaluation of anxiety sensitivity in the
pathogenesis of panic: replication and extension. J.
Abnorm. Psychol. 108, 532–537.
Stahl, S.M., Moore, B.A. (Eds.), 2013. Anxiety Disorders:
A Guide for Integrating Psychopharmacology and
Psychotherapy, 1 edition. ed. Routledge, New York.
Starcevic, V., 2009. Anxiety Disorders in Adults A Clinical
Guide, 2 edition. ed. Oxford University Press, Oxford ;
New York.
Weaver, F.M., Follett, K., Stern, M., Hur, K., Harris, C.,
Marks, W.J., Rothlind, J., Sagher, O., Reda, D., Moy,
C.S., Pahwa, R., Burchiel, K., Hogarth, P., Lai, E.C.,
Duda, J.E., Holloway, K., Samii, A., Horn, S.,
Bronstein, J., Stoner, G., Heemskerk, J., Huang, G.D.,
CSP 468 Study Group, 2009. Bilateral deep brain
stimulation vs best medical therapy for patients with
advanced Parkinson disease: a randomized controlled
trial. JAMA 301, 63–73. doi:10.1001/jama.2008.929.
White, D., Tavakoli, S., 2015. Repetitive transcranial
magnetic stimulation for treatment of major depressive
disorder with comorbid generalized anxiety disorder.
Ann. Clin. Psychiatry Off. J. Am. Acad. Clin.
Psychiatr. 27, 192–196.
